Tuesday Poster Session
Category: IBD
P5448 - Assessment of Sociodemographic Factors and Outcomes of Ulcerative Colitis Hospitalizations: A Large Population-Based Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Laura Sahyoun, MD
Weill Cornell Medicine
New York, NY
Presenting Author(s)
Laura Sahyoun, MD1, Darrick Li, MD, PhD2, Badr Al Bawardy, MD3
1Weill Cornell Medicine, New York, NY; 2Yale School of Medicine, Waterford, CT; 3Yale New Haven Hospital, New Haven, USA; King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia, New Haven, CT
Introduction: Up to 25% of patients with ulcerative colitis (UC) will require hospitalization. Impact of sociodemographic factors on UC hospitalizations have not been fully explored. We aimed to assess the impact of sociodemographic factors on UC hospitalization outcomes and on rates of rescue medical therapy and colectomy using a large real-world observational cohort.
Methods: This is a retrospective study using the Vizient Clinical Database from 1/1/2016-12/31/2023. Patients hospitalized for UC were identified using ICD-10 codes. Primary outcome was the rate of inpatient colectomy. Subgroup analysis was performed on those who received rescue medical therapy, which was defined as at least 1 dose of either infliximab, cyclosporine, tacrolimus, upadacitinib or tofacitinib while hospitalized. Statistical significance was calculated using Pearson’s χ2 test for categorical variables and t-test for quantitative variables. Multivariable logistic regression was used to identify covariates associated with inpatient colectomy. A p-value < 0.05 was deemed statistically significant.
Results: A total of 43,377 patients were analyzed, of whom 17.9% (n=7747) underwent inpatient colectomy. Patients who underwent inpatient colectomy were more likely to be younger, male (57.3%), non-Hispanic white, have private insurance and be admitted at a teaching hospital (p< 0.001) (Table 1). In multivariable regression analysis, all factors assessed were independently associated with risk of colectomy.
