Tuesday Poster Session
Category: IBD
P5367 - Impact of Metabolic Syndrome on Clinical Outcomes and Healthcare Utilization in Hospitalized Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ryan Njeim, MD (he/him/his)
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Metabolic syndrome (MetS) can affect the course of inflammatory bowel disease (IBD) as its associated comorbidities could increase risk of adverse events including but not limited to cardiovascular disease. However, the impact of MetS on hospitalized IBD patients remains underexplored. We aim to assess the effect of MetS in IBD patients on their hospital course and discharge outcomes.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample database 2016-2020. Patients with IBD, hypertension, diabetes, dyslipidemia, and obesity were identified using ICD-10 codes. By assigning 1 point to each metabolic risk factor, a combined metabolic score (CMS) was calculated and a score >2 was diagnostic for MetS. Our desired outcomes included hospital mortality, length of stay, vasopressor use, intubation, central line insertion, number of any procedure and discharge disposition. Univariate and multivariate analysis were conducted using SAS 9.4.
Results: Among 1,246,470 IBD patients, 118,780 had MetS. When compared to the control group (IBD only), IBD patients with MetS were significantly older (63.8 vs 52.3 years), more likely to be female (59.8% vs 55.5%), white (80.6% vs 77.1%), on Medicare (58.3% vs 32.2%) and reside in lower-income ZIP codes (28.2% vs 24.5%). Their hospitalizations were associated with longer length of stay (5.77 vs 5.3 days), higher utilization of intensive care resources such as intubation (3.9% vs 2.3%), central line use (1.4% vs 0.9%) and higher likelihood of discharge to skilled nursing facilities (17.6% vs 8.3%) or home health services (20.1% vs 12.7%). All p values were < 0.001. (Table 1)
