Tuesday Poster Session
Category: IBD
P5434 - Therapeutic Trends and Flare Incidence in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease Undergoing Hormone Replacement Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Andrew Suchan, MD (he/him/his)
Johns Hopkins University School of Medicine
Baltimore, MD
Presenting Author(s)
Andrew Suchan, MD, Lara Chaaban, MD, Bashar Hassan, MD, Fan Liang, MD, Joanna Melia, MD, Sowmya Sharma, MD
Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: The effect of hormone replacement therapy (HRT) on inflammatory bowel disease (IBD) in transgender and gender non-conforming (TGNC) patients remains unknown. IBD, including ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic autoimmune disorder with significant morbidity. Understanding the unique challenges and risks faced by TGNC patients, particularly those undergoing HRT, is essential for optimizing care. This study explores therapeutic differences and changes in flare incidence in TGNC patients with and without HRT. Based on data from cisgender patients, we hypothesize that HRT would reduce flares.
Methods: We conducted a retrospective review of TGNC IBD patients from the Johns Hopkins Health System between January 2015 and October 2024. ICD codes were used to identify IBD patients with gender dysphoria. Patients were grouped by HRT status for comparison. Flares were classified as significant episodes requiring clinic, ED, or inpatient care, steroids, or adjustment in IBD therapy for new/increased IBD symptoms.
