Tuesday Poster Session
Category: IBD
P5449 - Association of Body Mass Index and GLP-1 in Outcomes in Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Regis Lee, DO
HCA Healthcare Riverside Community Hospital
Riverside, CA
Presenting Author(s)
Regis Lee, DO1, Fadi Totah, DO2, Eric H. Choi, MD, FACG1
1HCA Healthcare Riverside Community Hospital, Riverside, CA; 2Riverside Community Hospital, Riverside, CA
Introduction: GLP-1 receptor agonists are commonly prescribed for diabetes and obesity, two prevalent comorbidities in individuals with inflammatory bowel disease (IBD). However, data on their safety and impact on IBD-related complications remain limited. This study evaluates the association between GLP-1 agonist use and the incidence of IBD complications in lean and non-lean patients.
Methods: Utilizing the TriNetX research database, which includes data across 148 healthcare organization, this study uses ICD-10 codes to identify lean patients (BMI ≤ 24.9) (CD w/ GLP: 1,180; CD w/o GLP: 142,106; UC w/GLP: 1,402; UC w/o GLP: 143,250) and non-lean (BMI ≥ 25) (CD w/GLP: 5,257; CD w/o GLP: 171,076; UC w/GLP: 7,016; UC w/o GLP: 196,480) with a diagnosis of Crohn’s disease (CD) or Ulcerative Colitis (UC) which was then divided by the presence of a GLP-1 agonist. A propensity score matching (PSM) system and cox proportional hazards model was used to determine if the presence of a GLP-1 agonist affected the incidence of anal fissure, anal fistula, intestinal abscess, intestinal obstruction (IO), gastrointestinal bleeds (GIB), certain extraintestinal manifestations (EIM), perforation, megacolon, hospitalization and mortality within a 5-year period.
Results: In lean CD patients, GLP-1 use was associated with a statistically significant reduction of complications including IO, GIB, hospitalization, and mortality (p< 0.05). In non-lean CD patients, GLP-1 use similarly correlated with a statistically significant reduction of complications including IO, hospitalization, and mortality (p< 0.05). In lean UC patients, GLP-1 use was associated with a statistically significant decreased risk of GIB, hospitalization, and mortality (p< 0.05). In non-lean UC patients, GLP-1 use was associated with a statistically significant reduction of complications, including intestinal abscess, anal fistula, GIB, perforation, hospitalization, and mortality (p< 0.05). Although osteoarthritis and anal fistula resulted in p-values < 0.05 in CD patients, the confidence intervals did not suggest a statistically significant effect of GLP-1 use. Lastly, no differences were observed in the incidence of EIMs or megacolon.
Discussion: GLP-1 agonist use was associated with reduced rates of select IBD complications and mortality in both lean and non-lean IBD patients. While the protective mechanism remains unclear, these findings highlight the need for prospective studies to explore GLP-1’s therapeutic role in IBD management.
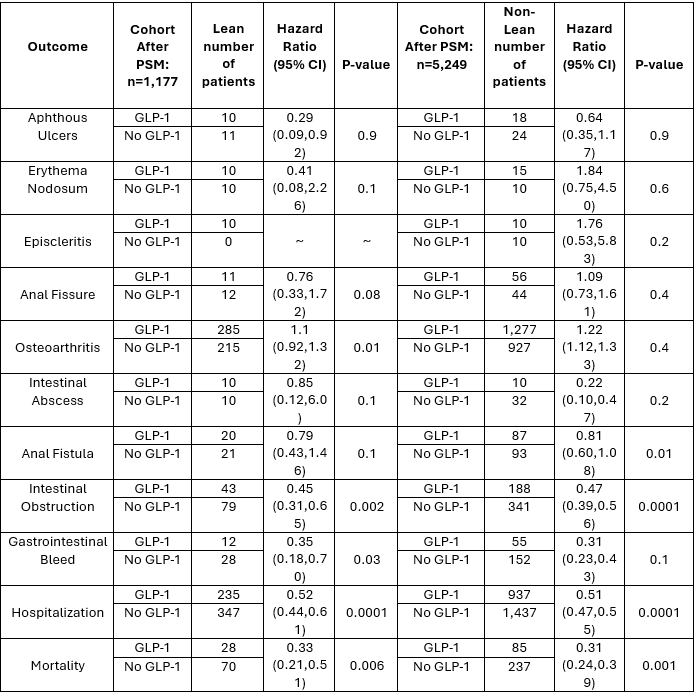
Figure: 5-year outcomes in lean and non-lean patients with Crohn's Disease with and without GLP-1 agonists.
