Tuesday Poster Session
Category: IBD
P5386 - An Integrated IBD Sub-Fellowship Increases Competency in Caring for IBD Patients Without Extending Training Duration
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- FW
Franklyn Wallace, MD
University of Wisconsin Hospitals and Clinics
Madison, WI
Presenting Author(s)
Franklyn Wallace, MD1, Gabriela Lobato, MD, PhD1, Ian Grimes, MD, MS2
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2University of Wisconsin, Madison, WI
Introduction: With the rising prevalence of inflammatory bowel disease (IBD) and the rapid expansion of therapeutic options, there is an increasing need to train gastroenterologists with special expertise in IBD care. Although many programs offer advanced training in IBD after completion of a general gastroenterology (GI) fellowship, prior studies have demonstrated that increased duration of training is a major barrier to seeking additional training in IBD. We sought to investigate the impact of a novel approach to IBD training via a 6-month sub-fellowship integrated into the final year of GI fellowship.
Methods: A 15-item survey was sent to all graduates from the fellowship program from 2014-2024. Self-reported data were collected regarding experiences with IBD training during fellowship, comfort with entrusted professional activities (EPAs) for IBD providers and current practice patterns. Physicians who had completed the IBD sub-fellowship program were compared to those who had not. Continuous variables were compared using two-sample t-test and ordinal variables were compared using chi-square.
Results: There were 25 total survey responses including 8 fellows who completed the IBD sub-fellowship. Fellows who completed the IBD sub-fellowship reported better overall satisfaction with their exposure to IBD during fellowship and spent more time on both outpatient IBD management and IBD-related research during their fellowship (Table 1). Those who completed the IBD sub-fellowship reported increased competence across all 10 IBD EPAs (Table 2). Among those physicians who continued to regularly care for patients with IBD, former IBD sub-fellows spend a significantly larger portion of their current clinical time to outpatient IBD care (50% versus 12%, p = < 0.05). Those who completed the IBD sub-fellowship also generally reported more frequent prescribing advanced therapy medications for management of IBD patients. There was no difference between the groups regarding sex, age, years in practice, practice setting, academic productivity or adenoma detection rate.
Discussion: Our study supports prior data suggesting that specific training in IBD improves physicians’ competence with caring for patients with IBD. In addition, we demonstrate that similar benefits can be achieved using a novel abbreviated 6 month program within the general GI fellowship. This approach eliminates the need to extend the duration of training, reducing the barrier to entry for individuals interested in developing expertise in IBD.
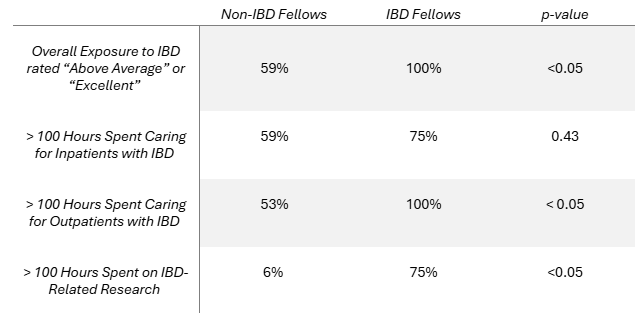
Figure: Table 1: Compared to those who did not complete the IBD sub-fellowship (n = 17), those who completed the IBD sub-fellowship (n = 8) reported significantly higher overall exposure to IBD during fellowship. IBD sub-fellows spent significantly more time on outpatient IBD cares and IBD-related research during their fellowship.
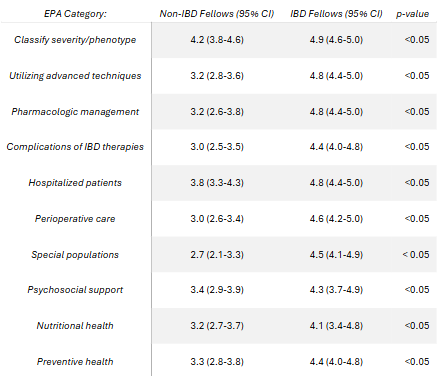
Figure: Table 2: Compared to those who did not complete the IBD sub-fellowship (n = 17), those who completed the IBD sub-fellowship (n = 8) reported significantly higher confidence with each of the 10 EPAs for IBD providers.
Disclosures:
Franklyn Wallace indicated no relevant financial relationships.
Gabriela Lobato indicated no relevant financial relationships.
Ian Grimes indicated no relevant financial relationships.