Results: 28 patients were included, 23 on HRT, 5 not. HRT patients trended older at 31.3 years (CI 10.11) versus 24.2 years (6.53), p=0.09. UC and CD rates were similar. Surprisingly, both groups were mostly transmen (Table 1). Treatment patterns were comparable, with most patients on maintenance therapy and no trends in histologic differences. 3 HRT patients had discontinued IBD therapy due to remission compared to 1 without HRT. The non-HRT group averaged 1.6 (2.07) flares compared to 0.52 (0.79) pre-HRT and 0.61 (0.94) post, p=0.06 and 0.1. 8 in the HRT group reported no flares in either period. The combined flare mean in HRT patients was 1.13 (1.32), p=.52. Adjusting for disease duration and years before/on HRT narrowed group differences (Table 2).
Discussion: We observed a trend toward fewer flares in HRT patients; however, the small sample size and duration limit conclusions. While IBD rates are equal in cis men and women, most patients were transmen, despite transwomen having 2-3 times greater prevalence in the general population, possibly reflecting genetic factors for inflammation. The observed age discrepancy may reflect greater opportunity for older patients to initiate HRT. These findings highlight the importance of tailored, inclusive IBD care, vigilant monitoring, and support for further investigation of disease trajectories in the young and expanding TGNC population.
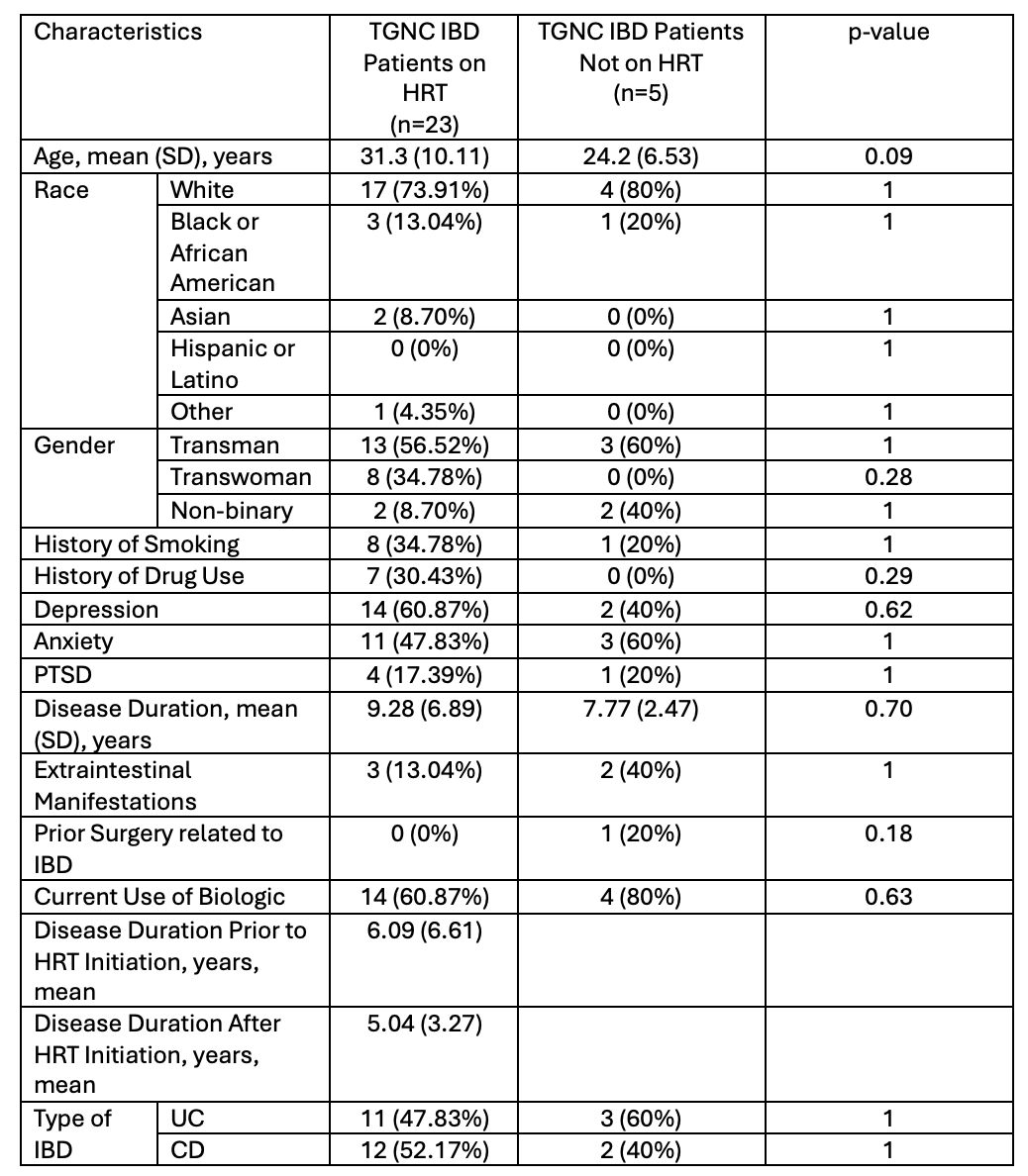
Figure: Table 1. Baseline characteristics
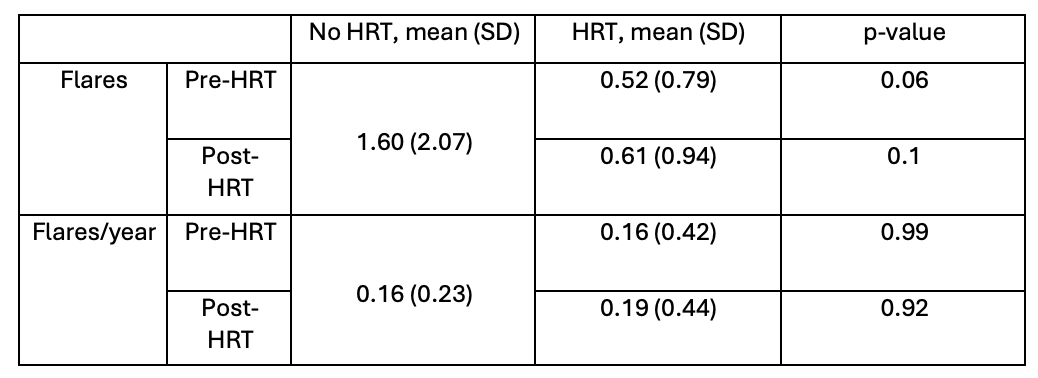
Figure: Table 2. Comparisons of flares between the TGNC cohorts with and without HRT
Disclosures:
Andrew Suchan indicated no relevant financial relationships.
Lara Chaaban indicated no relevant financial relationships.
Bashar Hassan indicated no relevant financial relationships.
Fan Liang indicated no relevant financial relationships.
Joanna Melia: Pfizer – Grant/Research Support.
Sowmya Sharma indicated no relevant financial relationships.
