Tuesday Poster Session
Category: IBD
P5363 - The Mediterranean Diet and Inflammatory Bowel Disease: A Comprehensive Systematic Review and Meta-Analysis of Efficacy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Muhammad Shahzil, MD
Penn State Health Milton S. Hershey Medical Center
Hershey, PA
Presenting Author(s)
Muhammad Shahzil, MD1, Syeda Kanza Kazmi, MD1, Minahel Shehzadi, MBBS2, Fariha Hasan, MD3, Muhammad Saad Faisal, MD4, Anza Muhammad, MBBS2, Ammad Javaid. Chaudhary, MD4, Justin Canakis, DO1, Kofi Clarke, MD1
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Cooper University Health Care, Camden, NJ; 4Henry Ford Health, Detroit, MI
Introduction: Environmental and dietary factors significantly influence the development and progression of inflammatory bowel disease (IBD). The Mediterranean diet (MD), characterized by high consumption of fruits, vegetables, healthy fats, lean proteins, and low intake of processed foods and sugars, is frequently recommended as adjunctive therapy. The American Gastroenterological Association includes MD in its guidelines for managing Crohn's disease (CD); however, the strength of the recommendation is low due to the DINE-CD trial, which did not demonstrate superiority of MD compared to the specific carbohydrate diet (SCD).
This meta-analysis aims to enhance current data by evaluating existing research on dietary management in ulcerative colitis (UC) and assessing the effectiveness of MD in achieving symptomatic remission or improvement in IBD patients compared to other dietary interventions.
Methods: Following Cochrane and PRISMA guidelines, randomized controlled trials (RCTs) comparing the MD to alternative dietary interventions in IBD patients were identified through comprehensive database searches up to October 2024. Data were analyzed using RevMan Web, employing a random-effects model.
Results: Four RCTs involving a total of 339 IBD patients were included in this analysis. Among these, 167 patients (including those with UC and CD) received the Mediterranean diet, while 172 followed non-Mediterranean diets (NMD). The MD was associated with a statistically significant improvement in clinical remission compared to NMD (RR 1.18, P = 0.02). When compared specifically to a regular diet, MD significantly reduced both CRP levels (MD -2.66, P < 0.00001) and fecal calprotectin (MD -229.46, P = 0.008). Specifically, within the UC population, MD significantly decreased CRP and fecal calprotectin levels.
Discussion: Our findings suggest the Mediterranean diet provides significant benefits in managing IBD, particularly for UC patients, as demonstrated by notable reductions in CRP and fecal calprotectin levels. However, similar benefits in patients with CD remain less clear despite previous evidence of symptomatic improvement.
Although MD shows superiority over regular diets, its relative advantage compared to other specialized diets, such as the SCD, remains uncertain. Variability among studies and adherence challenges complicate these comparisons. Future research should aim to identify specific patient subgroups most likely to benefit from MD and strategies to enhance adherence.
