Tuesday Poster Session
Category: IBD
P5366 - Metabolic Syndrome Predicts Worse Outcomes in Ulcerative Colitis Hospitalizations: A National Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Ryan Njeim, MD (he/him/his)
Staten Island University Hospital, Northwell Health
Staten Island, NY
Presenting Author(s)
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: A recent study has found that patients with inflammatory bowel disease (IBD) and metabolic comorbidities had a higher risk of recurrent hospitalizations. However, the effect of metabolic syndrome (MetS) on hospitalized ulcerative colitis (UC) patients has not been well studied. We aim to assess the effect of MetS in UC patients on their hospital-related outcomes.
Methods: We used the National Inpatient Sample database 2016-2020 to conduct a retrospective cohort study. ICD-10 codes were used to identify all patients with UC, and if they had hypertension (HTN), dyslipidemia (DL), diabetes mellitus (DM) or obesity. A combined metabolic score (CMS) was calculated by assigning 1 point to each of the 4 comorbidities. A score >2 was diagnostic for MetS. Our desired outcomes included hospital mortality, length of stay, vasopressor use, intubation, central line insertion, number of any procedure performed, and discharge disposition. Univariate and multivariate analysis were conducted using SAS 9.4
Results: Among 88,517 hospitalized UC patients, 2.96% had MetS. MetS patients were significantly older (62 vs 48.1 years old), likely to be females (55.9% vs 53.7%) and white (80.2% vs 75.4%). They presented mostly from rural areas (16.7% vs 13.3%), had lower economic status and were covered by Medicare (59.5% vs 31.9%). These patients had a longer hospital stay (6.07 vs 5.57 days), higher intubation (4% vs 2.6%) and central line insertion rates (1.5% vs 0.9%). They were more likely to be discharged to a skilled nursing facility (20.5% vs 9.6%) rather than to home (54.7% vs 72.3%). All p values were < 0.05.
Multivariate analyses for inpatient mortality, intubation, central line and vasopressor use are detailed in Table 1. A CMS=1-2 was not significantly associated with any of the 4 outcomes while a score of 3-4 had only higher odds of intubation (Odds ratio (OR) 1.32). DL was not associated with any of the 4 outcomes while DM and obesity were associated with intubation (OR 1.23 and 1.34) and central line use (OR1.29 and 1.37). Hospital mortality was associated with the presence of HTN and DM (OR 1.30 and OR 1.22).
Discussion: UC patients with metabolic comorbidities had a more complicated hospital course, higher mortality rates and worse outcomes on discharge compared to non-MetS UC patients. Our findings suggest a predicted need for strict and improved management of metabolic conditions in UC patients in order to mitigate complicated hospital outcomes.
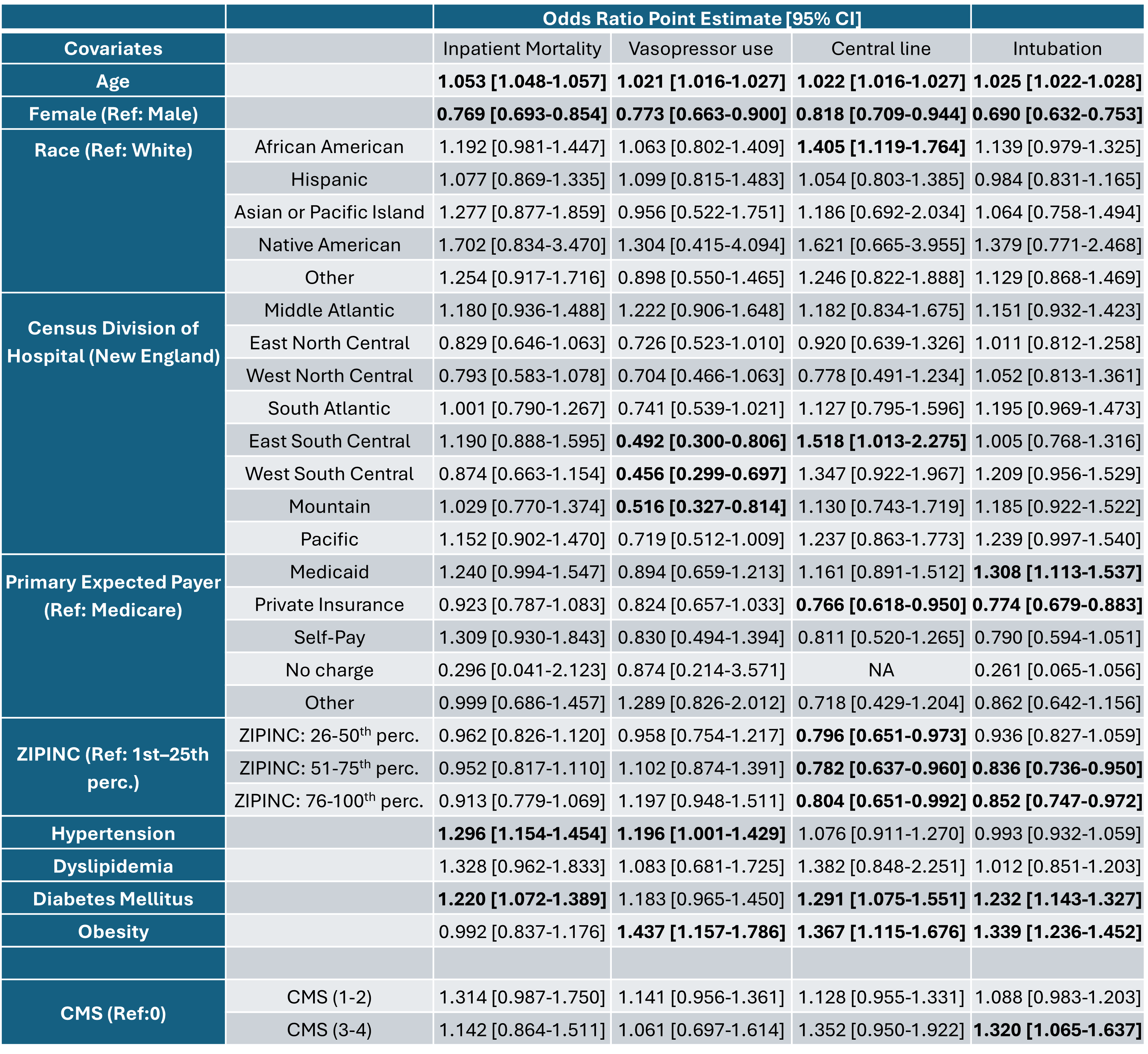