Andrew Suchan, MD, Lara Chaaban, MD, Bashar Hassan, MD, Fan Liang, MD, Joanna Melia, MD, Sowmya Sharma, MD. P5434 - Therapeutic Trends and Flare Incidence in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease Undergoing Hormone Replacement Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Johns Hopkins University School of Medicine, Baltimore, MD
Introduction: The effect of hormone replacement therapy (HRT) on inflammatory bowel disease (IBD) in transgender and gender non-conforming (TGNC) patients remains unknown. IBD, including ulcerative colitis (UC) and Crohn’s disease (CD), is a chronic autoimmune disorder with significant morbidity. Understanding the unique challenges and risks faced by TGNC patients, particularly those undergoing HRT, is essential for optimizing care. This study explores therapeutic differences and changes in flare incidence in TGNC patients with and without HRT. Based on data from cisgender patients, we hypothesize that HRT would reduce flares.
Methods: We conducted a retrospective review of TGNC IBD patients from the Johns Hopkins Health System between January 2015 and October 2024. ICD codes were used to identify IBD patients with gender dysphoria. Patients were grouped by HRT status for comparison. Flares were classified as significant episodes requiring clinic, ED, or inpatient care, steroids, or adjustment in IBD therapy for new/increased IBD symptoms.
Results: 28 patients were included, 23 on HRT, 5 not. HRT patients trended older at 31.3 years (CI 10.11) versus 24.2 years (6.53), p=0.09. UC and CD rates were similar. Surprisingly, both groups were mostly transmen (Table 1). Treatment patterns were comparable, with most patients on maintenance therapy and no trends in histologic differences. 