Rescue medical therapy was reported in 15% (n=6085). Of those, 11.5% (n=697) underwent inpatient colectomy. Those who underwent colectomy were more likely to be male (p< 0.001), white (p=0.03), non-Hispanic (p=0.019), and have higher Elixhauser co-morbidity score (p< 0.001). Having private insurance (p=0.001) and being hospitalized at a larger hospital (p=0.003) or teaching hospital (p< 0.001) was associated with inpatient colectomy (Table 2). In multivariable regression analysis, female sex (OR 0.73, p< 0.001), non-white race (OR 0.77, p=0.013), and non-private insurance (OR 0.83, p=0.04) were associated with lower risk of colectomy. Higher comorbidity index (OR 1.21, p< 0.001) and teaching hospitals (OR 1.92, p< 0.001) were associated with higher risk of colectomy.
Discussion: Inpatient colectomy during a UC admission was more common among males, non-Hispanic whites, those with commercial/private insurance and admitted to a large or teaching hospital. Further studies to assess risk factors for inpatient colectomy are warranted.
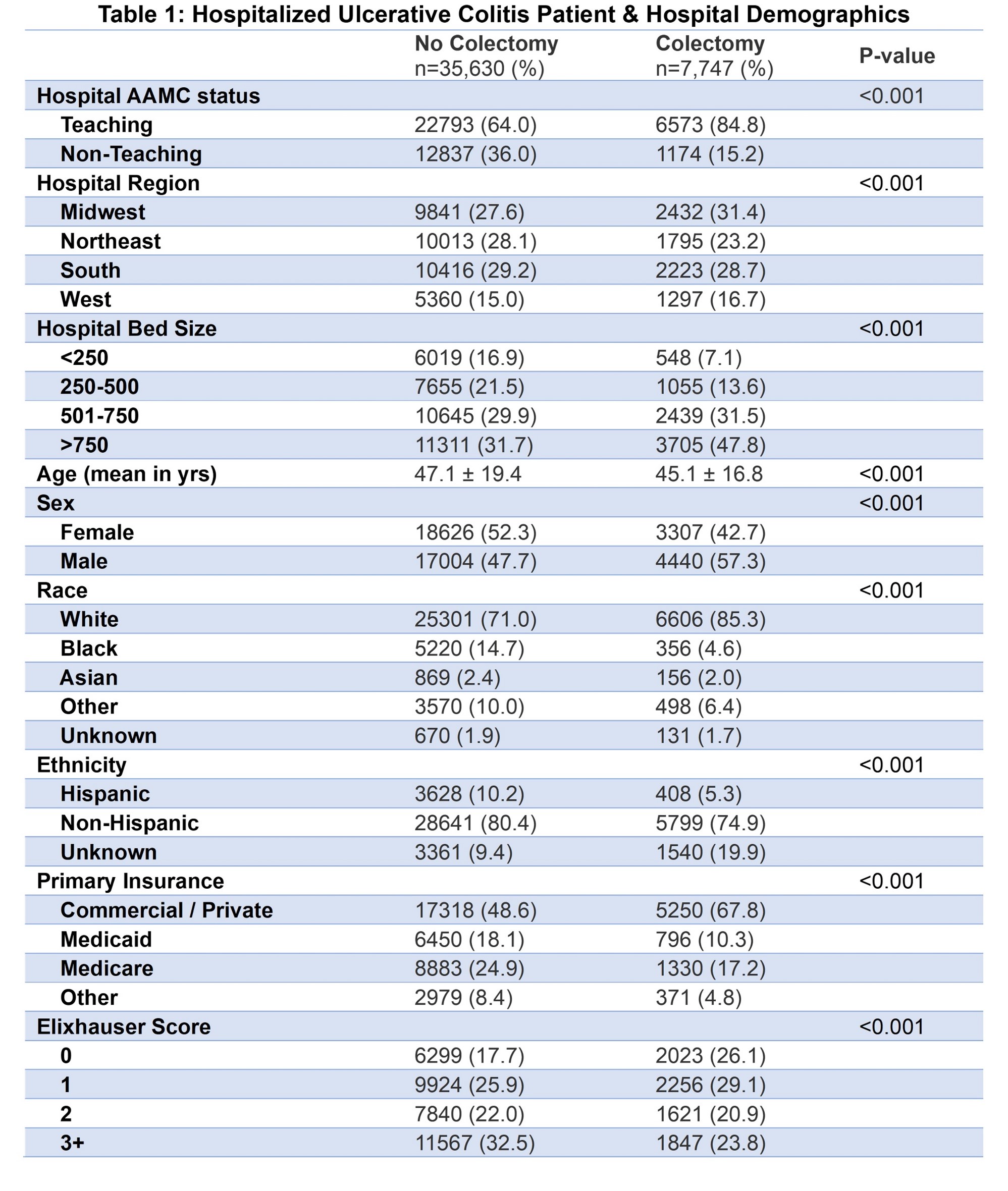
Figure: Table 1
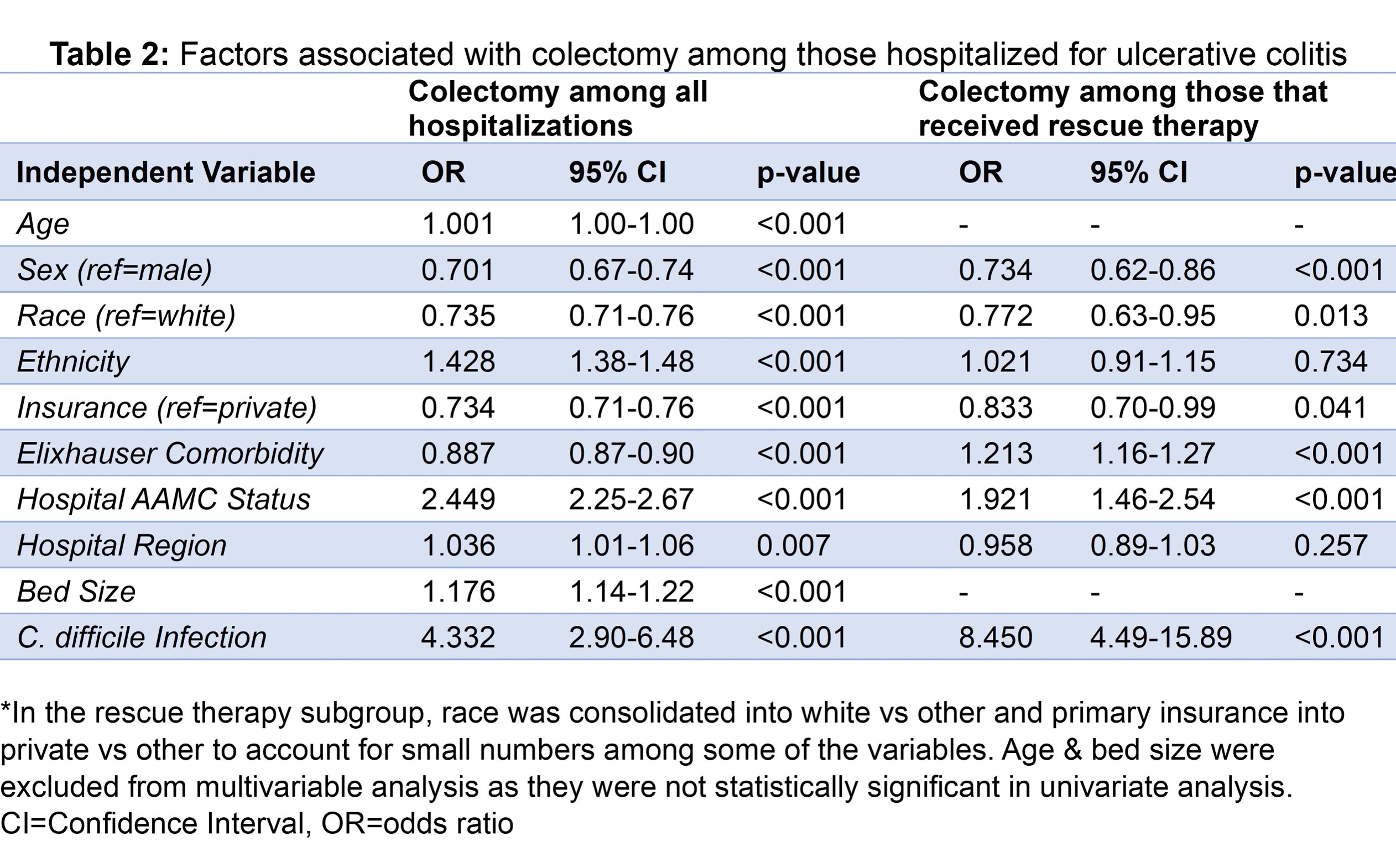
Figure: Table 2
Disclosures:
Laura Sahyoun indicated no relevant financial relationships.
Darrick Li: Phathom Pharmaceuticals – Speakers Bureau.
Badr Al Bawardy: AbbVie – Advisor or Review Panel Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Hikma – Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member. TAKEDA – Advisor or Review Panel Member, Speakers Bureau.
Laura Sahyoun, MD1, Darrick Li, MD, PhD2, Badr Al Bawardy, MD3. P5448 - Assessment of Sociodemographic Factors and Outcomes of Ulcerative Colitis Hospitalizations: A Large Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Weill Cornell Medicine, New York, NY; 2Yale School of Medicine, Waterford, CT; 3Yale New Haven Hospital, New Haven, USA; King Faisal Specialist Hospital and Research Center, Riyadh, Saudi Arabia, New Haven, CT
