Tuesday Poster Session
Category: IBD
P5444 - Presence of Spondyloarthritis Symptoms in IBD Is Associated With Higher Medication Use and Worse-Long Term Outcomes
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Simon J. Hong, MD
NYU Langone Health
New York, NY
Presenting Author(s)
Award: ACG Presidential Poster Award
Simon J. Hong, MD1, Rahul S. Dalal, MD, MPH2, Joerg Ermann, MD2, Andrew Stahly, MPH3, Frank I. Scott, MD, MSCE3, Benjamin Click, MD, MS4, Anna Way, MD3, Fardina Malik, MD, MS5, David Hudesman, MD, FACG6, Olivia Delau, MS1, Alexa Silfen, BA7, David T. Rubin, MD8, Michael Weisman, MD9, Kristine Kuhn, MD, PhD3, Reem Jan, MD7
1NYU Langone Health, New York, NY; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado, Denver, CO; 5University of Wisconsin, Madison, WI; 6NYU Langone Health Inflammatory Bowel Disease Center, New York, NY; 7University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 8University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL; 9Stanford University School of Medicine, Stanford, CA
Introduction: Musculoskeletal symptoms are the most common extra-intestinal manifestation of inflammatory bowel disease (IBD), with spondyloarthritis (SpA) reported in up to 50% of patients with IBD. In a recent study, we reported that 35% of IBD patients without known rheumatologic disease screened positive for SpA symptoms. In this follow-up study, we assessed the impact of a positive SpA screen on clinical outcomes at 1-year.
Methods: We previously administered two validated screening questionnaires for the detection of SpA in IBD (DETAIL = DETection of Arthritis in Inflammatory boweL diseases, IBIS-Q = IBD Identification of Spondyloarthritis Questionnaire) to IBD patients without a prior diagnosis of SpA. IBD providers were blinded to the questionnaire results. In this follow-up study, long-term outcomes up to 1 year after SpA screening were assessed by chart review. For all patients with available follow-up, we assessed subsequent rheumatologic evaluation, new medication initiation, and IBD or SpA-related clinical outcomes.
Results: This observational cohort included 317 patients (120 ulcerative colitis, 189 Crohn’s disease, 8 IBD-unclassified) with a median age of 38 years (IQR 29 – 51) and a 29% screen positive rate. When assessing clinical outcomes at 1-year, positive SpA screens were associated with numerically higher rates of a composite outcome of IBD- or SpA-related ED visit, hospitalization or IBD-related surgery (15% vs 8%; P=0.06). Screen-positive patients also had a significantly higher rate of NSAID use (8% vs 2%; P=0.02) and numerically higher rates of new biologic, systemic corticosteroid, and opioid use (Table 1). A positive SpA screen was associated with a higher use of any of these medications as a composite outcome (37% vs 23%; P=0.02). On multivariate analysis, a positive SpA screen (OR 1.8 [95% CI 1.01-3.1]), and higher number of prior advanced IBD therapy exposures (OR 1.5 [95% CI 1.2-1.9]) were significantly associated with medication use. Among patients with any positive SpA screen, a higher proportion were ultimately seen by a rheumatologist (9% vs 2%; P< 0.01).
Discussion: In patients with IBD, symptoms suggestive of SpA are associated with an increased risk of worse long-term IBD outcomes and a higher use of a combination of biologics, corticosteroids, opioids, and NSAIDs. Rheumatology referral rates remain low however, so strategies are needed to promote early identification and optimize treatment of SpA in patients with IBD.