3 HRT patients had discontinued IBD therapy due to remission compared to 1 without HRT. The non-HRT group averaged 1.6 (2.07) flares compared to 0.52 (0.79) pre-HRT and 0.61 (0.94) post, p=0.06 and 0.1. 8 in the HRT group reported no flares in either period. The combined flare mean in HRT patients was 1.13 (1.32), p=.52. Adjusting for disease duration and years before/on HRT narrowed group differences (Table 2).
Discussion: We observed a trend toward fewer flares in HRT patients; however, the small sample size and duration limit conclusions. While IBD rates are equal in cis men and women, most patients were transmen, despite transwomen having 2-3 times greater prevalence in the general population, possibly reflecting genetic factors for inflammation. The observed age discrepancy may reflect greater opportunity for older patients to initiate HRT. These findings highlight the importance of tailored, inclusive IBD care, vigilant monitoring, and support for further investigation of disease trajectories in the young and expanding TGNC population.
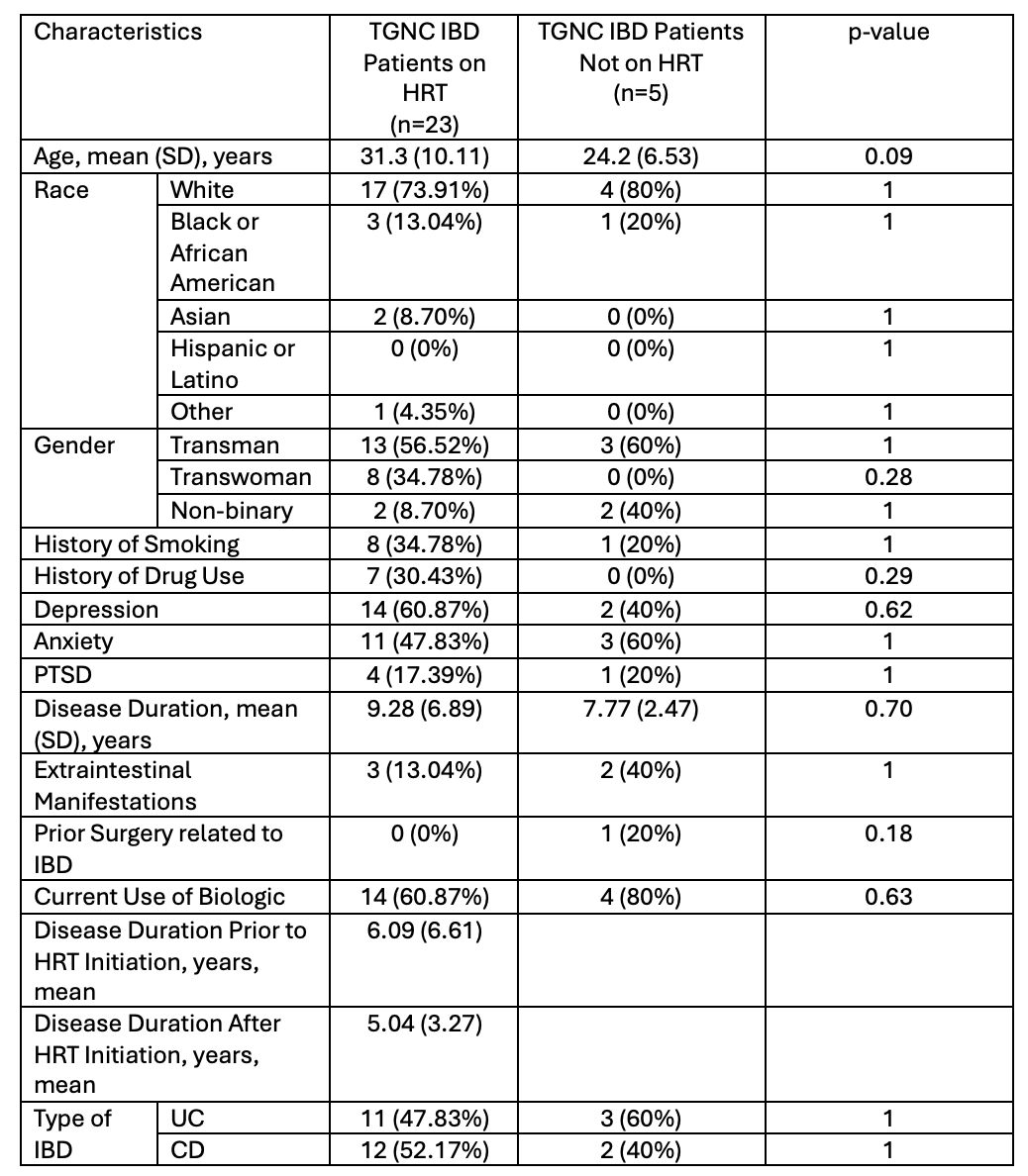
Figure: Table 1. Baseline characteristics
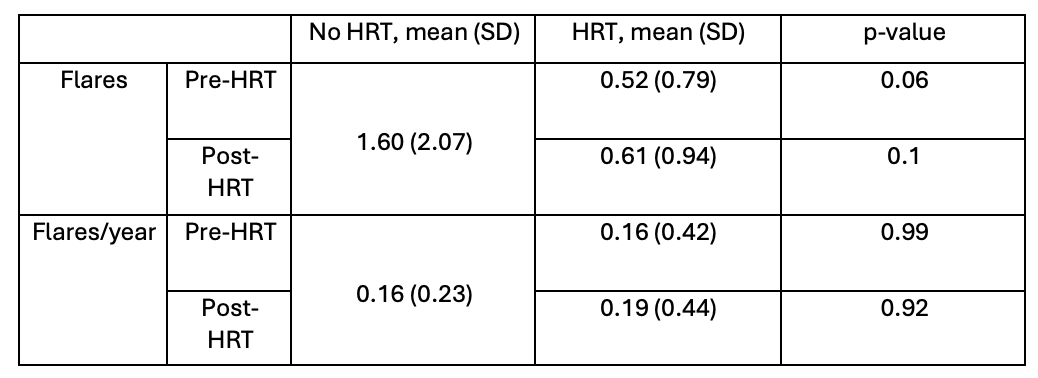
Figure: Table 2. Comparisons of flares between the TGNC cohorts with and without HRT
Disclosures:
Andrew Suchan indicated no relevant financial relationships.
Lara Chaaban indicated no relevant financial relationships.
Bashar Hassan indicated no relevant financial relationships.
Fan Liang indicated no relevant financial relationships.
Joanna Melia: Pfizer – Grant/Research Support.
Sowmya Sharma indicated no relevant financial relationships.
Andrew Suchan, MD, Lara Chaaban, MD, Bashar Hassan, MD, Fan Liang, MD, Joanna Melia, MD, Sowmya Sharma, MD. P5434 - Therapeutic Trends and Flare Incidence in Transgender and Gender Non-Conforming Patients With Inflammatory Bowel Disease Undergoing Hormone Replacement Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