While adjusting for sociodemographic variables, CMS was associated with worse clinical outcomes. Compared to CMS 0, a score of 3-4 was significantly associated with higher odds of intubation (OR 1.263 [1.03-1.55]), central line insertion (OR 1.34 [1.06-1.68]) and inpatient mortality (OR 1.54 [1.34-1.77]). Moreover, a score of 1-2 was associated with higher vasopressor use (OR 1.15 [1.03-1.29]) (Table 2). Similarly, individual metabolic factors were associated with worse clinical outcomes and were included in Table 2.
Discussion: Hospitalized IBD patients with MetS had a more complex hospital course, increased healthcare resources utilization and worse clinical outcomes than those without MetS. This study highlights the importance of early diagnosis and management of MetS in IBD patients to optimize outcomes and reduce healthcare burden.
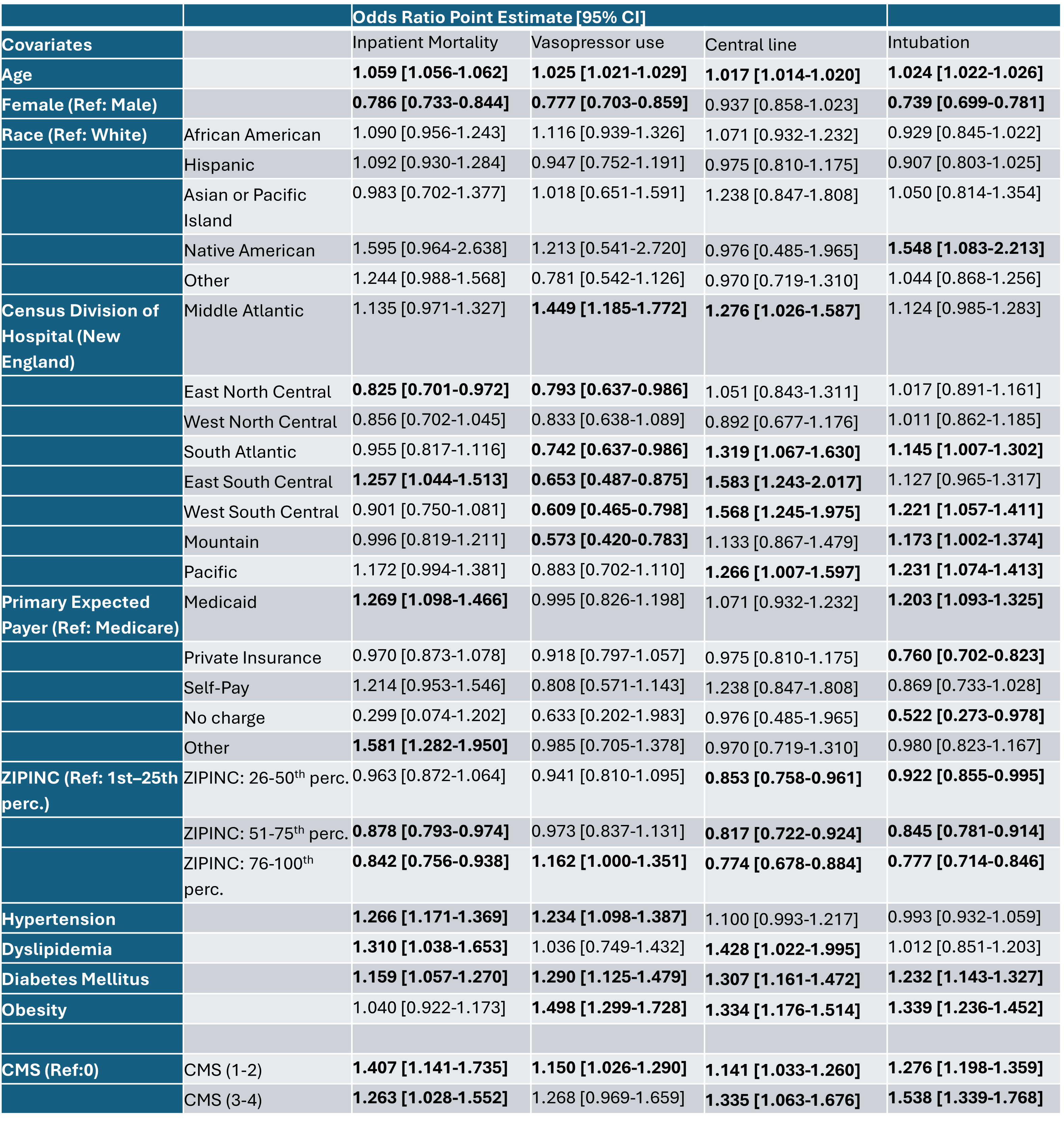
Figure: Table 1: Comparison of demographics, comorbidities and hospital outcomes among patients with inflammatory bowel disease by metabolic syndrome status
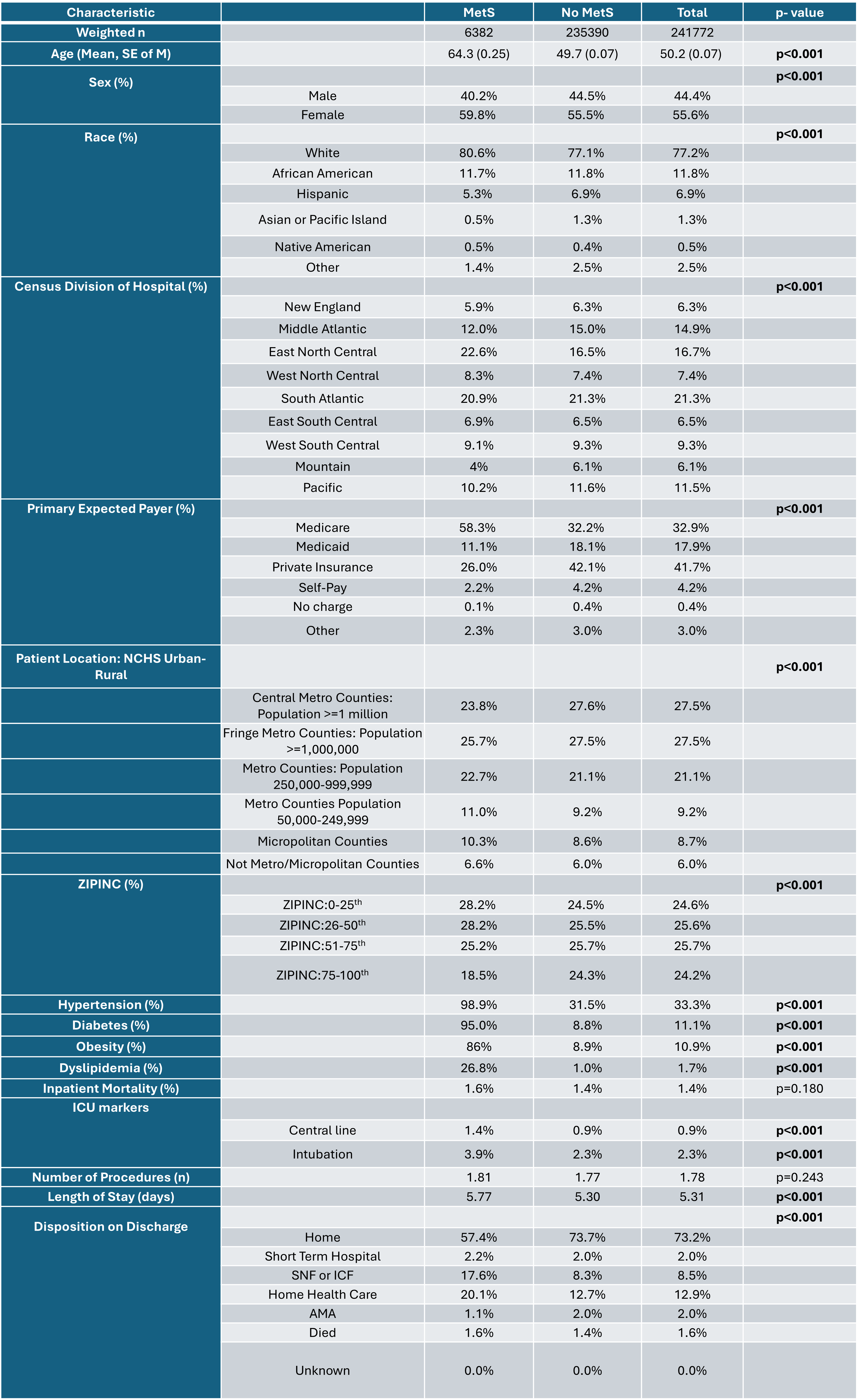
Figure: Table 2: Association between various hospital outcomes and metabolic factors in patients with inflammatory bowel disease, adjusted for sociodemographic factors.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD. P5367 - Impact of Metabolic Syndrome on Clinical Outcomes and Healthcare Utilization in Hospitalized Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: Metabolic syndrome (MetS) can affect the course of inflammatory bowel disease (IBD) as its associated comorbidities could increase risk of adverse events including but not limited to cardiovascular disease. However, the impact of MetS on hospitalized IBD patients remains underexplored. We aim to assess the effect of MetS in IBD patients on their hospital course and discharge outcomes.
