Tuesday Poster Session
Category: IBD
P5512 - Cronkhite-Canada Syndrome: An Inflammatory Bowel Disease Mimic
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- ME
Mario El Hayek, MD
Mayo Clinic
Jacksonville, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Mario El Hayek, MD, Sheev Zaver, MD, Yuting Huang, MD, PhD, Francis A.. Farraye, MD, MSc, MACG, Michele Lewis, MD
Mayo Clinic, Jacksonville, FL
Introduction: Cronkhite-Canada syndrome (CCS) is an extremely rare, non-hereditary polyposis syndrome, characterized by diffuse gastrointestinal hamartomatous polyps, along with ectodermal abnormalities such as alopecia, onychodystrophy, and skin hyperpigmentation. There are fewer than 500 cases reported worldwide since it was first described in 1955. We present a case of CCS initially diagnosed as Crohn’s disease highlighting its unique clinical and endoscopic features.
Case Description/
Methods: A 60-year-old African American female presented with a two-year history of watery diarrhea, abdominal pain, as well as progressive weight loss and malnutrition requiring enteral feeding. She was diagnosed as having Sjogren’s syndrome as well as Crohn’s disease and was treated with adalimumab and azathioprine following evaluation by multiple specialists but failed to improve and subsequently sought a second opinion at our institution. Her symptoms were also associated with alopecia, nail loosening, and hyperpigmentation (Image 1). Laboratory markers and stool studies were unremarkable except for marked eosinophilia. EGD revealed a normal esophagus, and markedly edematous, erythematous, and nodular gastric mucosa, most prominent in the body and antrum, along with diffuse nodular mucosa throughout the duodenum (Image 2). Sigmoidoscopy showed similar findings in the rectum and sigmoid colon. Gastric, duodenal, and colonic biopsies confirmed the presence of hamartomatous polyps.