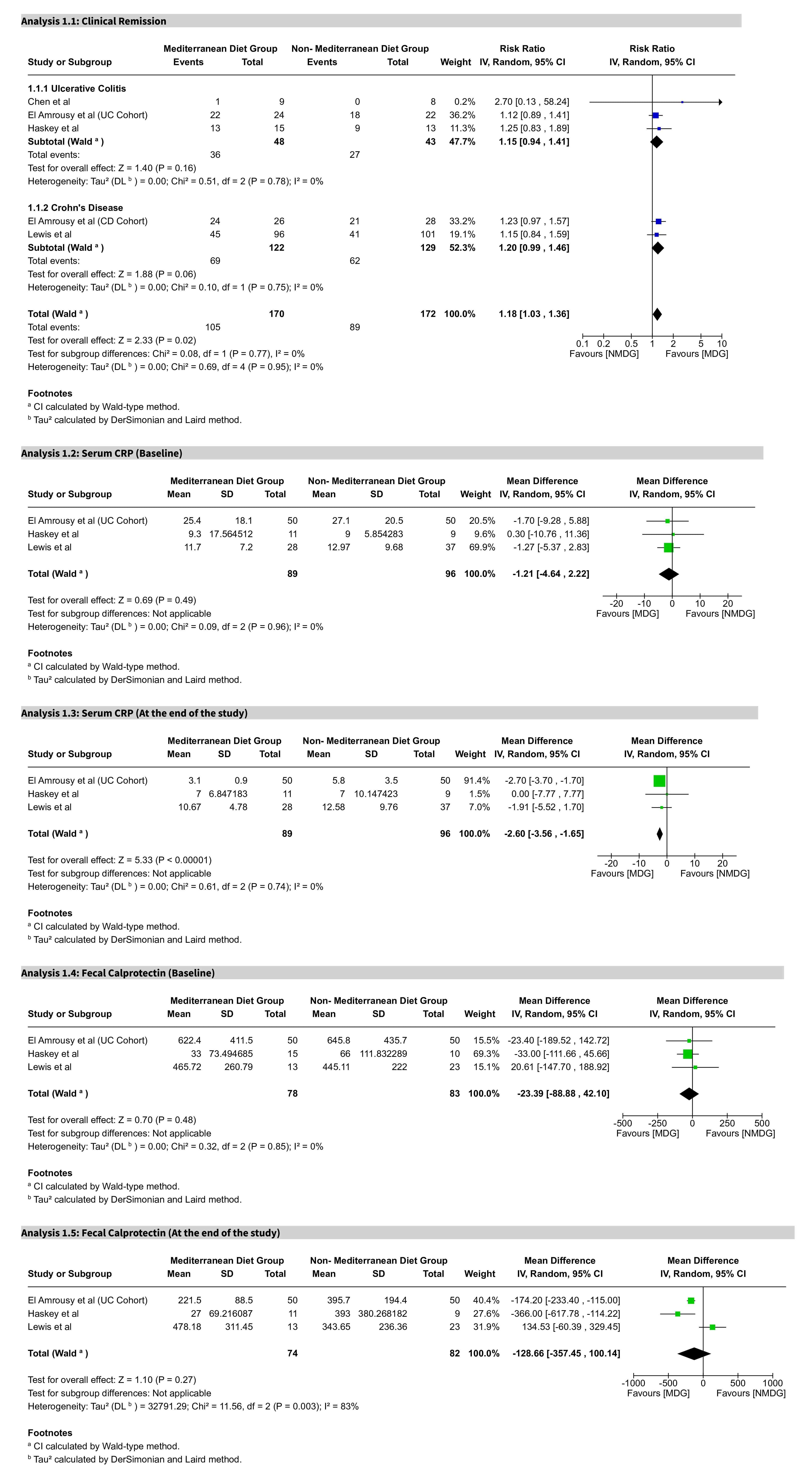
Figure: Figure 1. Forest plots comparing the Mediterranean Diet (MD) to non-Mediterranean diets (NMD) in patients with Inflammatory Bowel Disease (IBD).
(A) Clinical remission across ulcerative colitis (UC) and Crohn’s disease (CD) cohorts shows a significant benefit in favor of MD (RR 1.18, 95% CI [1.03, 1.36], P = 0.02).
(B) No significant difference in baseline serum CRP between MD and NMD groups (MD -1.21, 95% CI [-4.64, 2.22], P = 0.49).
(C) At study end, serum CRP was significantly lower in the MD group (MD -2.60, 95% CI [-3.56, -1.65], P < 0.00001).
(D) No significant baseline difference in fecal calprotectin between MD and NMD groups (MD -23.39, 95% CI [-88.88, 42.10], P = 0.48).
(E) At study end, fecal calprotectin was lower in the MD group, though with considerable heterogeneity (MD -128.66, 95% CI [-357.45, 100.14], P = 0.22).