Figure: Table 1: Association between hospital outcomes and metabolic factors in patients with ulcerative colitis, adjusted for sociodemographic factors.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD. P5366 - Metabolic Syndrome Predicts Worse Outcomes in Ulcerative Colitis Hospitalizations: A National Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Staten Island University Hospital, Northwell Health, Staten Island, NY
Introduction: A recent study has found that patients with inflammatory bowel disease (IBD) and metabolic comorbidities had a higher risk of recurrent hospitalizations. However, the effect of metabolic syndrome (MetS) on hospitalized ulcerative colitis (UC) patients has not been well studied. We aim to assess the effect of MetS in UC patients on their hospital-related outcomes.
Methods: We used the National Inpatient Sample database 2016-2020 to conduct a retrospective cohort study. ICD-10 codes were used to identify all patients with UC, and if they had hypertension (HTN), dyslipidemia (DL), diabetes mellitus (DM) or obesity. A combined metabolic score (CMS) was calculated by assigning 1 point to each of the 4 comorbidities. A score >2 was diagnostic for MetS. Our desired outcomes included hospital mortality, length of stay, vasopressor use, intubation, central line insertion, number of any procedure performed, and discharge disposition. Univariate and multivariate analysis were conducted using SAS 9.4
Results: Among 88,517 hospitalized UC patients, 2.96% had MetS. MetS patients were significantly older (62 vs 48.1 years old), likely to be females (55.9% vs 53.7%) and white (80.2% vs 75.4%). They presented mostly from rural areas (16.7% vs 13.3%), had lower economic status and were covered by Medicare (59.5% vs 31.9%). These patients had a longer hospital stay (6.07 vs 5.57 days), higher intubation (4% vs 2.6%) and central line insertion rates (1.5% vs 0.9%). They were more likely to be discharged to a skilled nursing facility (20.5% vs 9.6%) rather than to home (54.7% vs 72.3%). All p values were < 0.05.
Multivariate analyses for inpatient mortality, intubation, central line and vasopressor use are detailed in Table 1. A CMS=1-2 was not significantly associated with any of the 4 outcomes while a score of 3-4 had only higher odds of intubation (Odds ratio (OR) 1.32). DL was not associated with any of the 4 outcomes while DM and obesity were associated with intubation (OR 1.23 and 1.34) and central line use (OR1.29 and 1.37). Hospital mortality was associated with the presence of HTN and DM (OR 1.30 and OR 1.22).
Discussion: UC patients with metabolic comorbidities had a more complicated hospital course, higher mortality rates and worse outcomes on discharge compared to non-MetS UC patients. Our findings suggest a predicted need for strict and improved management of metabolic conditions in UC patients in order to mitigate complicated hospital outcomes.