Methods: A retrospective cohort study was conducted using the National Inpatient Sample database 2016-2020. Patients with IBD, hypertension, diabetes, dyslipidemia, and obesity were identified using ICD-10 codes. By assigning 1 point to each metabolic risk factor, a combined metabolic score (CMS) was calculated and a score >2 was diagnostic for MetS. Our desired outcomes included hospital mortality, length of stay, vasopressor use, intubation, central line insertion, number of any procedure and discharge disposition. Univariate and multivariate analysis were conducted using SAS 9.4.
Results: Among 1,246,470 IBD patients, 118,780 had MetS. When compared to the control group (IBD only), IBD patients with MetS were significantly older (63.8 vs 52.3 years), more likely to be female (59.8% vs 55.5%), white (80.6% vs 77.1%), on Medicare (58.3% vs 32.2%) and reside in lower-income ZIP codes (28.2% vs 24.5%). Their hospitalizations were associated with longer length of stay (5.77 vs 5.3 days), higher utilization of intensive care resources such as intubation (3.9% vs 2.3%), central line use (1.4% vs 0.9%) and higher likelihood of discharge to skilled nursing facilities (17.6% vs 8.3%) or home health services (20.1% vs 12.7%). All p values were < 0.001. (Table 1)
While adjusting for sociodemographic variables, CMS was associated with worse clinical outcomes. Compared to CMS 0, a score of 3-4 was significantly associated with higher odds of intubation (OR 1.263 [1.03-1.55]), central line insertion (OR 1.34 [1.06-1.68]) and inpatient mortality (OR 1.54 [1.34-1.77]). Moreover, a score of 1-2 was associated with higher vasopressor use (OR 1.15 [1.03-1.29]) (Table 2). Similarly, individual metabolic factors were associated with worse clinical outcomes and were included in Table 2.