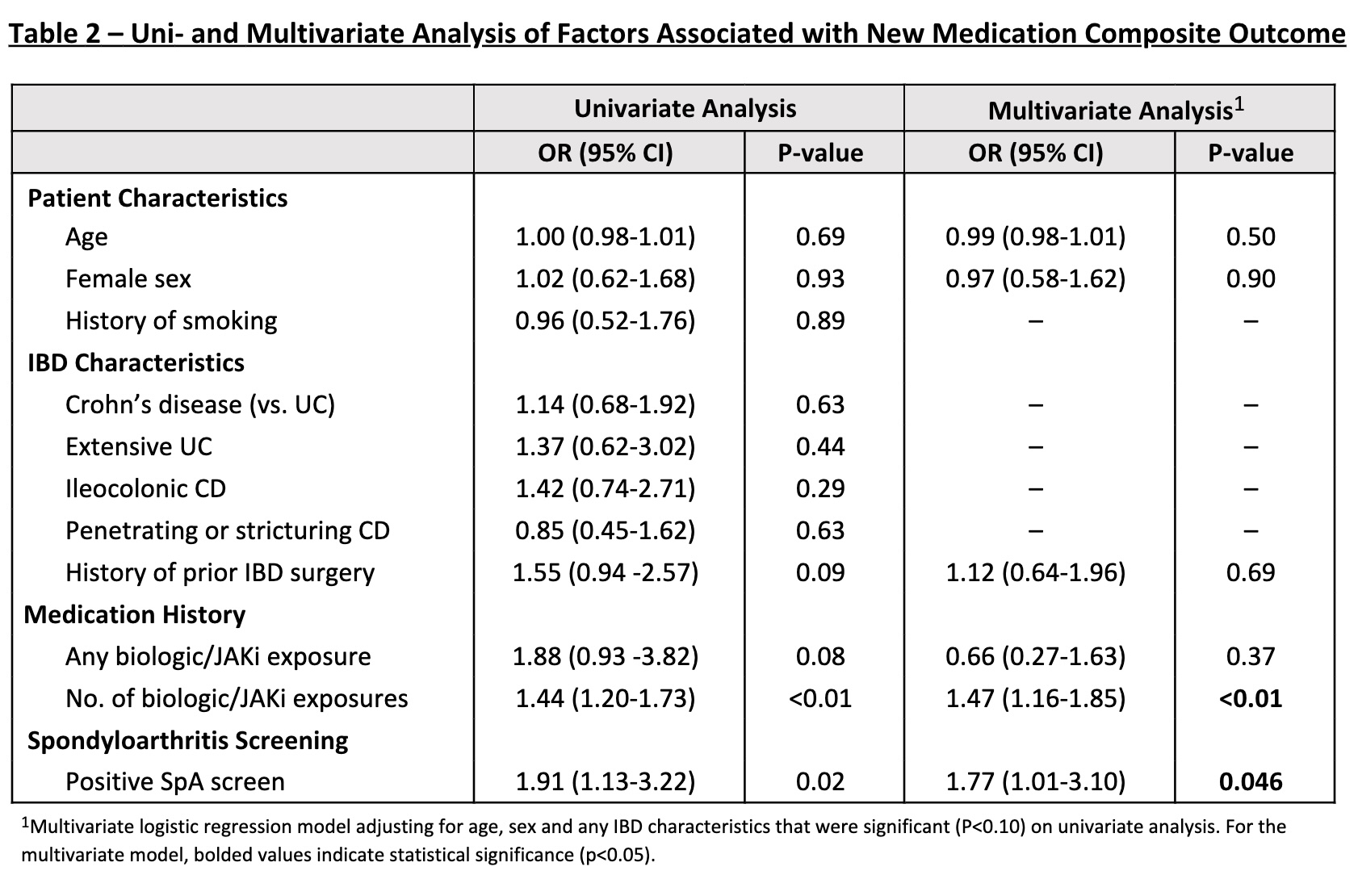
Figure: Table 1 - IBD and SpA-Related Outcomes at 1-Year Follow-up
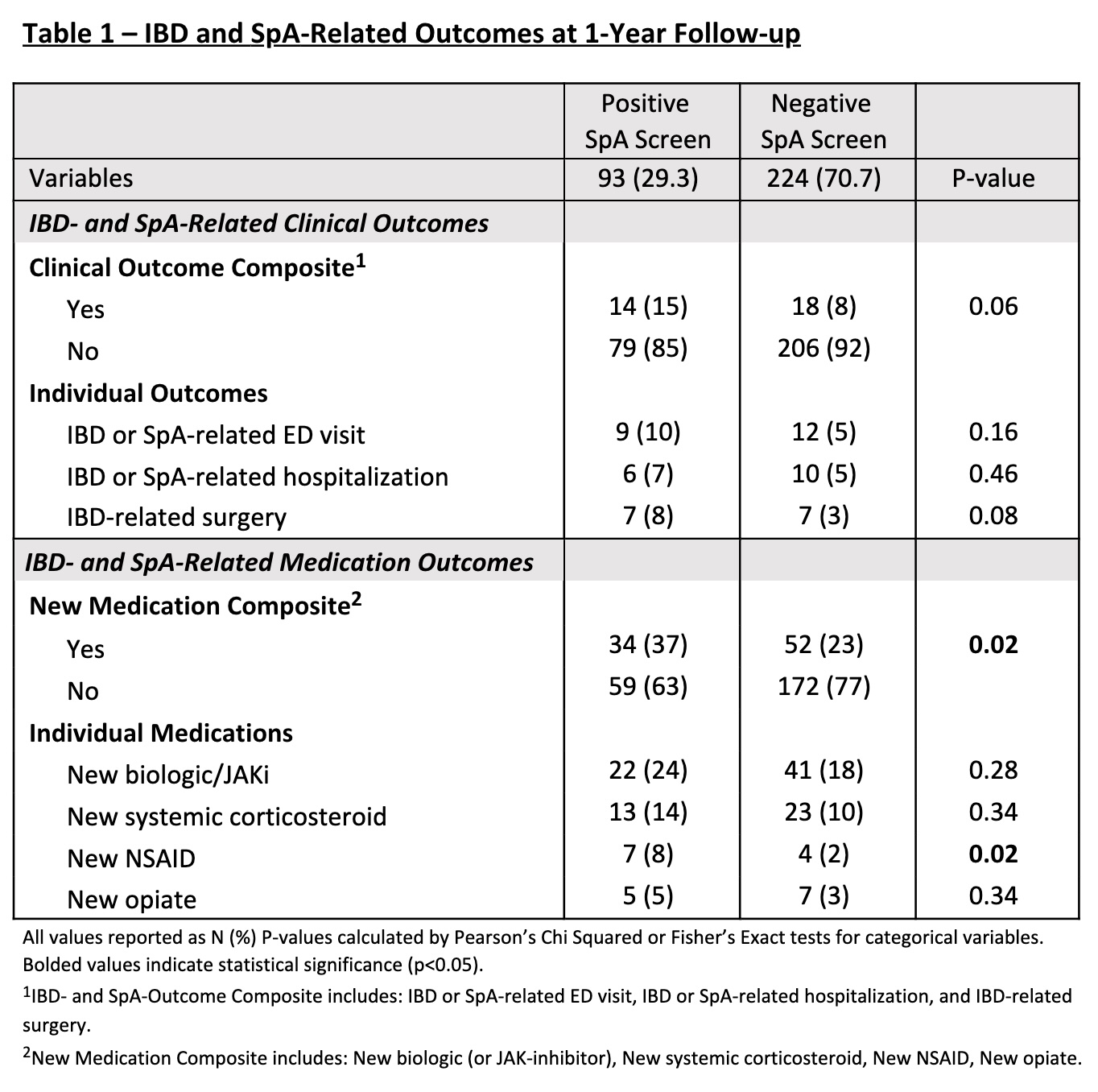
Figure: Table 2 – Uni- and Multivariate Analysis of Factors Associated with New Medication Composite Outcome
Disclosures:
Simon Hong: Abbvie – Advisory Committee/Board Member.
Rahul Dalal indicated no relevant financial relationships.
Joerg Ermann indicated no relevant financial relationships.
Andrew Stahly indicated no relevant financial relationships.
Frank Scott indicated no relevant financial relationships.
Benjamin Click indicated no relevant financial relationships.
Anna Way indicated no relevant financial relationships.
Fardina Malik indicated no relevant financial relationships.