Discussion: CCS is most commonly reported in middle-aged adults. Its etiology remains unclear, though an autoimmune component has been suggested given its association with other autoimmune conditions and increased levels of IgG-4 positive plasma cells in polyps. Recent transcriptomic analyses of CCS polyps have also shown upregulation of innate immune pathways. Early recognition is critical, as delayed diagnosis can lead to significant nutritional deficiencies and increased GI malignancy risk and morbidity. Treatment entails nutritional support as well as corticosteroids, with gradual tapering based on clinical response, and steroid-spearing agents like azathioprine. Most patients experience improvement in both gastrointestinal symptoms and ectodermal abnormalities with treatment. Our case underscores the importance of considering CCS in patients presenting with gastrointestinal symptoms suspicious for Crohn’s disease. The presence of typical dermatologic features can lead to an earlier diagnosis.

Figure: Image 1. Dermatologic Features in Cronkhite-Canada Syndrome: A) Alopecia B) Onychodystrophy and C) Hyperpigmentation
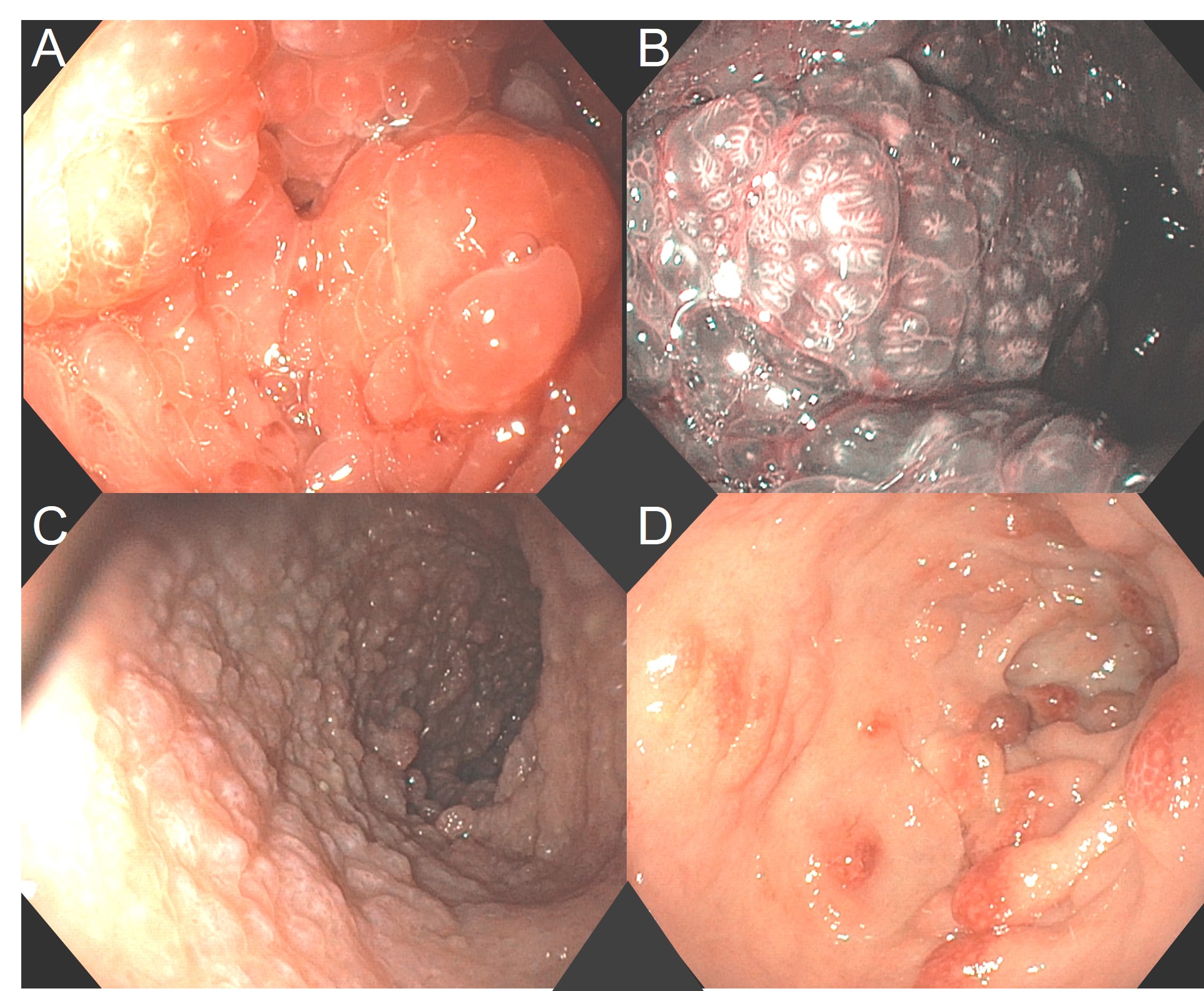
Figure: Image 2. Endoscopic findings in Cronkhite-Canada Syndrome: A) EGD image of diffuse polyposis in the stomach. B) Gastric mucosa appearance under Narrow Band Imaging (NBI). C) View in the duodenal bulb. D) Colonic polyposis seen on flexible sigmoidoscopy.
Disclosures:
Mario El Hayek indicated no relevant financial relationships.
Sheev Zaver indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Michele Lewis indicated no relevant financial relationships.
Mario El Hayek, MD, Sheev Zaver, MD, Yuting Huang, MD, PhD, Francis A.. Farraye, MD, MSc, MACG, Michele Lewis, MD. P5512 - Cronkhite-Canada Syndrome: An Inflammatory Bowel Disease Mimic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mario El Hayek, MD, Sheev Zaver, MD, Yuting Huang, MD, PhD, Francis A.. Farraye, MD, MSc, MACG, Michele Lewis, MD
Mayo Clinic, Jacksonville, FL
Introduction: Cronkhite-Canada syndrome (CCS) is an extremely rare, non-hereditary polyposis syndrome, characterized by diffuse gastrointestinal hamartomatous polyps, along with ectodermal abnormalities such as alopecia, onychodystrophy, and skin hyperpigmentation. There are fewer than 500 cases reported worldwide since it was first described in 1955. We present a case of CCS initially diagnosed as Crohn’s disease highlighting its unique clinical and endoscopic features.
