Tuesday Poster Session
Category: IBD
P5467 - Necrotizing Enterocolitis in Infancy Is Associated with Increased Risk for Developing Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JD
Judy Daboul, MD
The Ohio State University Wexner Medical Center
Columbus, OH
Presenting Author(s)
Judy Daboul, MD1, Antonio Alvarez Castaneda, MD1, Melica Nikahd, MS2, Adeeti Chiplunker, MD1
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Columbus, OH
Introduction: Necrotizing enterocolitis (NEC) is a devastating neonatal gastrointestinal condition presenting in the earliest days of life. Enhanced toll-like receptor 4 (TLR-4) expression results in intestinal barrier dysfunction and inflammation and has been linked to developing NEC. Inflammatory bowel disease (IBD) is also characterized by intestinal barrier dysfunction and inflammation and hyper-expression of TLR-4. This study aims to determine if NEC is a risk factor for the development of IBD later in life.
Methods: The MarketScan insurance claims database identified patients with NEC and NEC with IBD using ICD-10 codes. Additional data was used to create a matched cohort of IBD patients without a history of NEC and control for multiple factors to identify if there were any differences in IBD phenotype, distribution, surgical interventions, and treatment modalities. A p-value of < 0.01 was considered significant.
Results: 8,258 patients (49.1% male) were included. 1,859 patients (55.5% male) had history of NEC. NEC patients had a significantly higher prevalence of developing IBD compared to the control (2.3% vs 0.2%, p< 0.001), Table 1. After controlling for tobacco use, antibiotic use, region of residence, super-rurality, sex, and year of birth, NEC patients were 14.8 times more likely to develop IBD than the control (95% CI: 7.4-29.6; p < 0.001) Figure 1. The rate of occurrence of IBD at any point during the study period was 9.7 times higher in the NEC group than the control group (95% CI: 4.9, 19.5; p< 0.001). There were increased overall abdominal surgeries in IBD patients with NEC, particularly small bowel resection (31% vs 0%, p = 0.034), and a significantly increased number of patients with a concurrent diagnosis of short bowel syndrome in IBD patients with NEC compared to IBD controls (42.9% vs 0%, p < 0.01), likely the result of initial treatment for NEC. Due to the limitations of the dataset, differences in IBD specific treatments in IBD-NEC patients versus IBD patients was not statistically significant.
Discussion: NEC is associated with increased prevalence of developing IBD later in life. A high proportion of patients can have a concurrent diagnosis of short bowel syndrome. It is unclear whether other factors such as early antibiotics, which may have contributed to NEC development and altered the gut microbiome and intestinal barrier, are contributing in part to this increase. More research needs to be done to elucidate the mechanisms connecting these different processes.
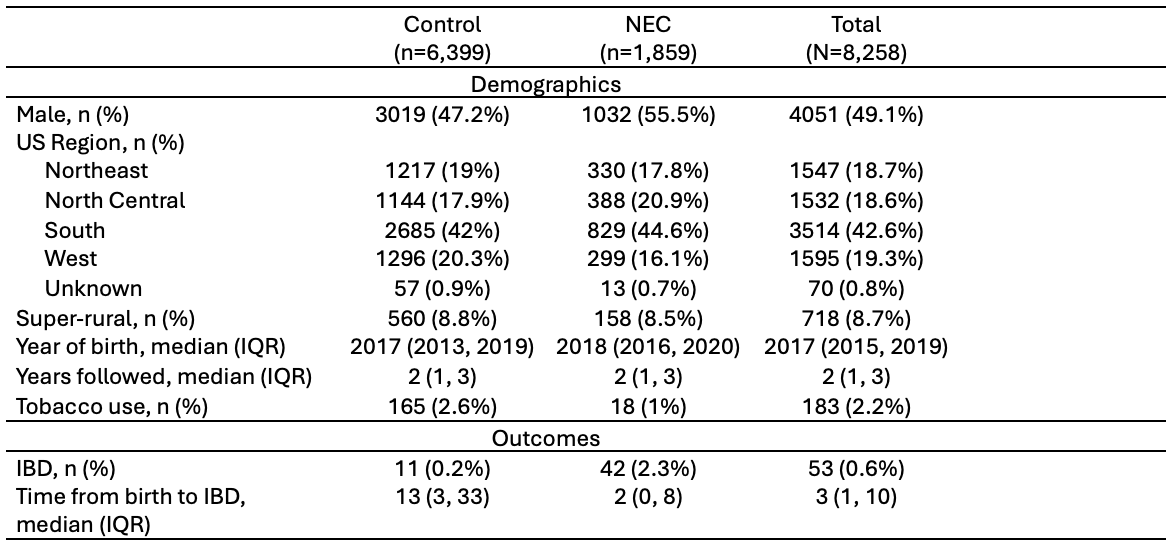