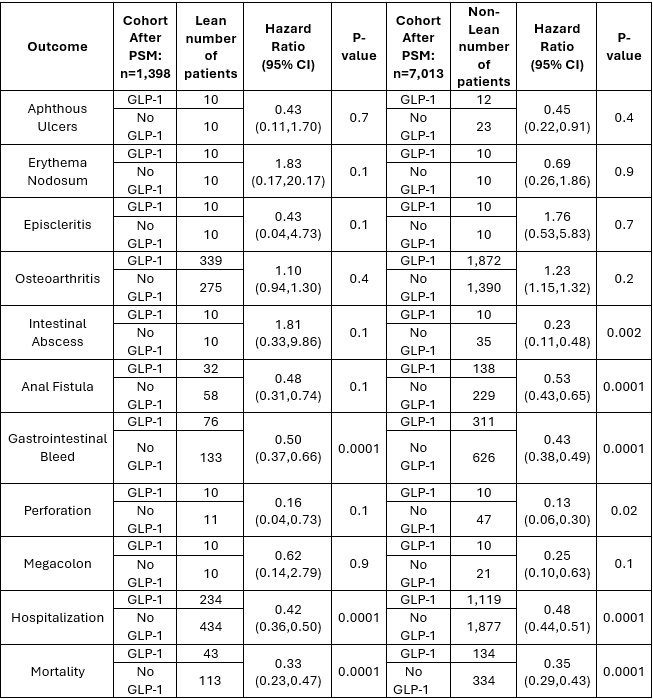
Figure: 5-year outcomes in lean and non-lean patients with Ulcerative Colitis with and without GLP-1 agonists.
Disclosures:
Regis Lee indicated no relevant financial relationships.
Fadi Totah indicated no relevant financial relationships.
Eric H. Choi indicated no relevant financial relationships.
Regis Lee, DO1, Fadi Totah, DO2, Eric H. Choi, MD, FACG1. P5449 - Association of Body Mass Index and GLP-1 in Outcomes in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1HCA Healthcare Riverside Community Hospital, Riverside, CA; 2Riverside Community Hospital, Riverside, CA
Introduction: GLP-1 receptor agonists are commonly prescribed for diabetes and obesity, two prevalent comorbidities in individuals with inflammatory bowel disease (IBD). However, data on their safety and impact on IBD-related complications remain limited. This study evaluates the association between GLP-1 agonist use and the incidence of IBD complications in lean and non-lean patients.
Methods: Utilizing the TriNetX research database, which includes data across 148 healthcare organization, this study uses ICD-10 codes to identify lean patients (BMI ≤ 24.9) (CD w/ GLP: 1,180; CD w/o GLP: 142,106; UC w/GLP: 1,402; UC w/o GLP: 143,250) and non-lean (BMI ≥ 25) (CD w/GLP: 5,257; CD w/o GLP: 171,076; UC w/GLP: 7,016; UC w/o GLP: 196,480) with a diagnosis of Crohn’s disease (CD) or Ulcerative Colitis (UC) which was then divided by the presence of a GLP-1 agonist. A propensity score matching (PSM) system and cox proportional hazards model was used to determine if the presence of a GLP-1 agonist affected the incidence of anal fissure, anal fistula, intestinal abscess, intestinal obstruction (IO), gastrointestinal bleeds (GIB), certain extraintestinal manifestations (EIM), perforation, megacolon, hospitalization and mortality within a 5-year period.
Results: In lean CD patients, GLP-1 use was associated with a statistically significant reduction of complications including IO, GIB, hospitalization, and mortality (p< 0.05). In non-lean CD patients, GLP-1 use similarly correlated with a statistically significant reduction of complications including IO, hospitalization, and mortality (p< 0.05). In lean UC patients, GLP-1 use was associated with a statistically significant decreased risk of GIB, hospitalization, and mortality (p< 0.05). In non-lean UC patients, GLP-1 use was associated with a statistically significant reduction of complications, including intestinal abscess, anal fistula, GIB, perforation, hospitalization, and mortality (p< 0.05). Although osteoarthritis and anal fistula resulted in p-values < 0.05 in CD patients, the confidence intervals did not suggest a statistically significant effect of GLP-1 use. Lastly, no differences were observed in the incidence of EIMs or megacolon.