Case Description/
Methods: A 60-year-old African American female presented with a two-year history of watery diarrhea, abdominal pain, as well as progressive weight loss and malnutrition requiring enteral feeding. She was diagnosed as having Sjogren’s syndrome as well as Crohn’s disease and was treated with adalimumab and azathioprine following evaluation by multiple specialists but failed to improve and subsequently sought a second opinion at our institution. Her symptoms were also associated with alopecia, nail loosening, and hyperpigmentation (Image 1). Laboratory markers and stool studies were unremarkable except for marked eosinophilia. EGD revealed a normal esophagus, and markedly edematous, erythematous, and nodular gastric mucosa, most prominent in the body and antrum, along with diffuse nodular mucosa throughout the duodenum (Image 2). Sigmoidoscopy showed similar findings in the rectum and sigmoid colon. Gastric, duodenal, and colonic biopsies confirmed the presence of hamartomatous polyps.
Discussion: CCS is most commonly reported in middle-aged adults. Its etiology remains unclear, though an autoimmune component has been suggested given its association with other autoimmune conditions and increased levels of IgG-4 positive plasma cells in polyps. Recent transcriptomic analyses of CCS polyps have also shown upregulation of innate immune pathways. Early recognition is critical, as delayed diagnosis can lead to significant nutritional deficiencies and increased GI malignancy risk and morbidity. Treatment entails nutritional support as well as corticosteroids, with gradual tapering based on clinical response, and steroid-spearing agents like azathioprine. Most patients experience improvement in both gastrointestinal symptoms and ectodermal abnormalities with treatment. Our case underscores the importance of considering CCS in patients presenting with gastrointestinal symptoms suspicious for Crohn’s disease. The presence of typical dermatologic features can lead to an earlier diagnosis.