David Hudesman: Abbvie – Consultant. Abivax – Consultant. Biocon – Consultant. BMS – Consultant. CorEvitas – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Johnson and Johnson – Consultant, Grant/Research Support. Pfizer – Consultant, Grant/Research Support. Prometheus – Consultant. Sanofi – Consultant. Takeda – Consultant.
Olivia Delau indicated no relevant financial relationships.
Alexa Silfen indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Michael Weisman: set point pharmaceuticals – data safety monitoring board. Spyre Therapeutics – Advisor or Review Panel Member.
Kristine Kuhn: Pfizer – Grant/Research Support. Solarea – Consultant.
Reem Jan indicated no relevant financial relationships.
Simon J. Hong, MD1, Rahul S. Dalal, MD, MPH2, Joerg Ermann, MD2, Andrew Stahly, MPH3, Frank I. Scott, MD, MSCE3, Benjamin Click, MD, MS4, Anna Way, MD3, Fardina Malik, MD, MS5, David Hudesman, MD, FACG6, Olivia Delau, MS1, Alexa Silfen, BA7, David T. Rubin, MD8, Michael Weisman, MD9, Kristine Kuhn, MD, PhD3, Reem Jan, MD7. P5444 - Presence of Spondyloarthritis Symptoms in IBD Is Associated With Higher Medication Use and Worse-Long Term Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Simon J. Hong, MD1, Rahul S. Dalal, MD, MPH2, Joerg Ermann, MD2, Andrew Stahly, MPH3, Frank I. Scott, MD, MSCE3, Benjamin Click, MD, MS4, Anna Way, MD3, Fardina Malik, MD, MS5, David Hudesman, MD, FACG6, Olivia Delau, MS1, Alexa Silfen, BA7, David T. Rubin, MD8, Michael Weisman, MD9, Kristine Kuhn, MD, PhD3, Reem Jan, MD7
1NYU Langone Health, New York, NY; 2Brigham and Women's Hospital, Harvard Medical School, Boston, MA; 3University of Colorado Anschutz Medical Campus, Aurora, CO; 4University of Colorado, Denver, CO; 5University of Wisconsin, Madison, WI; 6NYU Langone Health Inflammatory Bowel Disease Center, New York, NY; 7University of Chicago Medicine, Inflammatory Bowel Disease Center, Chicago, IL; 8University of Chicago Medicine Inflammatory Bowel Disease Center, Chicago, IL, USA, Chicago, IL; 9Stanford University School of Medicine, Stanford, CA
Introduction: Musculoskeletal symptoms are the most common extra-intestinal manifestation of inflammatory bowel disease (IBD), with spondyloarthritis (SpA) reported in up to 50% of patients with IBD. In a recent study, we reported that 35% of IBD patients without known rheumatologic disease screened positive for SpA symptoms. In this follow-up study, we assessed the impact of a positive SpA screen on clinical outcomes at 1-year.
Methods: We previously administered two validated screening questionnaires for the detection of SpA in IBD (DETAIL = DETection of Arthritis in Inflammatory boweL diseases, IBIS-Q = IBD Identification of Spondyloarthritis Questionnaire) to IBD patients without a prior diagnosis of SpA. IBD providers were blinded to the questionnaire results. In this follow-up study, long-term outcomes up to 1 year after SpA screening were assessed by chart review. For all patients with available follow-up, we assessed subsequent rheumatologic evaluation, new medication initiation, and IBD or SpA-related clinical outcomes.
Results: This observational cohort included 317 patients (120 ulcerative colitis, 189 Crohn’s disease, 8 IBD-unclassified) with a median age of 38 years (IQR 29 – 51) and a 29% screen positive rate. When assessing clinical outcomes at 1-year, positive SpA screens were associated with numerically higher rates of a composite outcome of IBD- or SpA-related ED visit, hospitalization or IBD-related surgery (15% vs 8%; P=0.06). Screen-positive patients also had a significantly higher rate of NSAID use (8% vs 2%; P=0.02) and numerically higher rates of new biologic, systemic corticosteroid, and opioid use (Table 1). A positive SpA screen was associated with a higher use of any of these medications as a composite outcome (37% vs 23%; P=0.02). On multivariate analysis, a positive SpA screen (OR 1.8 [95% CI 1.01-3.1]), and higher number of prior advanced IBD therapy exposures (OR 1.5 [95% CI 1.2-1.9]) were significantly associated with medication use. Among patients with any positive SpA screen, a higher proportion were ultimately seen by a rheumatologist (9% vs 2%; P< 0.01).