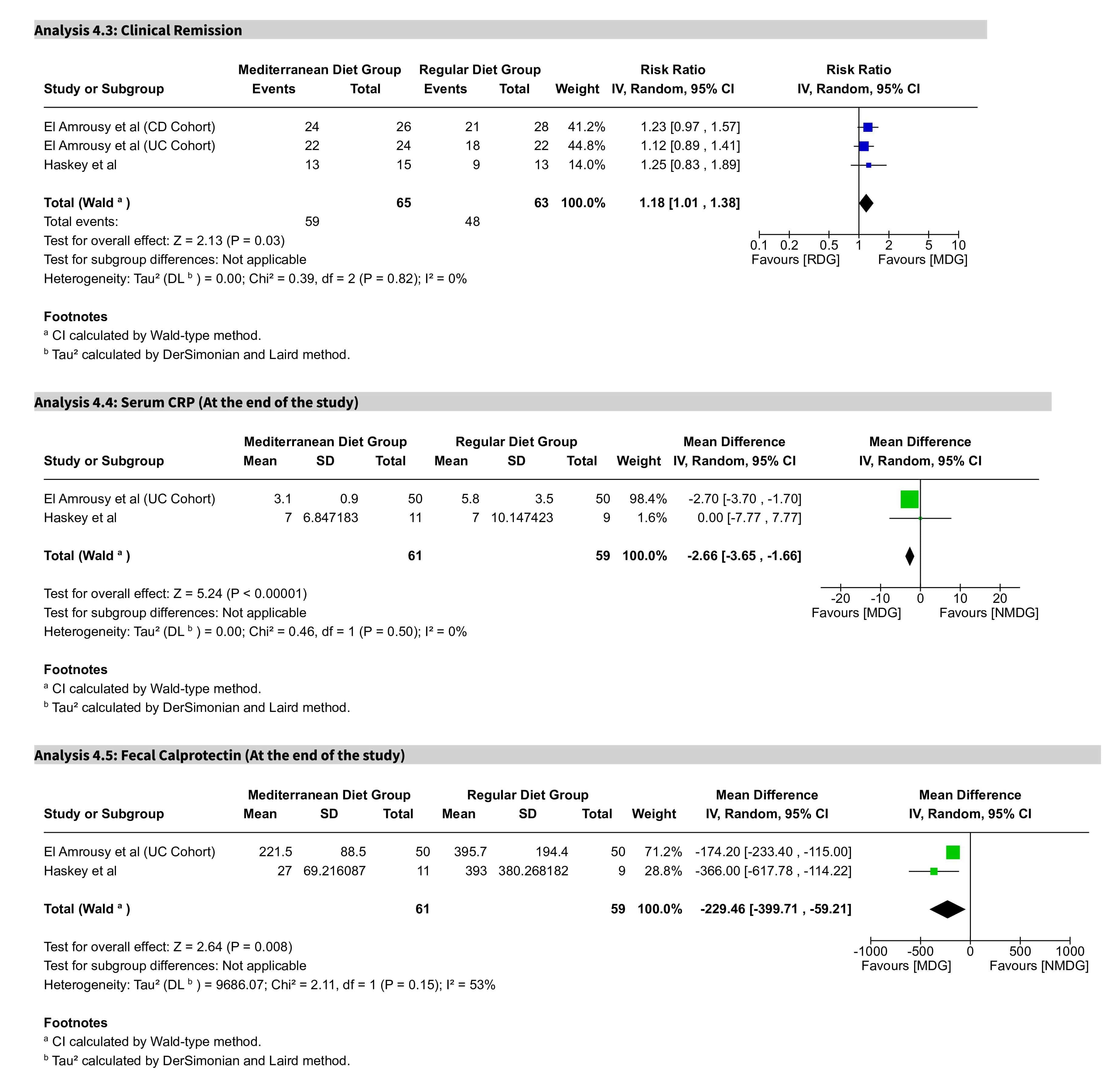
Figure: Figure 2. Subgroup analysis comparing the Mediterranean Diet (MD) to a regular diet (RD) in IBD patients.
