Tuesday Poster Session
Category: IBD
P5409 - Who Bears the Brunt? Geographic, Racial, and Ethnic Disparities in Inflammatory Bowel Disease in the United States
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Aria Khan, MD (she/her/hers)
NYC Health + Hospitals/Woodhull
Jamaica, NY
Presenting Author(s)
Shamikha Cheema, MBBS1, Aria Khan, MD2, Syed Ibad Hussain, MBBS3, Momina Khaliq, MBBS4, Arun Kumar. Maloth, MBBS5, Muhammad Shaheer Bin Faheem, MBBS6, Muhammad Faique Hassan, MBBS1, Hassan Ijaz, MBBS7
1King Edward Medical University, Lahore, Punjab, Pakistan; 2NYC Health + Hospitals/Woodhull, Jamaica, NY; 3Jinnah Sindh Medical University, Karachi, Sindh, Pakistan; 4Edward Medical University Lahore, Lahore, Punjab, Pakistan; 5Kakatiya Medical College, Warangal, India, Warangal, Telangana, India; 6Karachi Institute of Medical Sciences, KIMS, Karachi, Sindh, Pakistan; 7King Edward Medical University Lahore, Lahore, Punjab, Pakistan
Introduction: Inflammatory bowel diseases (IBD) have emerged as a major health concern in modern times, particularly in Westernized nations that have recently joined the industrialized world. The burden of IBD remains significant, with a prevalence exceeding 0.3%. These statistics underscore the need for research on the prevention of inflammatory bowel disease and advancements in healthcare systems to address this intricate and expensive condition.
Methods: Mortality data were extracted from the CDC WONDER database (2018–2023), and analysis was performed to calculate age-adjusted mortality rates (AAMRs) per 1,00,000 people. Annual percent changes (APCs) with 95% confidence intervals were calculated for each group. The trends across various demographic variables such as race, gender, age, and urban vs rural status were assessed using the Joinpoint Regression Program (v 5.1.0).
Results: Between 2018 and 2023, 25,153 IBD-related deaths occurred among adults in the United States. The AAMR increased from 8.27 per 100,000 in 2018 to 10.76 in 2023 (APC= 5.60; 95% CI, 0.04-12.30). Men had higher AAMRs than women between 2018 and 2023 (overall AAMR men: 10.9 vs. women: 9.8) with an APC= 5.69; 95% CI, 0.74-10.89, p= 0.032786. In 2023, the highest AAMRs were observed among non-Hispanic (NH) White individuals (11.4) (APC= 6.18;95% CI, 0.20-12.52, p= 0.045285), followed by NH Black (6.9), NH American Indian (5.8), Hispanic (3.7), and NH Asian (2.0) populations. The Midwest region had the highest regional AAMR (11.5), followed by the West (10.9), South (9.7), and Northeast regions (9.4). States in the top 90th percentile for AAMR included Oregon, Vermont, Rhode Island, Colorado, and Minnesota, each with approximately double the AAMRs of those in the bottom 10th percentile, such as Hawaii, Florida, the District of Columbia, Arizona, and New Jersey.
Discussion: The rising burden of IBD in the US highlights the systemic disproportions and gaps in resource allocation and gut health maintenance. Focused public health strategies should be implemented to control preventable deaths and reduce inequities in vulnerable populations.
