Tuesday Poster Session
Category: IBD
P5398 - Appendectomy Improves Outcomes in Appendicitis Patients With and Without Ulcerative Colitis: A Nationwide Inpatient Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Isaac Giovannie, MD
Rush University Medical Center
Chicago, IL
Presenting Author(s)
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Joseph Frasca, MD1, Zoe Post, MD, MSc1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1
1Rush University Medical Center, Chicago, IL; 2Infirmary Health, Mobile, AL; 3Rush University Medical Center, Chicagoii, IL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease associated with increased healthcare utilization and surgical complexity. While appendectomy is a common and effective treatment for appendicitis, limited data exist on its impact in patients with coexisting UC. Given concerns about altered immune response and postoperative risk in UC, we aimed to assess whether appendectomy improves hospital outcomes in appendicitis patients with UC and how its effects compare to those without UC.
Methods: We conducted a retrospective cohort study using data from the National Inpatient Sample (NIS) from 2016–2019. We identified adult patients hospitalized with a principal diagnosis of appendicitis, excluding those who had undergone colectomy or ileocecectomy. Patients were stratified based on UC status. Multivariable linear and logistic regression models were used to evaluate the effect of appendectomy on three key outcomes: length of stay (LOS), total hospital charges (TOTCHG), and in-hospital mortality. Interaction terms were included to assess whether UC status modified the effect of appendectomy on these outcomes. All analyses accounted for demographic variables and hospital characteristics.
Results: We identified 141,349 hospitalized adults with appendicitis, including 505 (0.36%) with UC. Compared to non-UC patients, UC patients had worse outcomes: longer length of stay (LOS; 5.01 vs. 3.73 days), higher hospital charges ($77,723 vs. $62,460), and higher in-hospital mortality (1.2% vs. 0.4%, p = 0.008). In multivariable models, appendectomy was linked to shorter LOS and lower charges in both groups. Among UC patients, appendectomy reduced LOS by 2.56 days and charges by $19,738; among non-UC patients, it reduced LOS by 2.19 days and charges by $3,993 (all p < 0.05). Appendectomy significantly lowered overall in-hospital mortality (aOR = 0.19, p < 0.001). Although UC was independently associated with higher mortality, interaction terms showed that appendectomy’s benefits were consistent regardless of UC status.
Discussion: These findings support appendectomy as an effective intervention in appendicitis, including in UC patients. Despite worse baseline outcomes, UC patients saw significant reductions in LOS, charges, and mortality, similar to non-UC patients. This challenges concerns about surgical risk in UC and highlights appendectomy’s value in improving short-term outcomes. Further research is needed to assess long-term results and post-discharge complications in UC patients.
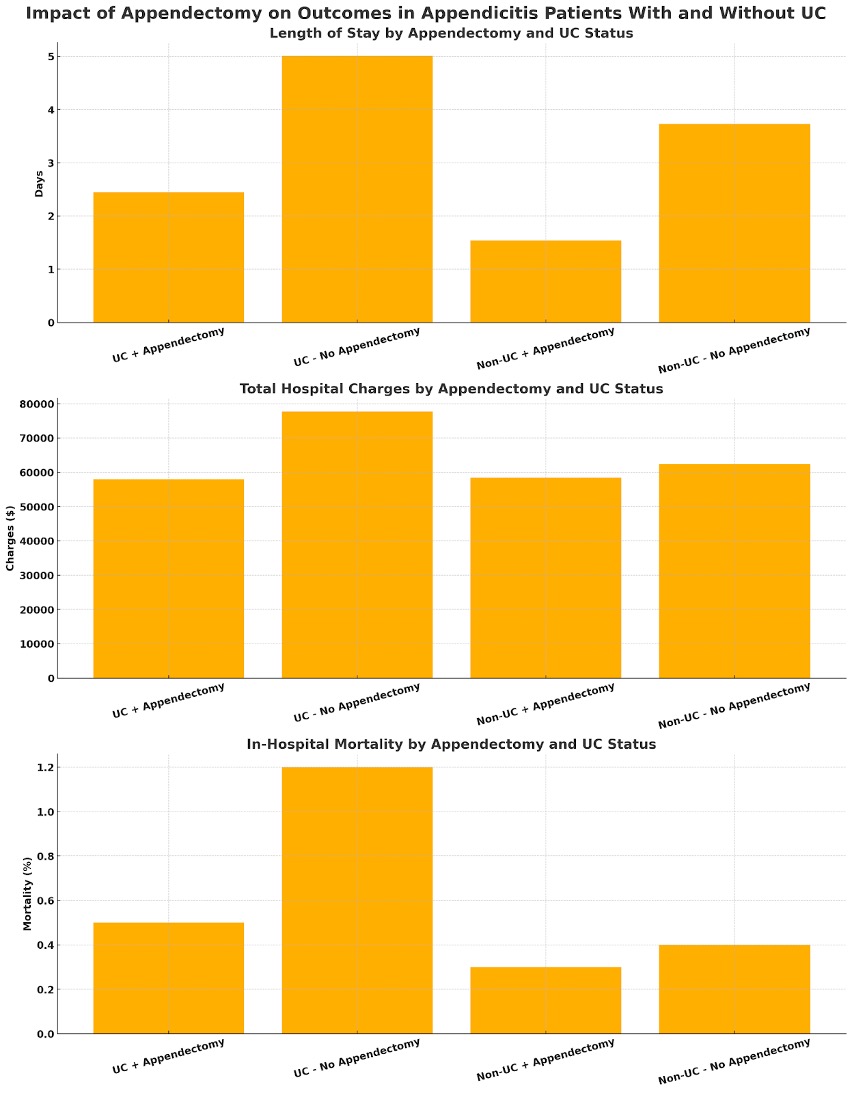
Figure: Impact of Appendectomy on Hospital Outcomes in Appendicitis Patients With and Without Ulcerative Colitis (UC):
This figure shows three key hospital outcomes — length of stay (LOS), total hospital charges, and in-hospital mortality — stratified by UC status and whether appendectomy was performed.