Introduction: Up to 25% of patients with ulcerative colitis (UC) will require hospitalization. Impact of sociodemographic factors on UC hospitalizations have not been fully explored. We aimed to assess the impact of sociodemographic factors on UC hospitalization outcomes and on rates of rescue medical therapy and colectomy using a large real-world observational cohort.
Methods: This is a retrospective study using the Vizient Clinical Database from 1/1/2016-12/31/2023. Patients hospitalized for UC were identified using ICD-10 codes. Primary outcome was the rate of inpatient colectomy. Subgroup analysis was performed on those who received rescue medical therapy, which was defined as at least 1 dose of either infliximab, cyclosporine, tacrolimus, upadacitinib or tofacitinib while hospitalized. Statistical significance was calculated using Pearson’s χ2 test for categorical variables and t-test for quantitative variables. Multivariable logistic regression was used to identify covariates associated with inpatient colectomy. A p-value < 0.05 was deemed statistically significant.
Results: A total of 43,377 patients were analyzed, of whom 17.9% (n=7747) underwent inpatient colectomy. Patients who underwent inpatient colectomy were more likely to be younger, male (57.3%), non-Hispanic white, have private insurance and be admitted at a teaching hospital (p< 0.001) (Table 1). In multivariable regression analysis, all factors assessed were independently associated with risk of colectomy.
Rescue medical therapy was reported in 15% (n=6085). Of those, 11.5% (n=697) underwent inpatient colectomy. Those who underwent colectomy were more likely to be male (p< 0.001), white (p=0.03), non-Hispanic (p=0.019), and have higher Elixhauser co-morbidity score (p< 0.001). Having private insurance (p=0.001) and being hospitalized at a larger hospital (p=0.003) or teaching hospital (p< 0.001) was associated with inpatient colectomy (Table 2). In multivariable regression analysis, female sex (OR 0.73, p< 0.001), non-white race (OR 0.77, p=0.013), and non-private insurance (OR 0.83, p=0.04) were associated with lower risk of colectomy. Higher comorbidity index (OR 1.21, p< 0.001) and teaching hospitals (OR 1.92, p< 0.001) were associated with higher risk of colectomy.