Discussion: In patients with IBD, symptoms suggestive of SpA are associated with an increased risk of worse long-term IBD outcomes and a higher use of a combination of biologics, corticosteroids, opioids, and NSAIDs. Rheumatology referral rates remain low however, so strategies are needed to promote early identification and optimize treatment of SpA in patients with IBD.
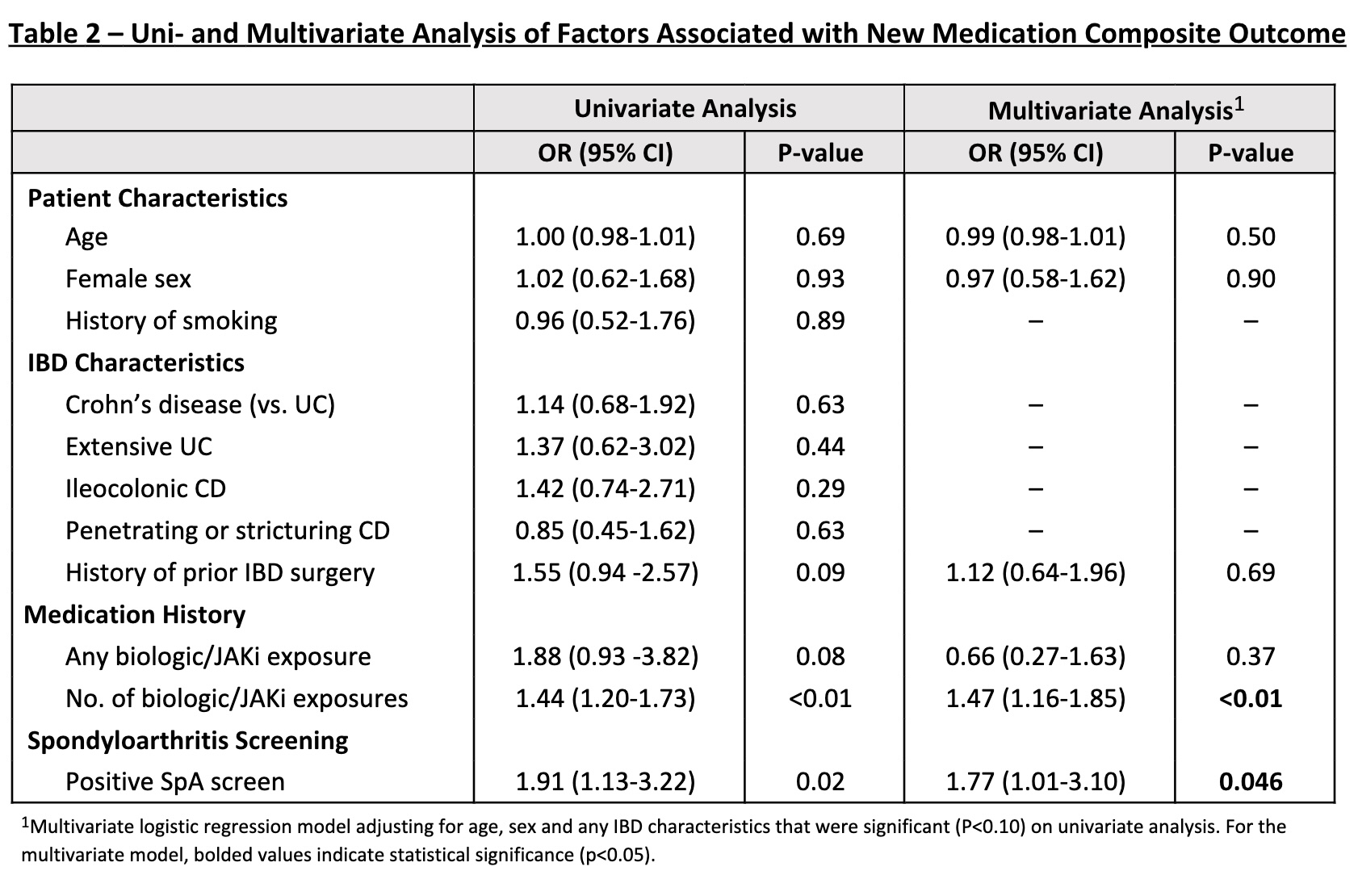
Figure: Table 1 - IBD and SpA-Related Outcomes at 1-Year Follow-up
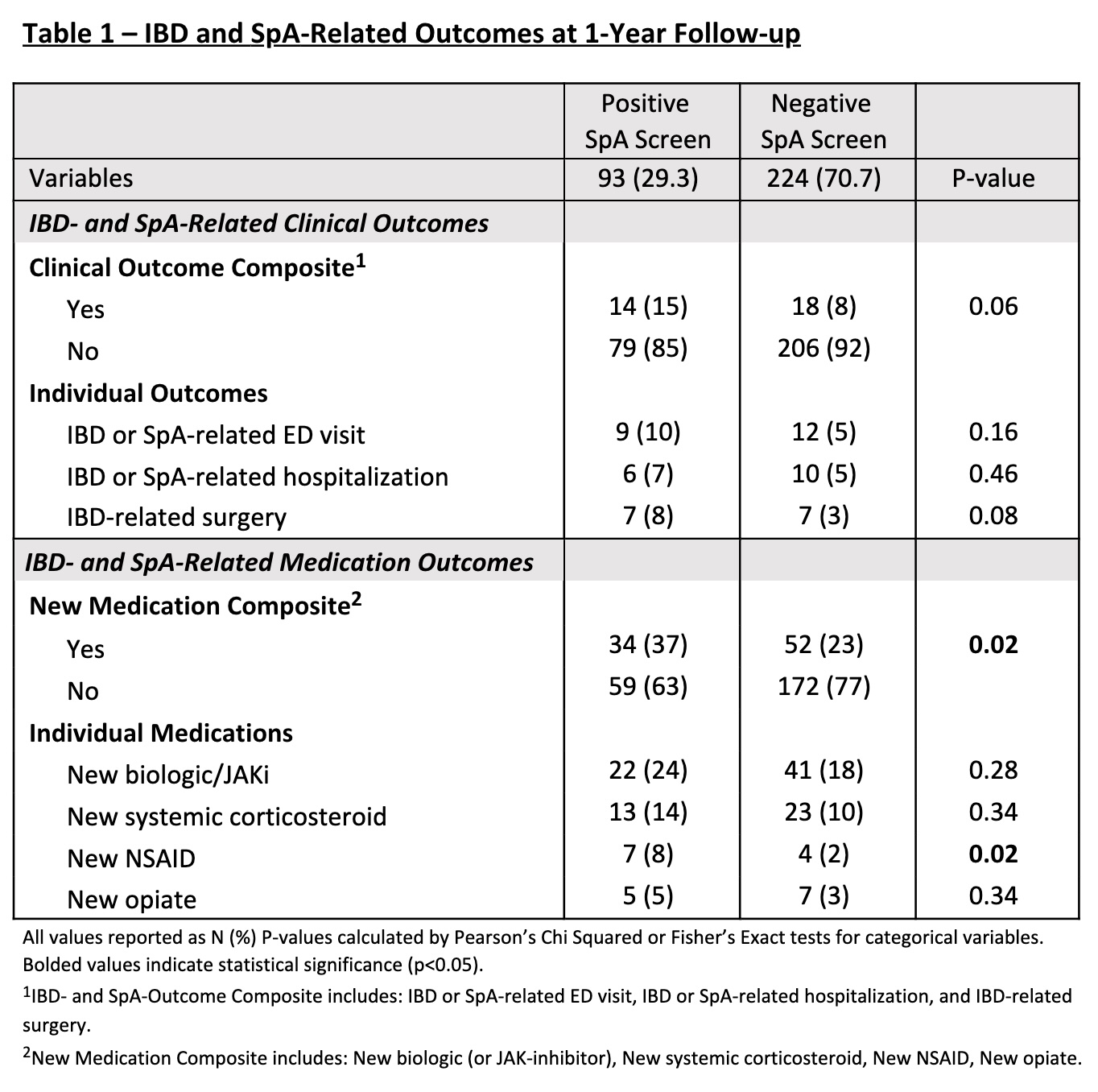
Figure: Table 2 – Uni- and Multivariate Analysis of Factors Associated with New Medication Composite Outcome
Disclosures:
Simon Hong: Abbvie – Advisory Committee/Board Member.