Top panel (LOS): Patients with UC who underwent appendectomy had a shorter mean hospital stay (~2.5 days) compared to UC patients without appendectomy (~5 days). A similar pattern was observed in non-UC patients, with appendectomy reducing LOS from ~3.8 to ~1.5 days.
Middle panel (Total Charges): Appendectomy was associated with lower hospital charges in both groups. UC patients with appendectomy had charges around $58,000, compared to ~$78,000 without appendectomy. Among non-UC patients, appendectomy reduced charges from ~$63,000 to ~$58,000.
Bottom panel (Mortality): In-hospital mortality was significantly lower in both groups when appendectomy was performed. UC patients without appendectomy had the highest mortality (~1.2%), while those with appendectomy dropped to ~0.5%. Non-UC patients showed a similar pattern, with mortality reduced from ~0.4% to ~0.25% following appendectomy.
Takeaway:
Appendectomy consistently improves hospital outcomes — reducing LOS, costs, and mortality — regardless of UC status. These findings reinforce the value of appendectomy even in the higher-risk UC population, challenging concerns about surgical risk in inflammatory bowel disease patients.

Figure: Table 1: ICD codes used to identify patients for appendectomy, ulcerative Colitis, appendicitis, and colectomy/ileocecectomy.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Meghana Kakarla indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Joseph Frasca, MD1, Zoe Post, MD, MSc1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1. P5398 - Appendectomy Improves Outcomes in Appendicitis Patients With and Without Ulcerative Colitis: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rush University Medical Center, Chicago, IL; 2Infirmary Health, Mobile, AL; 3Rush University Medical Center, Chicagoii, IL
Introduction: Ulcerative colitis (UC) is a chronic inflammatory bowel disease associated with increased healthcare utilization and surgical complexity. While appendectomy is a common and effective treatment for appendicitis, limited data exist on its impact in patients with coexisting UC. Given concerns about altered immune response and postoperative risk in UC, we aimed to assess whether appendectomy improves hospital outcomes in appendicitis patients with UC and how its effects compare to those without UC.
Methods: We conducted a retrospective cohort study using data from the National Inpatient Sample (NIS) from 2016–2019. We identified adult patients hospitalized with a principal diagnosis of appendicitis, excluding those who had undergone colectomy or ileocecectomy. Patients were stratified based on UC status. Multivariable linear and logistic regression models were used to evaluate the effect of appendectomy on three key outcomes: length of stay (LOS), total hospital charges (TOTCHG), and in-hospital mortality. Interaction terms were included to assess whether UC status modified the effect of appendectomy on these outcomes. All analyses accounted for demographic variables and hospital characteristics.
Results: We identified 141,349 hospitalized adults with appendicitis, including 505 (0.36%) with UC. Compared to non-UC patients, UC patients had worse outcomes: longer length of stay (LOS; 5.01 vs. 3.73 days), higher hospital charges ($77,723 vs. $62,460), and higher in-hospital mortality (1.2% vs. 0.4%, p = 0.008). In multivariable models, appendectomy was linked to shorter LOS and lower charges in both groups. Among UC patients, appendectomy reduced LOS by 2.56 days and charges by $19,738; among non-UC patients, it reduced LOS by 2.19 days and charges by $3,993 (all p < 0.05). Appendectomy significantly lowered overall in-hospital mortality (aOR = 0.19, p < 0.001). Although UC was independently associated with higher mortality, interaction terms showed that appendectomy’s benefits were consistent regardless of UC status.
Discussion: These findings support appendectomy as an effective intervention in appendicitis, including in UC patients. Despite worse baseline outcomes, UC patients saw significant reductions in LOS, charges, and mortality, similar to non-UC patients. This challenges concerns about surgical risk in UC and highlights appendectomy’s value in improving short-term outcomes. Further research is needed to assess long-term results and post-discharge complications in UC patients.