Figure: Image 1. Dermatologic Features in Cronkhite-Canada Syndrome: A) Alopecia B) Onychodystrophy and C) Hyperpigmentation
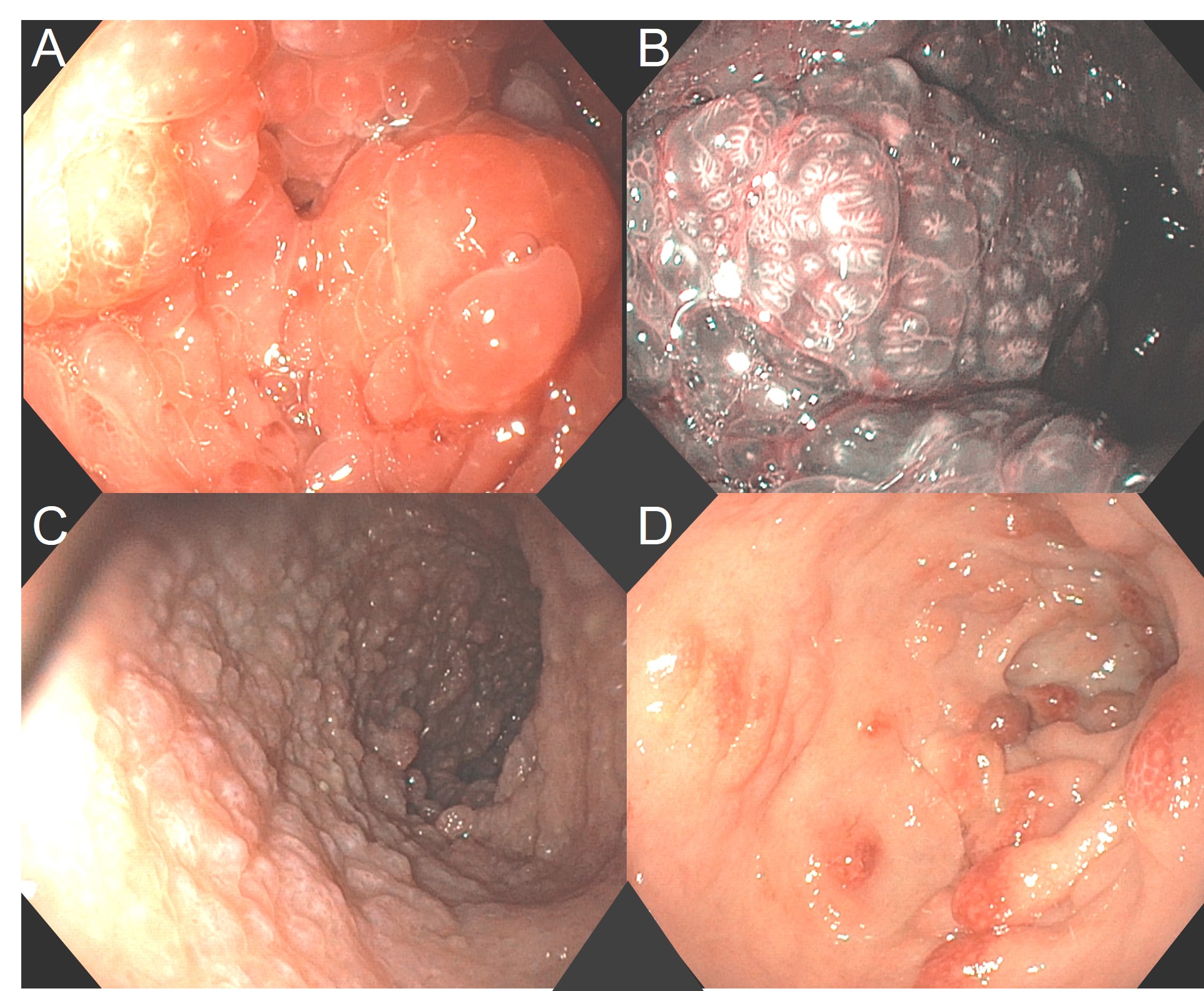
Figure: Image 2. Endoscopic findings in Cronkhite-Canada Syndrome: A) EGD image of diffuse polyposis in the stomach. B) Gastric mucosa appearance under Narrow Band Imaging (NBI). C) View in the duodenal bulb. D) Colonic polyposis seen on flexible sigmoidoscopy.
Disclosures:
Mario El Hayek indicated no relevant financial relationships.
Sheev Zaver indicated no relevant financial relationships.
Yuting Huang indicated no relevant financial relationships.
Francis Farraye: Astellas – Advisory Committee/Board Member. Avalo – Advisory Committee/Board Member. Bausch – Advisory Committee/Board Member. BMS – Advisory Committee/Board Member. Braintree Labs – Advisory Committee/Board Member. Fresenius Kabi – Advisory Committee/Board Member. GI Reviewers – Independent Contractor. IBD Educational Group – Independent Contractor. Iterative Health – Advisory Committee/Board Member, Stock Options. Janssen – Advisory Committee/Board Member. Lilly – DSMB. Pfizer – Advisory Committee/Board Member. Pharmacosmos – Advisory Committee/Board Member. Sandoz – Advisory Committee/Board Member. Viatris – Advisory Committee/Board Member.
Michele Lewis indicated no relevant financial relationships.
Mario El Hayek, MD, Sheev Zaver, MD, Yuting Huang, MD, PhD, Francis A.. Farraye, MD, MSc, MACG, Michele Lewis, MD. P5512 - Cronkhite-Canada Syndrome: An Inflammatory Bowel Disease Mimic, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