Discussion: Hospitalized IBD patients with MetS had a more complex hospital course, increased healthcare resources utilization and worse clinical outcomes than those without MetS. This study highlights the importance of early diagnosis and management of MetS in IBD patients to optimize outcomes and reduce healthcare burden.
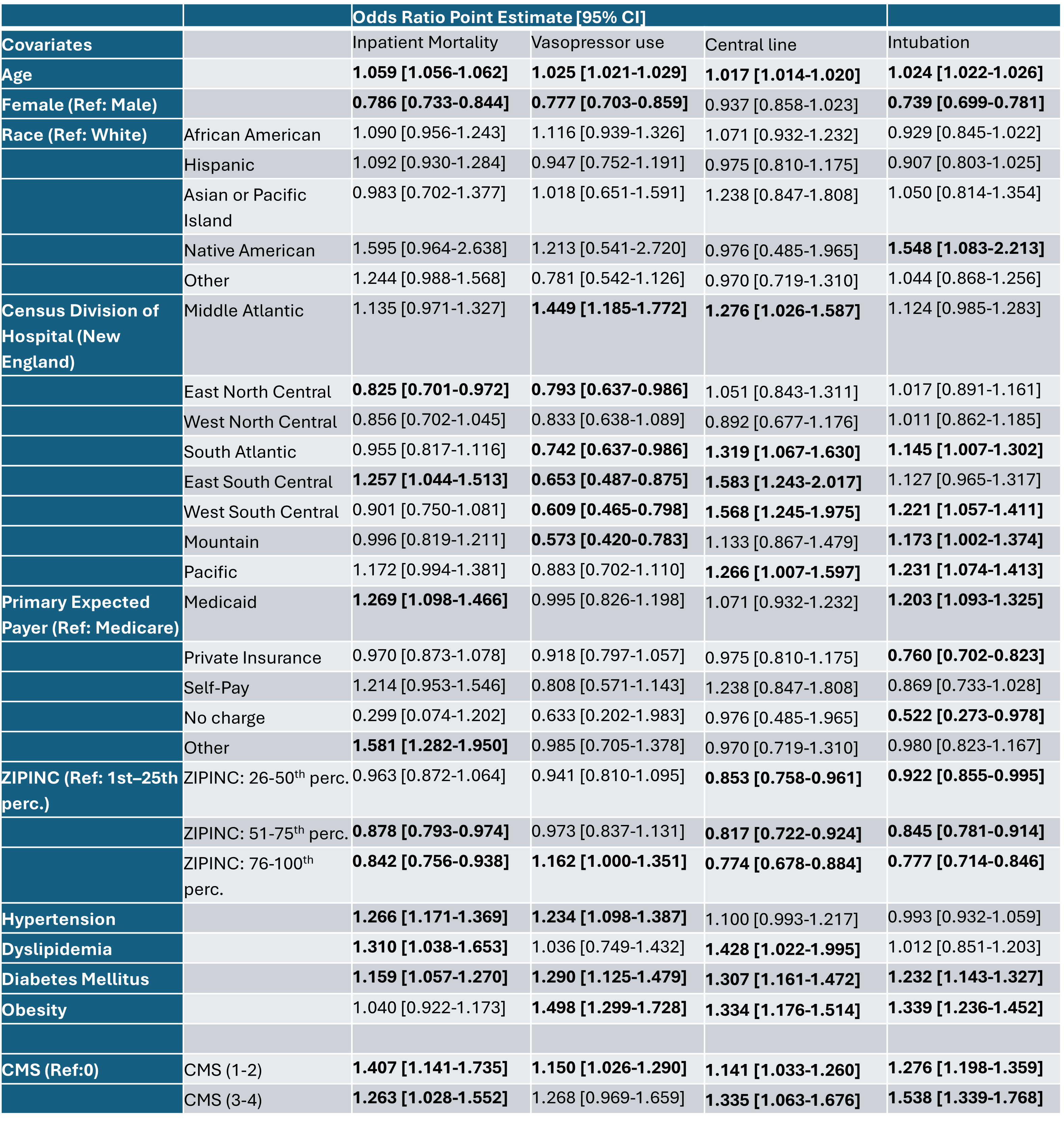
Figure: Table 1: Comparison of demographics, comorbidities and hospital outcomes among patients with inflammatory bowel disease by metabolic syndrome status