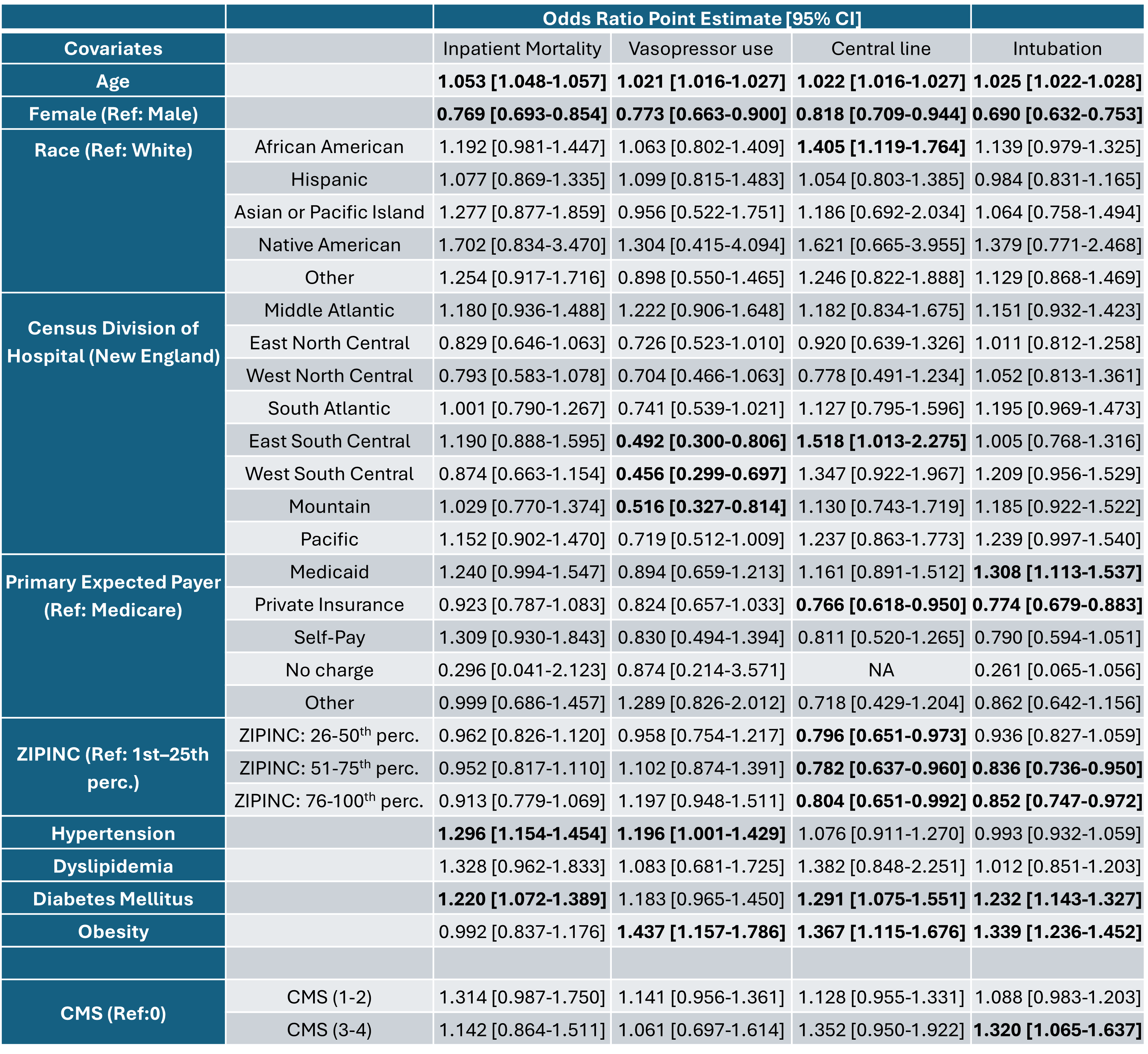
Figure: Table 1: Association between hospital outcomes and metabolic factors in patients with ulcerative colitis, adjusted for sociodemographic factors.
Disclosures:
Ryan Njeim indicated no relevant financial relationships.
Chapman Wei indicated no relevant financial relationships.
Elie Moussa indicated no relevant financial relationships.
Joelle Sleiman indicated no relevant financial relationships.
Liliane Deeb indicated no relevant financial relationships.
Ryan Njeim, MD, Chapman Wei, MD, Elie Moussa, MD, Joelle Sleiman, MD, Liliane Deeb, MD. P5366 - Metabolic Syndrome Predicts Worse Outcomes in Ulcerative Colitis Hospitalizations: A National Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