Figure: Matched cohort descriptives; NEC patients were matched to at most 10 controls on year of birth, US region of residence, sex, super-rurality, tobacco use, and length of time followed during the study period
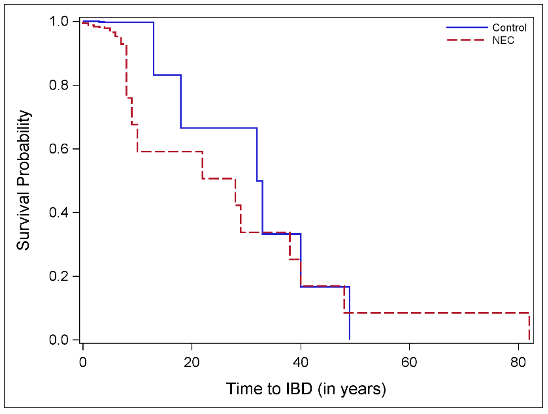
Figure: Kaplan-Meier curve of time to IBD stratified by NEC
Disclosures:
Judy Daboul indicated no relevant financial relationships.
Antonio Alvarez Castaneda indicated no relevant financial relationships.
Melica Nikahd indicated no relevant financial relationships.
Adeeti Chiplunker: Ironwood Pharmaceuticals – Advisory Committee/Board Member.
Judy Daboul, MD1, Antonio Alvarez Castaneda, MD1, Melica Nikahd, MS2, Adeeti Chiplunker, MD1. P5467 - Necrotizing Enterocolitis in Infancy Is Associated with Increased Risk for Developing Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1The Ohio State University Wexner Medical Center, Columbus, OH; 2The Ohio State University, Columbus, OH
Introduction: Necrotizing enterocolitis (NEC) is a devastating neonatal gastrointestinal condition presenting in the earliest days of life. Enhanced toll-like receptor 4 (TLR-4) expression results in intestinal barrier dysfunction and inflammation and has been linked to developing NEC. Inflammatory bowel disease (IBD) is also characterized by intestinal barrier dysfunction and inflammation and hyper-expression of TLR-4. This study aims to determine if NEC is a risk factor for the development of IBD later in life.
Methods: The MarketScan insurance claims database identified patients with NEC and NEC with IBD using ICD-10 codes. Additional data was used to create a matched cohort of IBD patients without a history of NEC and control for multiple factors to identify if there were any differences in IBD phenotype, distribution, surgical interventions, and treatment modalities. A p-value of < 0.01 was considered significant.
Results: 8,258 patients (49.1% male) were included. 1,859 patients (55.5% male) had history of NEC. NEC patients had a significantly higher prevalence of developing IBD compared to the control (2.3% vs 0.2%, p< 0.001), Table 1. After controlling for tobacco use, antibiotic use, region of residence, super-rurality, sex, and year of birth, NEC patients were 14.8 times more likely to develop IBD than the control (95% CI: 7.4-29.6; p < 0.001) Figure 1. The rate of occurrence of IBD at any point during the study period was 9.7 times higher in the NEC group than the control group (95% CI: 4.9, 19.5; p< 0.001). There were increased overall abdominal surgeries in IBD patients with NEC, particularly small bowel resection (31% vs 0%, p = 0.034), and a significantly increased number of patients with a concurrent diagnosis of short bowel syndrome in IBD patients with NEC compared to IBD controls (42.9% vs 0%, p < 0.01), likely the result of initial treatment for NEC. Due to the limitations of the dataset, differences in IBD specific treatments in IBD-NEC patients versus IBD patients was not statistically significant.