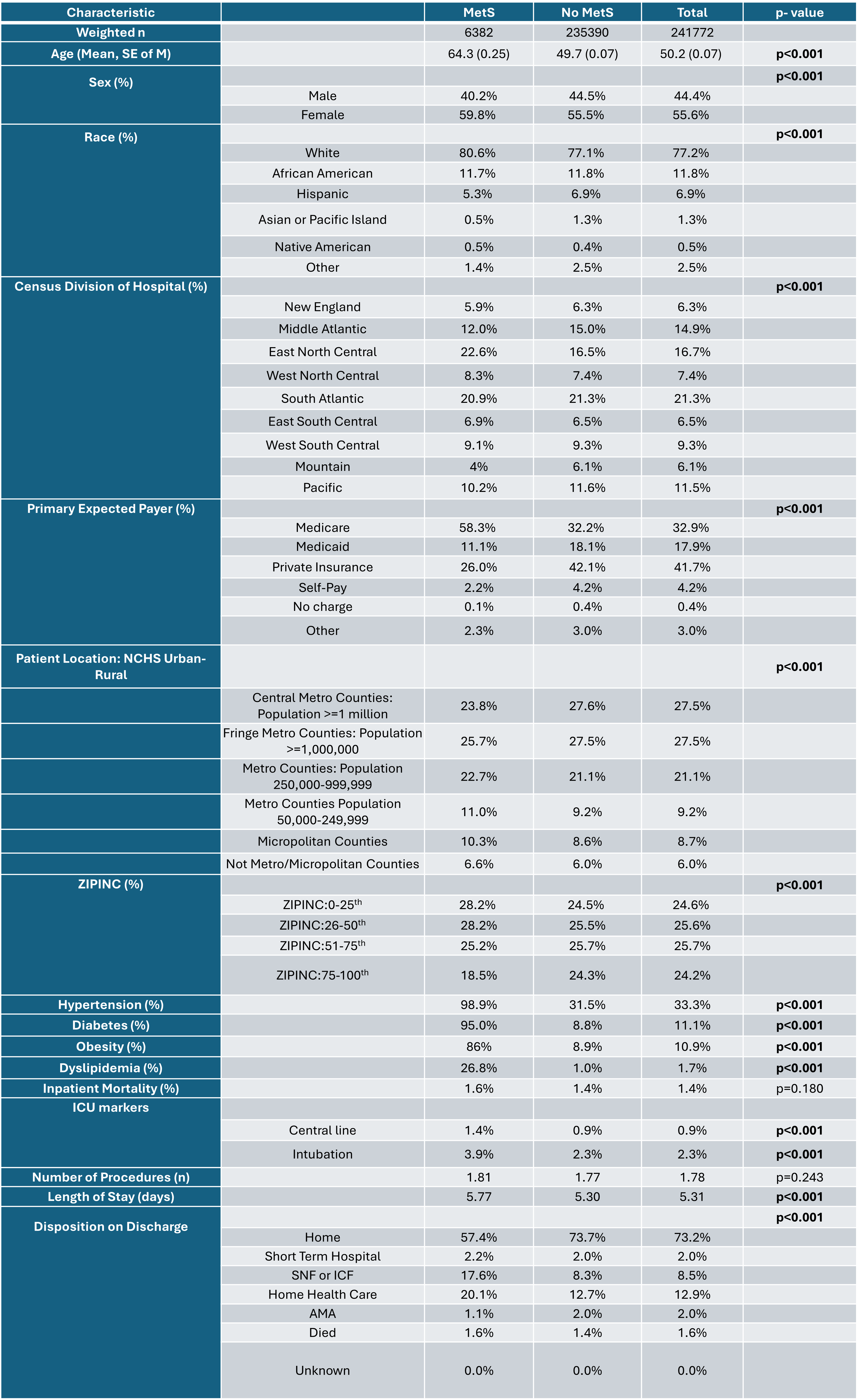
Figure: Table 2: Association between various hospital outcomes and metabolic factors in patients with inflammatory bowel disease, adjusted for sociodemographic factors.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD. P5367 - Impact of Metabolic Syndrome on Clinical Outcomes and Healthcare Utilization in Hospitalized Patients With Inflammatory Bowel Disease: A National Inpatient Sample Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