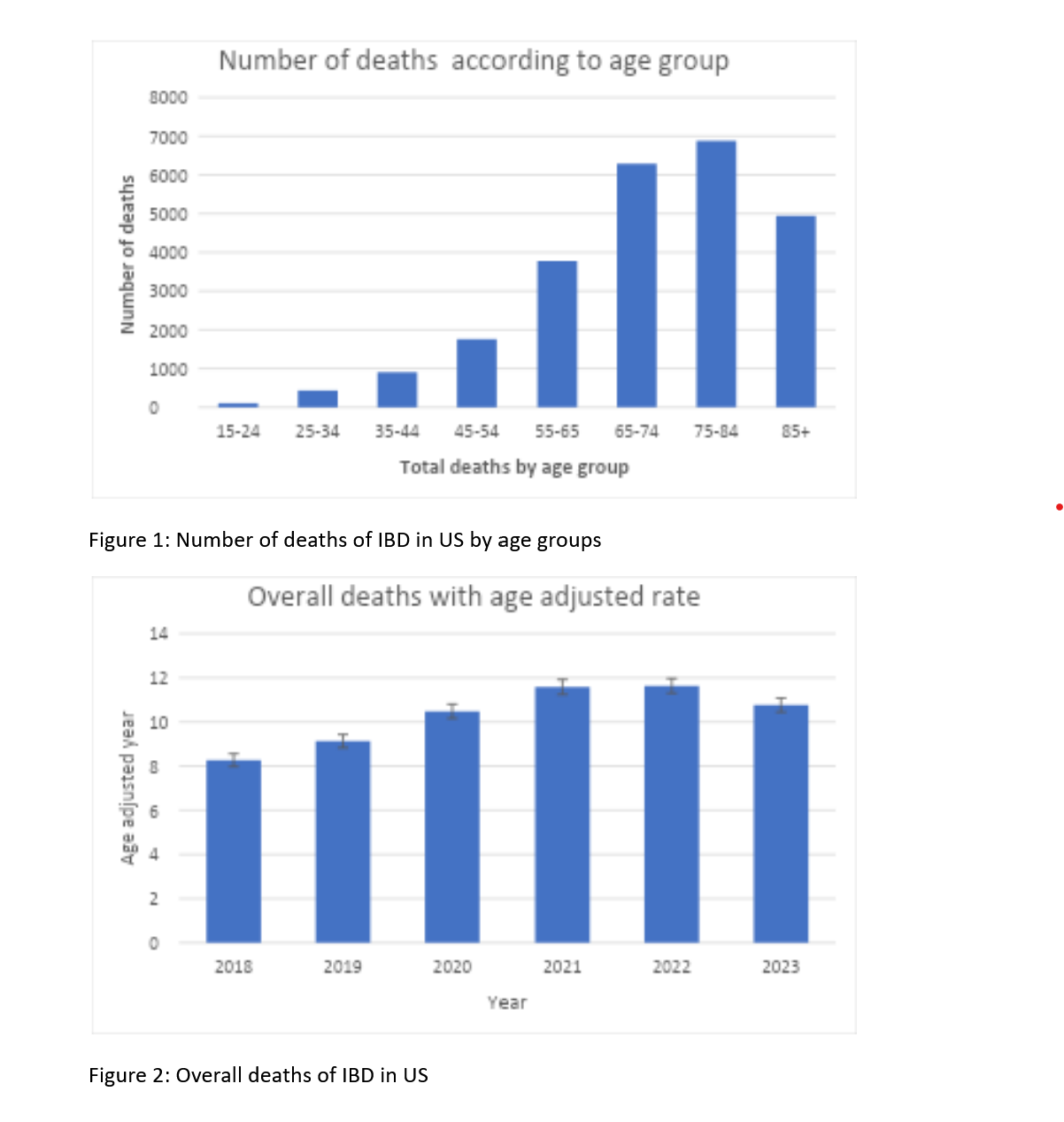
Figure: Number of deaths of IBD in US by age groups and Overall deaths of IBD in US
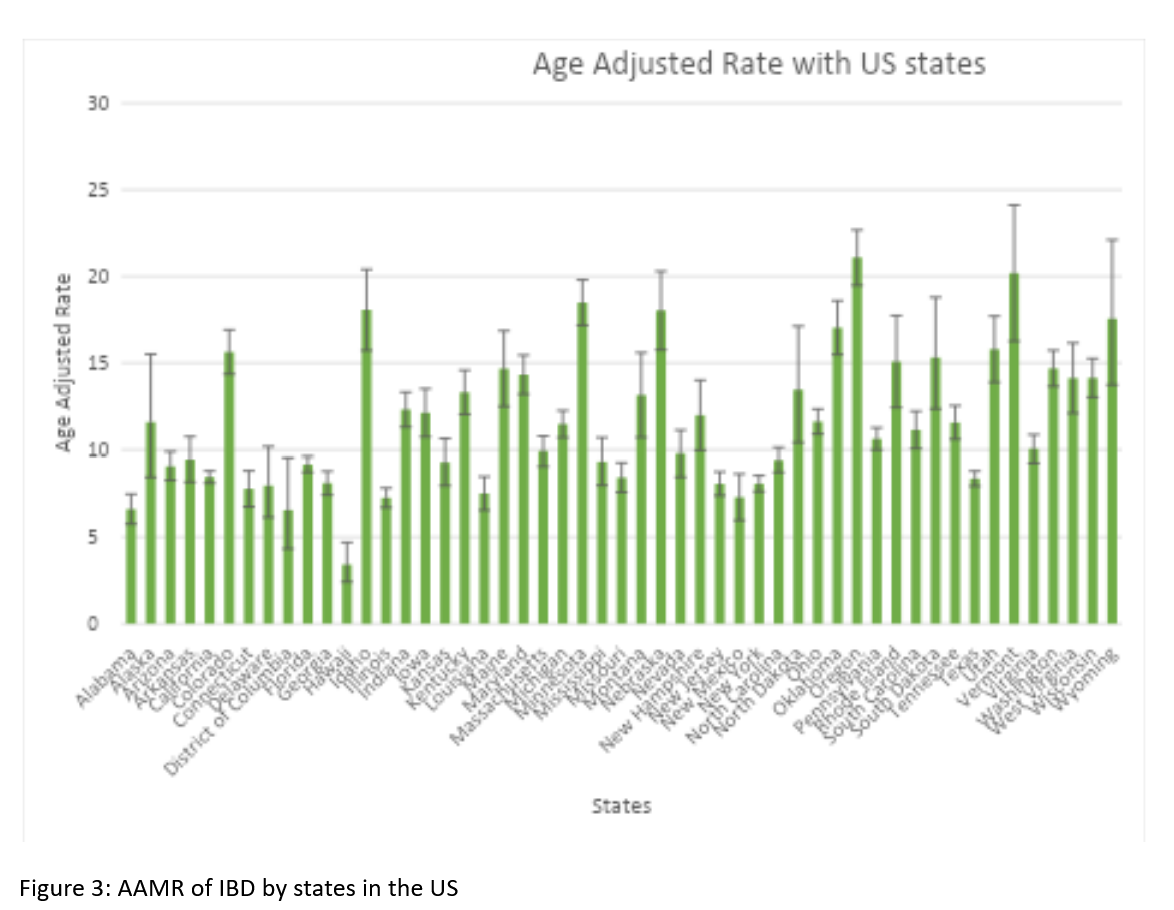
Figure: AAMR of IBD by states in the US
Disclosures:
Shamikha Cheema indicated no relevant financial relationships.
Aria Khan indicated no relevant financial relationships.
Syed Ibad Hussain indicated no relevant financial relationships.
Momina Khaliq indicated no relevant financial relationships.
Arun Maloth indicated no relevant financial relationships.
Muhammad Shaheer Bin Faheem indicated no relevant financial relationships.
Muhammad Faique Hassan indicated no relevant financial relationships.
Hassan Ijaz indicated no relevant financial relationships.
Shamikha Cheema, MBBS1, Aria Khan, MD2, Syed Ibad Hussain, MBBS3, Momina Khaliq, MBBS4, Arun Kumar. Maloth, MBBS5, Muhammad Shaheer Bin Faheem, MBBS6, Muhammad Faique Hassan, MBBS1, Hassan Ijaz, MBBS7. P5409 - Who Bears the Brunt? Geographic, Racial, and Ethnic Disparities in Inflammatory Bowel Disease in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1King Edward Medical University, Lahore, Punjab, Pakistan; 2NYC Health + Hospitals/Woodhull, Jamaica, NY; 3Jinnah Sindh Medical University, Karachi, Sindh, Pakistan; 4Edward Medical University Lahore, Lahore, Punjab, Pakistan; 5Kakatiya Medical College, Warangal, India, Warangal, Telangana, India; 6Karachi Institute of Medical Sciences, KIMS, Karachi, Sindh, Pakistan; 7King Edward Medical University Lahore, Lahore, Punjab, Pakistan