Discussion: NEC is associated with increased prevalence of developing IBD later in life. A high proportion of patients can have a concurrent diagnosis of short bowel syndrome. It is unclear whether other factors such as early antibiotics, which may have contributed to NEC development and altered the gut microbiome and intestinal barrier, are contributing in part to this increase. More research needs to be done to elucidate the mechanisms connecting these different processes.
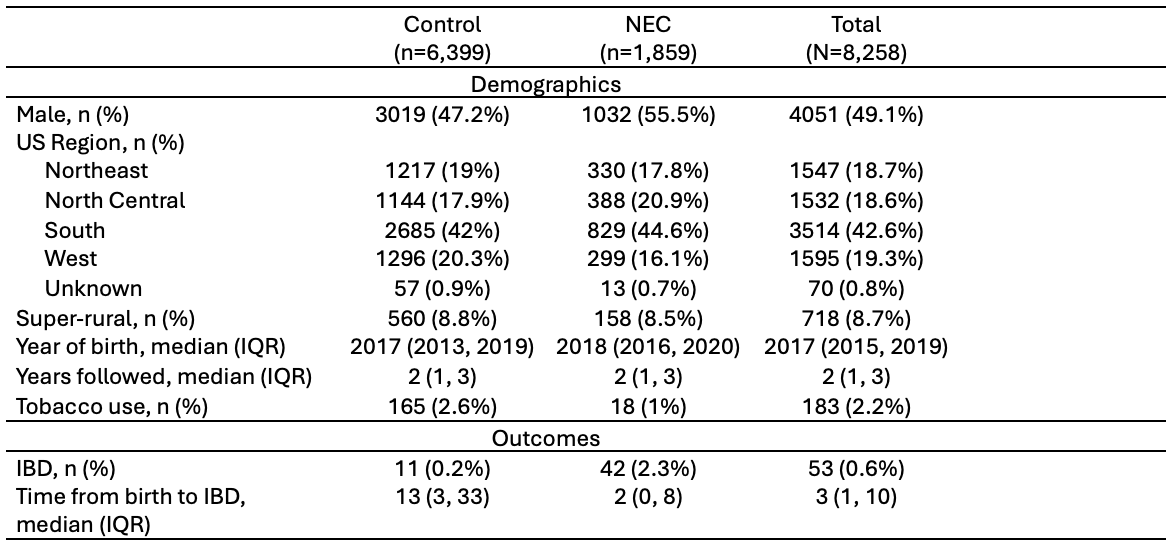
Figure: Matched cohort descriptives; NEC patients were matched to at most 10 controls on year of birth, US region of residence, sex, super-rurality, tobacco use, and length of time followed during the study period
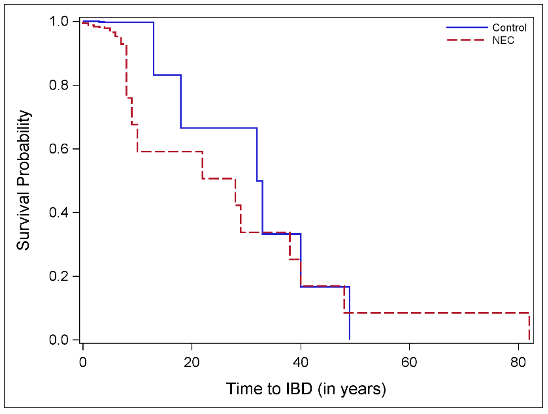
Figure: Kaplan-Meier curve of time to IBD stratified by NEC
Disclosures:
Judy Daboul indicated no relevant financial relationships.
Antonio Alvarez Castaneda indicated no relevant financial relationships.
Melica Nikahd indicated no relevant financial relationships.
Adeeti Chiplunker: Ironwood Pharmaceuticals – Advisory Committee/Board Member.
Judy Daboul, MD1, Antonio Alvarez Castaneda, MD1, Melica Nikahd, MS2, Adeeti Chiplunker, MD1. P5467 - Necrotizing Enterocolitis in Infancy Is Associated with Increased Risk for Developing Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