Discussion: Inpatient colectomy during a UC admission was more common among males, non-Hispanic whites, those with commercial/private insurance and admitted to a large or teaching hospital. Further studies to assess risk factors for inpatient colectomy are warranted.
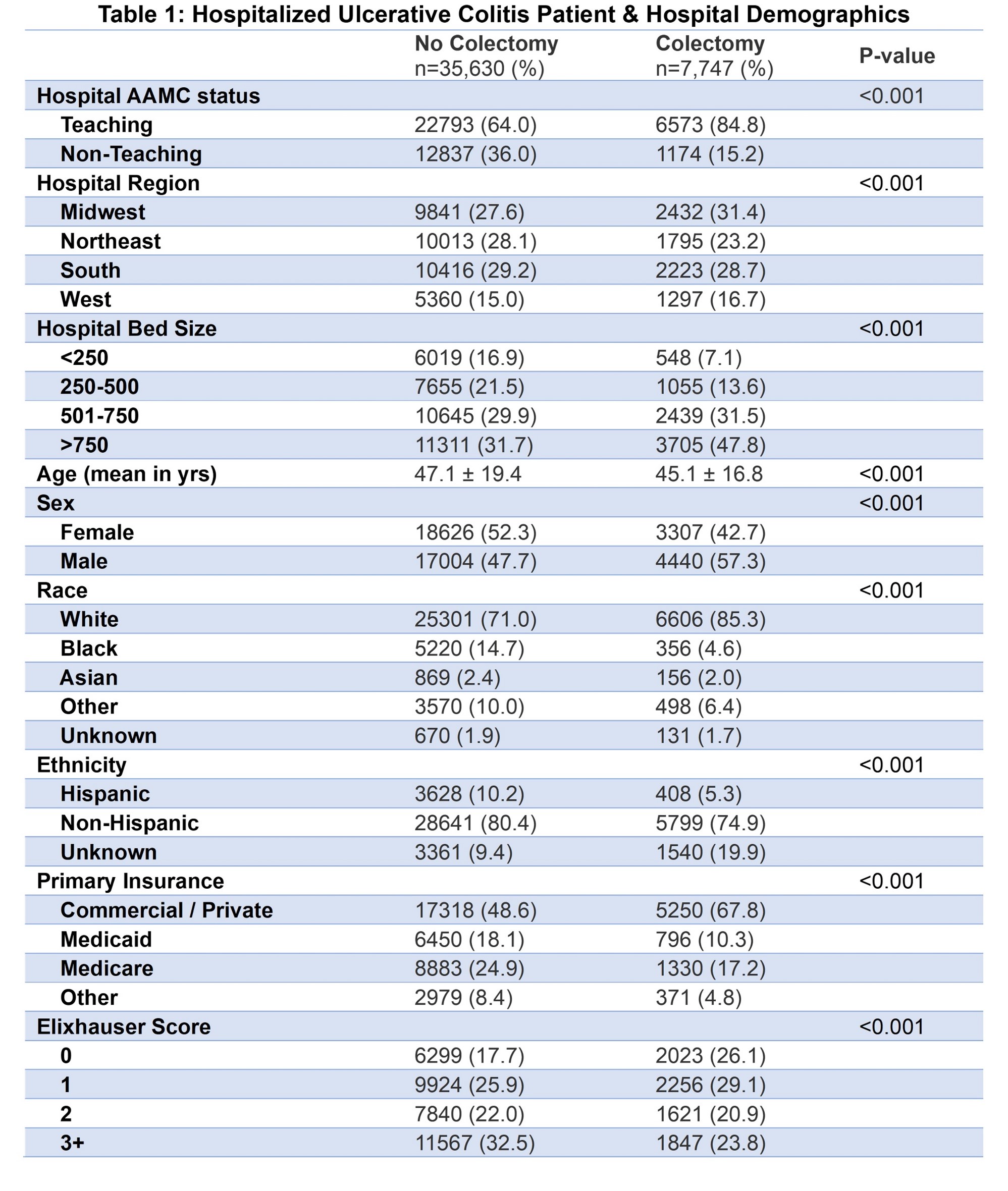
Figure: Table 1
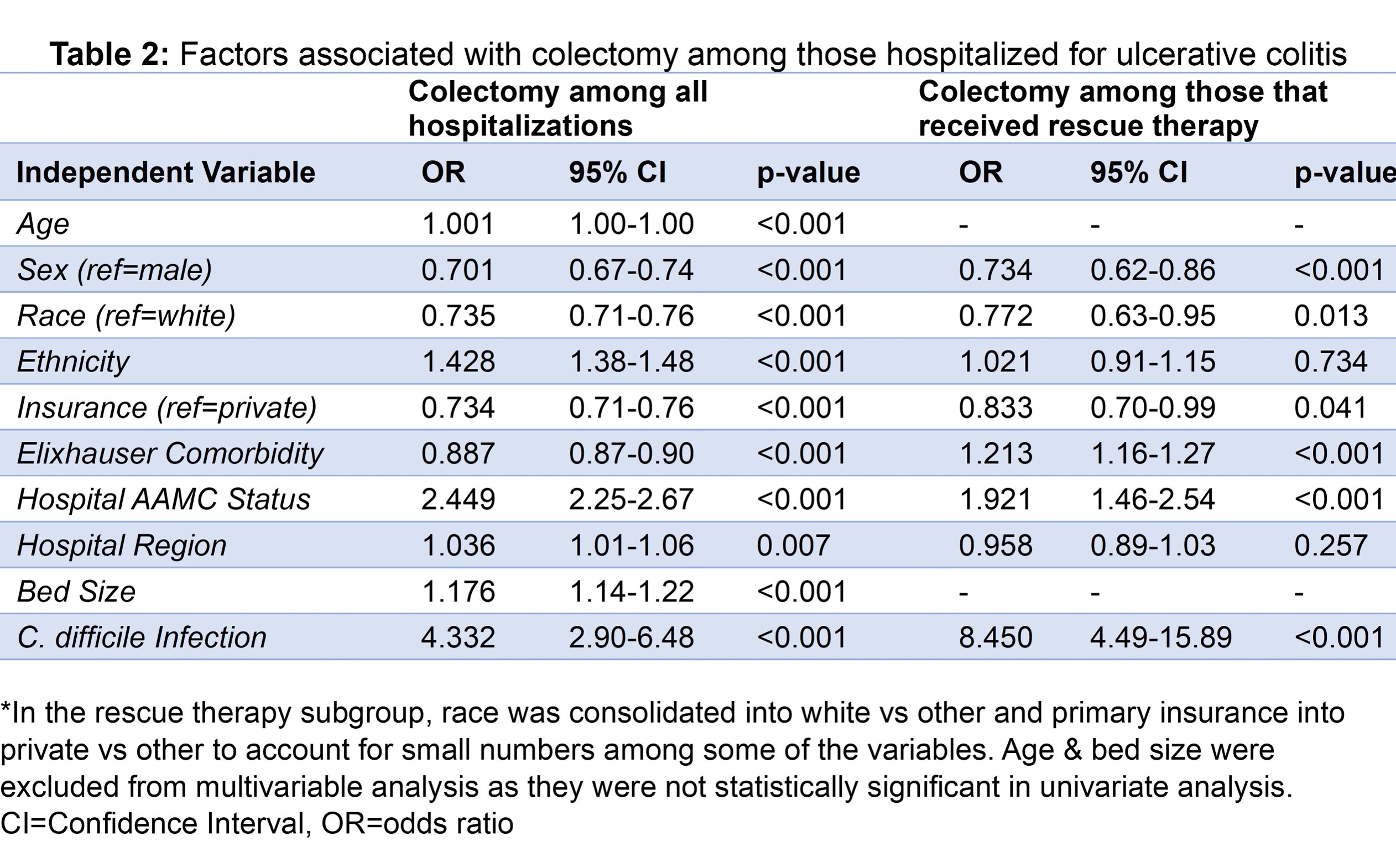
Figure: Table 2
Disclosures:
Laura Sahyoun indicated no relevant financial relationships.
Darrick Li: Phathom Pharmaceuticals – Speakers Bureau.
Badr Al Bawardy: AbbVie – Advisor or Review Panel Member, Consultant, Speakers Bureau. Bristol Myers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Hikma – Speakers Bureau. Janssen – Advisory Committee/Board Member, Speakers Bureau. Pfizer – Advisory Committee/Board Member. TAKEDA – Advisor or Review Panel Member, Speakers Bureau.
Laura Sahyoun, MD1, Darrick Li, MD, PhD2, Badr Al Bawardy, MD3. P5448 - Assessment of Sociodemographic Factors and Outcomes of Ulcerative Colitis Hospitalizations: A Large Population-Based Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