Introduction: Inflammatory bowel diseases (IBD) have emerged as a major health concern in modern times, particularly in Westernized nations that have recently joined the industrialized world. The burden of IBD remains significant, with a prevalence exceeding 0.3%. These statistics underscore the need for research on the prevention of inflammatory bowel disease and advancements in healthcare systems to address this intricate and expensive condition.
Methods: Mortality data were extracted from the CDC WONDER database (2018–2023), and analysis was performed to calculate age-adjusted mortality rates (AAMRs) per 1,00,000 people. Annual percent changes (APCs) with 95% confidence intervals were calculated for each group. The trends across various demographic variables such as race, gender, age, and urban vs rural status were assessed using the Joinpoint Regression Program (v 5.1.0).
Results: Between 2018 and 2023, 25,153 IBD-related deaths occurred among adults in the United States. The AAMR increased from 8.27 per 100,000 in 2018 to 10.76 in 2023 (APC= 5.60; 95% CI, 0.04-12.30). Men had higher AAMRs than women between 2018 and 2023 (overall AAMR men: 10.9 vs. women: 9.8) with an APC= 5.69; 95% CI, 0.74-10.89, p= 0.032786. In 2023, the highest AAMRs were observed among non-Hispanic (NH) White individuals (11.4) (APC= 6.18;95% CI, 0.20-12.52, p= 0.045285), followed by NH Black (6.9), NH American Indian (5.8), Hispanic (3.7), and NH Asian (2.0) populations. The Midwest region had the highest regional AAMR (11.5), followed by the West (10.9), South (9.7), and Northeast regions (9.4). States in the top 90th percentile for AAMR included Oregon, Vermont, Rhode Island, Colorado, and Minnesota, each with approximately double the AAMRs of those in the bottom 10th percentile, such as Hawaii, Florida, the District of Columbia, Arizona, and New Jersey.