Discussion: GLP-1 agonist use was associated with reduced rates of select IBD complications and mortality in both lean and non-lean IBD patients. While the protective mechanism remains unclear, these findings highlight the need for prospective studies to explore GLP-1’s therapeutic role in IBD management.
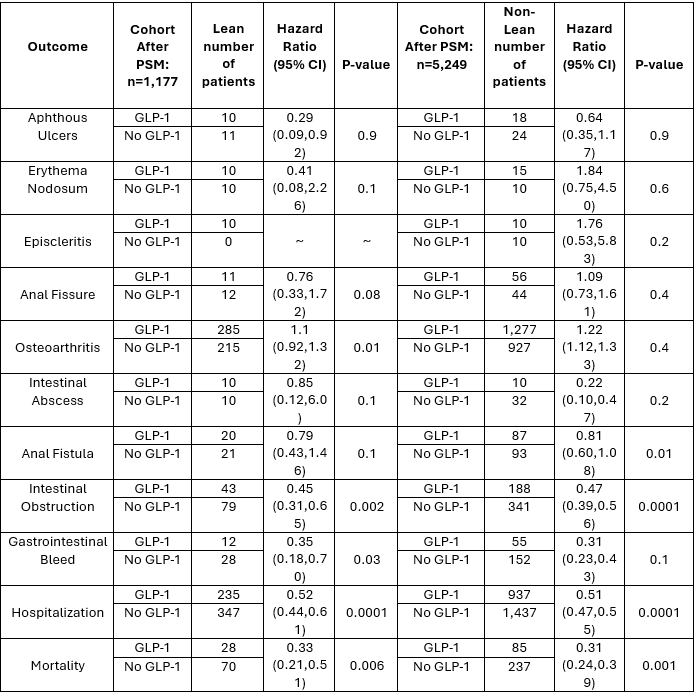
Figure: 5-year outcomes in lean and non-lean patients with Crohn's Disease with and without GLP-1 agonists.
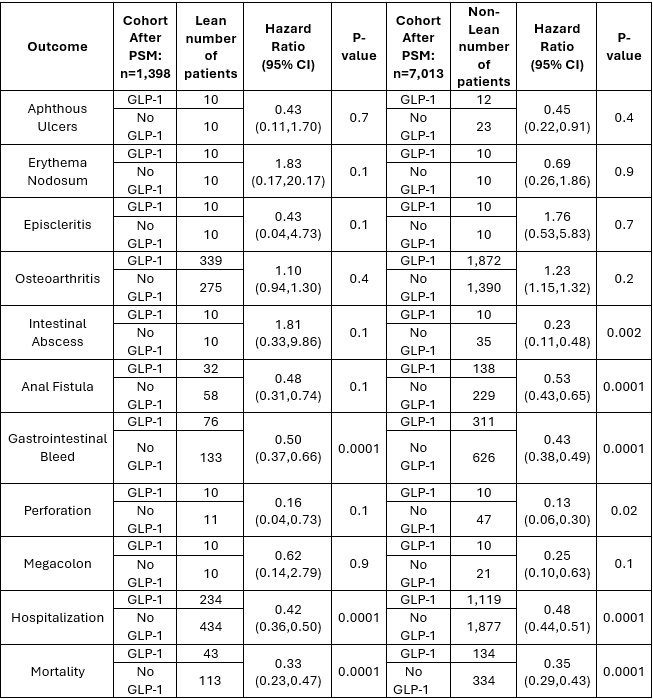
Figure: 5-year outcomes in lean and non-lean patients with Ulcerative Colitis with and without GLP-1 agonists.
Disclosures:
Regis Lee indicated no relevant financial relationships.
Fadi Totah indicated no relevant financial relationships.
Eric H. Choi indicated no relevant financial relationships.
Regis Lee, DO1, Fadi Totah, DO2, Eric H. Choi, MD, FACG1. P5449 - Association of Body Mass Index and GLP-1 in Outcomes in Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