Rahul Dalal indicated no relevant financial relationships.
Joerg Ermann indicated no relevant financial relationships.
Andrew Stahly indicated no relevant financial relationships.
Frank Scott indicated no relevant financial relationships.
Benjamin Click indicated no relevant financial relationships.
Anna Way indicated no relevant financial relationships.
Fardina Malik indicated no relevant financial relationships.
David Hudesman: Abbvie – Consultant. Abivax – Consultant. Biocon – Consultant. BMS – Consultant. CorEvitas – Consultant. Eli Lilly – Consultant. Fresenius Kabi – Consultant. Johnson and Johnson – Consultant, Grant/Research Support. Pfizer – Consultant, Grant/Research Support. Prometheus – Consultant. Sanofi – Consultant. Takeda – Consultant.
Olivia Delau indicated no relevant financial relationships.
Alexa Silfen indicated no relevant financial relationships.
David Rubin: AbbVie – Advisory Committee/Board Member, Consultant, Speaker fees. Abivax SA – Consultant. Altrubio – Advisory Committee/Board Member, Consultant, Speaker feees, Stock Options. Avalo – Advisory Committee/Board Member, Consultant, Speaker fees. Bausch Health – Consultant. Bristol Myers Squibb – Advisory Committee/Board Member, Consultant, Speaker fees. Buhlmann Diagnostics – Advisory Committee/Board Member, Consultant, Speaker fees. Celltrion – Consultant. ClostraBio – Consultant. Connect BioPharma – Consultant. Cornerstones Health, Inc – Board of Directors membership. Douglas Pharmaceuticals – Consultant. Eli Lilly & Co. – Consultant. Foresee, Genentech (Roche) Inc. – Consultant. Image Analysis Group – Consultant. InDex Pharmaceutical – Consultant. Intouch Group – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Advisory Committee/Board Member, Consultant, Speaker fees. Iterative Health – Stock Options. Janssen Pharmaceuticals – Consultant. Lilly – Advisory Committee/Board Member, Consultant, Speaker fees. Odyssey Therapeutics – Consultant. Pfizer – Advisory Committee/Board Member, Consultant, Speaker fees. Sanofi – Consultant. Takeda – Advisory Committee/Board Member, Consultant, Grant/Research Support, Speaker fees. Throne – Consultant. Vedanta – Consultant.
Michael Weisman: set point pharmaceuticals – data safety monitoring board. Spyre Therapeutics – Advisor or Review Panel Member.
Kristine Kuhn: Pfizer – Grant/Research Support. Solarea – Consultant.
Reem Jan indicated no relevant financial relationships.
Simon J. Hong, MD1, Rahul S. Dalal, MD, MPH2, Joerg Ermann, MD2, Andrew Stahly, MPH3, Frank I. Scott, MD, MSCE3, Benjamin Click, MD, MS4, Anna Way, MD3, Fardina Malik, MD, MS5, David Hudesman, MD, FACG6, Olivia Delau, MS1, Alexa Silfen, BA7, David T. Rubin, MD8, Michael Weisman, MD9, Kristine Kuhn, MD, PhD3, Reem Jan, MD7. P5444 - Presence of Spondyloarthritis Symptoms in IBD Is Associated With Higher Medication Use and Worse-Long Term Outcomes, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