Discussion: The rising burden of IBD in the US highlights the systemic disproportions and gaps in resource allocation and gut health maintenance. Focused public health strategies should be implemented to control preventable deaths and reduce inequities in vulnerable populations.
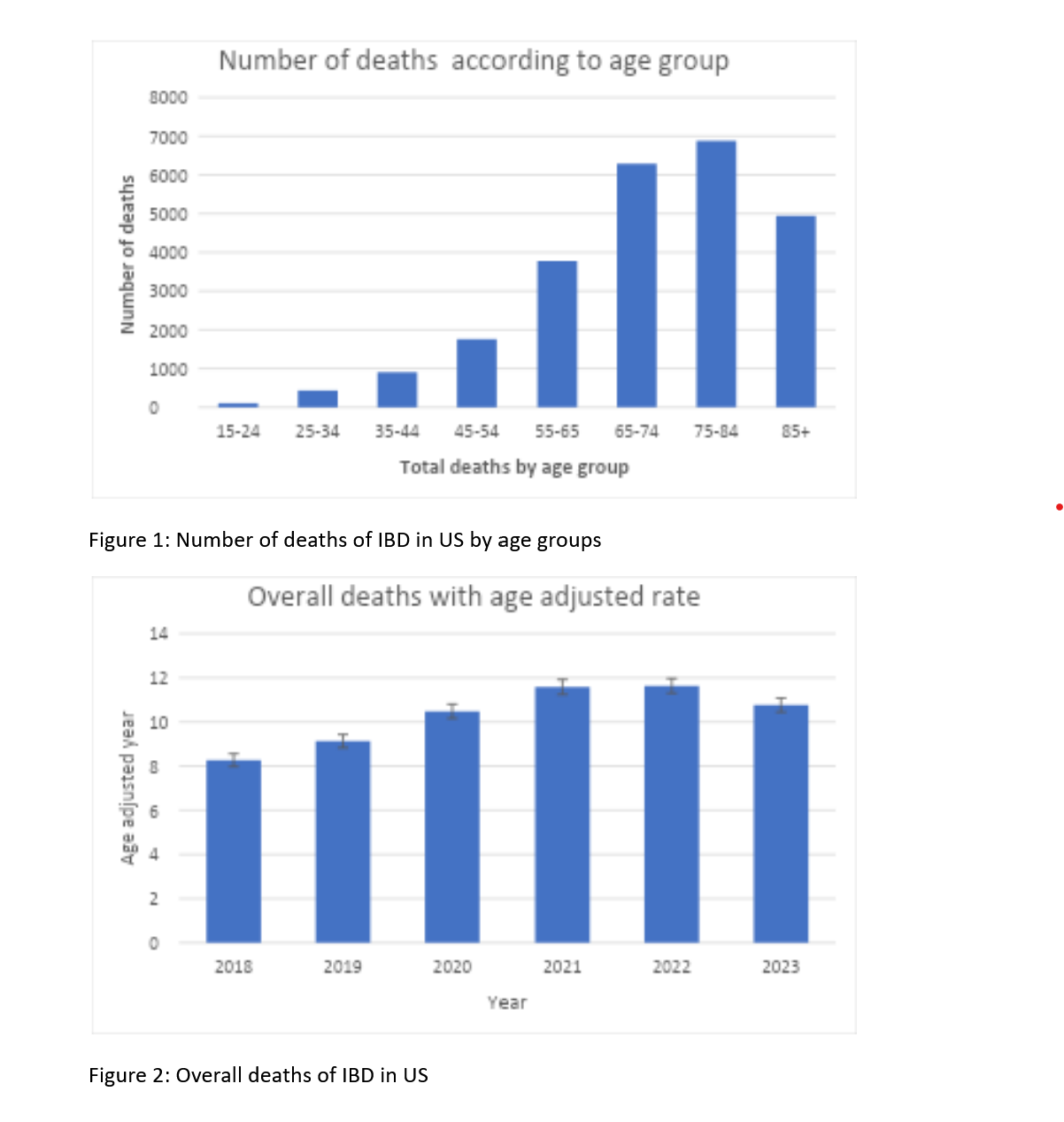
Figure: Number of deaths of IBD in US by age groups and Overall deaths of IBD in US
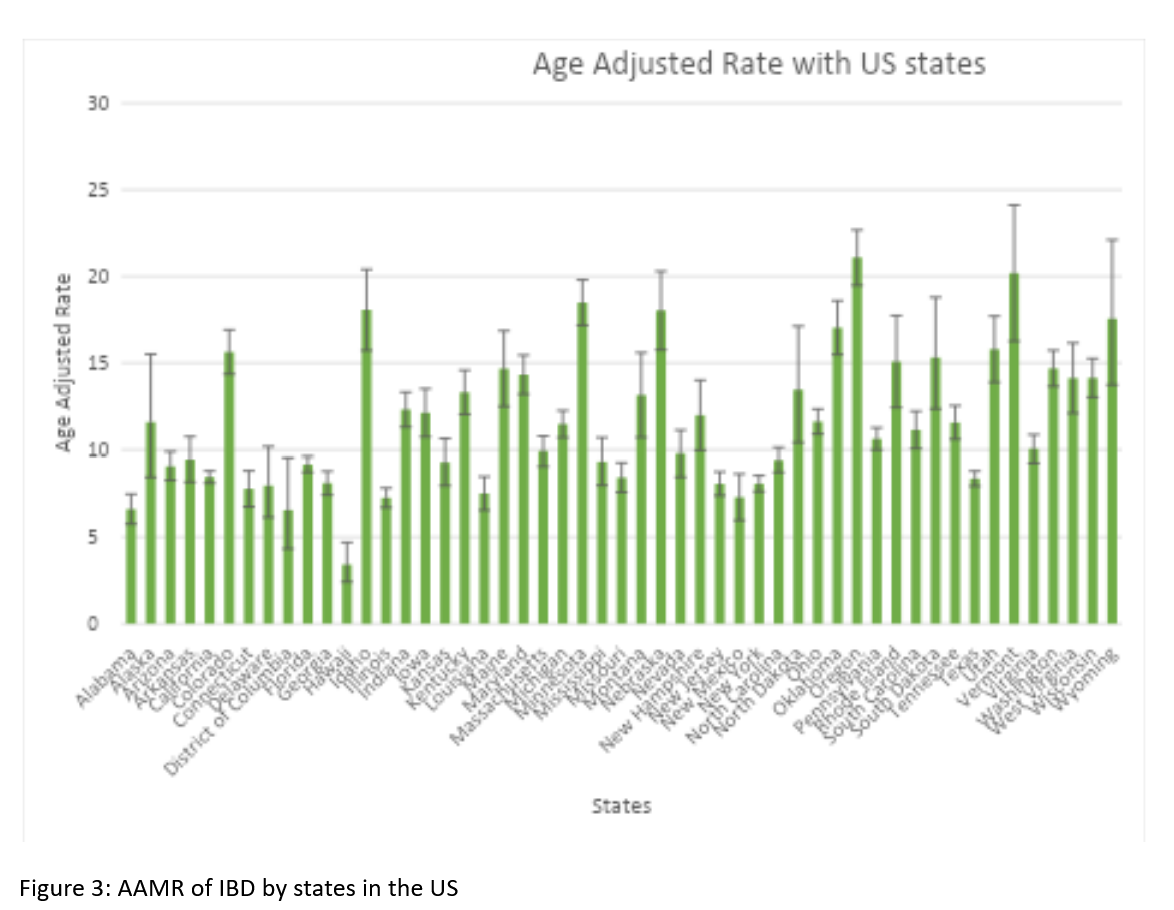
Figure: AAMR of IBD by states in the US
Disclosures:
Shamikha Cheema indicated no relevant financial relationships.
Aria Khan indicated no relevant financial relationships.
Syed Ibad Hussain indicated no relevant financial relationships.
Momina Khaliq indicated no relevant financial relationships.
Arun Maloth indicated no relevant financial relationships.
Muhammad Shaheer Bin Faheem indicated no relevant financial relationships.
Muhammad Faique Hassan indicated no relevant financial relationships.
Hassan Ijaz indicated no relevant financial relationships.
Shamikha Cheema, MBBS1, Aria Khan, MD2, Syed Ibad Hussain, MBBS3, Momina Khaliq, MBBS4, Arun Kumar. Maloth, MBBS5, Muhammad Shaheer Bin Faheem, MBBS6, Muhammad Faique Hassan, MBBS1, Hassan Ijaz, MBBS7. P5409 - Who Bears the Brunt? Geographic, Racial, and Ethnic Disparities in Inflammatory Bowel Disease in the United States, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