Franklyn Wallace, MD1, Gabriela Lobato, MD, PhD1, Ian Grimes, MD, MS2. P5386 - An Integrated IBD Sub-Fellowship Increases Competency in Caring for IBD Patients Without Extending Training Duration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Wisconsin Hospitals and Clinics, Madison, WI; 2University of Wisconsin, Madison, WI
Introduction: With the rising prevalence of inflammatory bowel disease (IBD) and the rapid expansion of therapeutic options, there is an increasing need to train gastroenterologists with special expertise in IBD care. Although many programs offer advanced training in IBD after completion of a general gastroenterology (GI) fellowship, prior studies have demonstrated that increased duration of training is a major barrier to seeking additional training in IBD. We sought to investigate the impact of a novel approach to IBD training via a 6-month sub-fellowship integrated into the final year of GI fellowship.
Methods: A 15-item survey was sent to all graduates from the fellowship program from 2014-2024. Self-reported data were collected regarding experiences with IBD training during fellowship, comfort with entrusted professional activities (EPAs) for IBD providers and current practice patterns. Physicians who had completed the IBD sub-fellowship program were compared to those who had not. Continuous variables were compared using two-sample t-test and ordinal variables were compared using chi-square.
Results: There were 25 total survey responses including 8 fellows who completed the IBD sub-fellowship. Fellows who completed the IBD sub-fellowship reported better overall satisfaction with their exposure to IBD during fellowship and spent more time on both outpatient IBD management and IBD-related research during their fellowship (Table 1). Those who completed the IBD sub-fellowship reported increased competence across all 10 IBD EPAs (Table 2). Among those physicians who continued to regularly care for patients with IBD, former IBD sub-fellows spend a significantly larger portion of their current clinical time to outpatient IBD care (50% versus 12%, p = < 0.05). Those who completed the IBD sub-fellowship also generally reported more frequent prescribing advanced therapy medications for management of IBD patients. There was no difference between the groups regarding sex, age, years in practice, practice setting, academic productivity or adenoma detection rate.
Discussion: Our study supports prior data suggesting that specific training in IBD improves physicians’ competence with caring for patients with IBD. In addition, we demonstrate that similar benefits can be achieved using a novel abbreviated 6 month program within the general GI fellowship. This approach eliminates the need to extend the duration of training, reducing the barrier to entry for individuals interested in developing expertise in IBD.
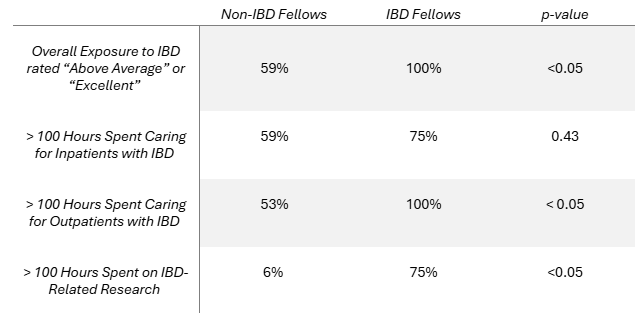
Figure: Table 1: Compared to those who did not complete the IBD sub-fellowship (n = 17), those who completed the IBD sub-fellowship (n = 8) reported significantly higher overall exposure to IBD during fellowship. IBD sub-fellows spent significantly more time on outpatient IBD cares and IBD-related research during their fellowship.
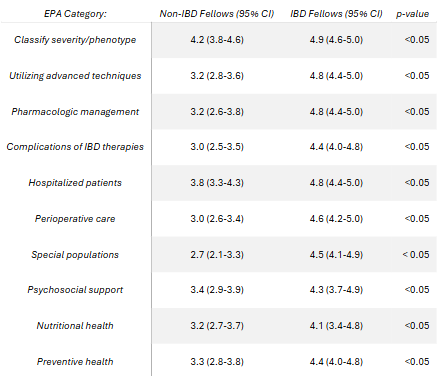
Figure: Table 2: Compared to those who did not complete the IBD sub-fellowship (n = 17), those who completed the IBD sub-fellowship (n = 8) reported significantly higher confidence with each of the 10 EPAs for IBD providers.
Disclosures:
Franklyn Wallace indicated no relevant financial relationships.
Gabriela Lobato indicated no relevant financial relationships.
Ian Grimes indicated no relevant financial relationships.
Franklyn Wallace, MD1, Gabriela Lobato, MD, PhD1, Ian Grimes, MD, MS2. P5386 - An Integrated IBD Sub-Fellowship Increases Competency in Caring for IBD Patients Without Extending Training Duration, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