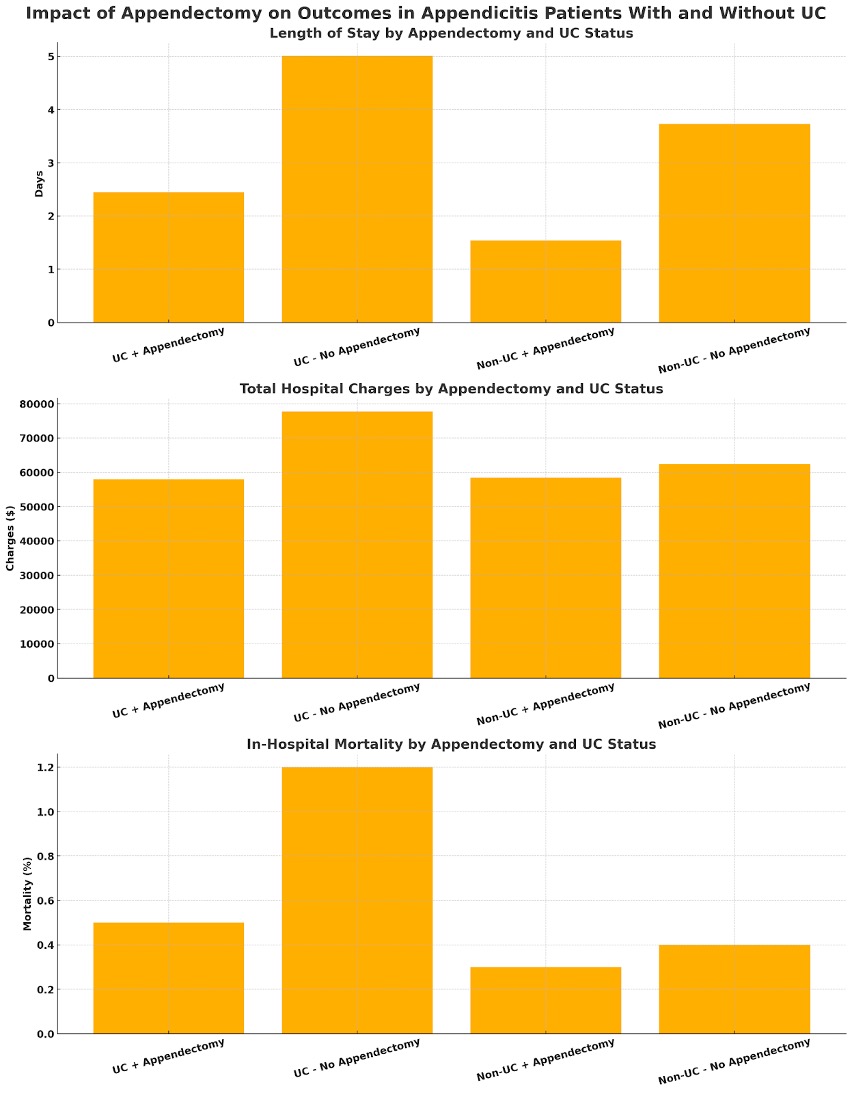
Figure: Impact of Appendectomy on Hospital Outcomes in Appendicitis Patients With and Without Ulcerative Colitis (UC):
This figure shows three key hospital outcomes — length of stay (LOS), total hospital charges, and in-hospital mortality — stratified by UC status and whether appendectomy was performed.
Top panel (LOS): Patients with UC who underwent appendectomy had a shorter mean hospital stay (~2.5 days) compared to UC patients without appendectomy (~5 days). A similar pattern was observed in non-UC patients, with appendectomy reducing LOS from ~3.8 to ~1.5 days.
Middle panel (Total Charges): Appendectomy was associated with lower hospital charges in both groups. UC patients with appendectomy had charges around $58,000, compared to ~$78,000 without appendectomy. Among non-UC patients, appendectomy reduced charges from ~$63,000 to ~$58,000.
Bottom panel (Mortality): In-hospital mortality was significantly lower in both groups when appendectomy was performed. UC patients without appendectomy had the highest mortality (~1.2%), while those with appendectomy dropped to ~0.5%. Non-UC patients showed a similar pattern, with mortality reduced from ~0.4% to ~0.25% following appendectomy.
Takeaway:
Appendectomy consistently improves hospital outcomes — reducing LOS, costs, and mortality — regardless of UC status. These findings reinforce the value of appendectomy even in the higher-risk UC population, challenging concerns about surgical risk in inflammatory bowel disease patients.

Figure: Table 1: ICD codes used to identify patients for appendectomy, ulcerative Colitis, appendicitis, and colectomy/ileocecectomy.
Disclosures:
Giovannie Isaac-Coss indicated no relevant financial relationships.
Meghana Kakarla indicated no relevant financial relationships.
Joseph Frasca indicated no relevant financial relationships.
Zoe Post indicated no relevant financial relationships.
Maham Lodhi indicated no relevant financial relationships.
Veena Nannegari indicated no relevant financial relationships.
Atsushi Sakuraba indicated no relevant financial relationships.
Giovannie Isaac-Coss, MD1, Meghana Kakarla, MD2, Joseph Frasca, MD1, Zoe Post, MD, MSc1, Maham Lodhi, MD1, Veena Nannegari, MD3, Atsushi Sakuraba, MD, PhD1. P5398 - Appendectomy Improves Outcomes in Appendicitis Patients With and Without Ulcerative Colitis: A Nationwide Inpatient Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