(A) Clinical remission was significantly more likely in the MD group compared to RD (RR 1.18, 95% CI [1.01, 1.38], P = 0.03).
(B) At study end, serum CRP levels were significantly reduced in the MD group (MD -2.66, 95% CI [-3.65, -1.66], P < 0.00001).
(C) Fecal calprotectin levels were significantly lower in the MD group compared to RD (MD -229.46, 95% CI [-399.71, -59.21], P = 0.008).
Disclosures:
Muhammad Shahzil indicated no relevant financial relationships.
Syeda Kanza Kazmi indicated no relevant financial relationships.
Minahel Shehzadi indicated no relevant financial relationships.
Fariha Hasan indicated no relevant financial relationships.
Muhammad Saad Faisal indicated no relevant financial relationships.
Anza Muhammad indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Kofi Clarke: Takeda – Clinical Trial Support.
Muhammad Shahzil, MD1, Syeda Kanza Kazmi, MD1, Minahel Shehzadi, MBBS2, Fariha Hasan, MD3, Muhammad Saad Faisal, MD4, Anza Muhammad, MBBS2, Ammad Javaid. Chaudhary, MD4, Justin Canakis, DO1, Kofi Clarke, MD1. P5363 - The Mediterranean Diet and Inflammatory Bowel Disease: A Comprehensive Systematic Review and Meta-Analysis of Efficacy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Penn State Health Milton S. Hershey Medical Center, Hershey, PA; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Cooper University Health Care, Camden, NJ; 4Henry Ford Health, Detroit, MI
Introduction: Environmental and dietary factors significantly influence the development and progression of inflammatory bowel disease (IBD). The Mediterranean diet (MD), characterized by high consumption of fruits, vegetables, healthy fats, lean proteins, and low intake of processed foods and sugars, is frequently recommended as adjunctive therapy. The American Gastroenterological Association includes MD in its guidelines for managing Crohn's disease (CD); however, the strength of the recommendation is low due to the DINE-CD trial, which did not demonstrate superiority of MD compared to the specific carbohydrate diet (SCD).
This meta-analysis aims to enhance current data by evaluating existing research on dietary management in ulcerative colitis (UC) and assessing the effectiveness of MD in achieving symptomatic remission or improvement in IBD patients compared to other dietary interventions.
Methods: Following Cochrane and PRISMA guidelines, randomized controlled trials (RCTs) comparing the MD to alternative dietary interventions in IBD patients were identified through comprehensive database searches up to October 2024. Data were analyzed using RevMan Web, employing a random-effects model.
Results: Four RCTs involving a total of 339 IBD patients were included in this analysis. Among these, 167 patients (including those with UC and CD) received the Mediterranean diet, while 172 followed non-Mediterranean diets (NMD). The MD was associated with a statistically significant improvement in clinical remission compared to NMD (RR 1.18, P = 0.02). When compared specifically to a regular diet, MD significantly reduced both CRP levels (MD -2.66, P < 0.00001) and fecal calprotectin (MD -229.46, P = 0.008). Specifically, within the UC population, MD significantly decreased CRP and fecal calprotectin levels.
Discussion: Our findings suggest the Mediterranean diet provides significant benefits in managing IBD, particularly for UC patients, as demonstrated by notable reductions in CRP and fecal calprotectin levels. However, similar benefits in patients with CD remain less clear despite previous evidence of symptomatic improvement.
Although MD shows superiority over regular diets, its relative advantage compared to other specialized diets, such as the SCD, remains uncertain. Variability among studies and adherence challenges complicate these comparisons. Future research should aim to identify specific patient subgroups most likely to benefit from MD and strategies to enhance adherence.
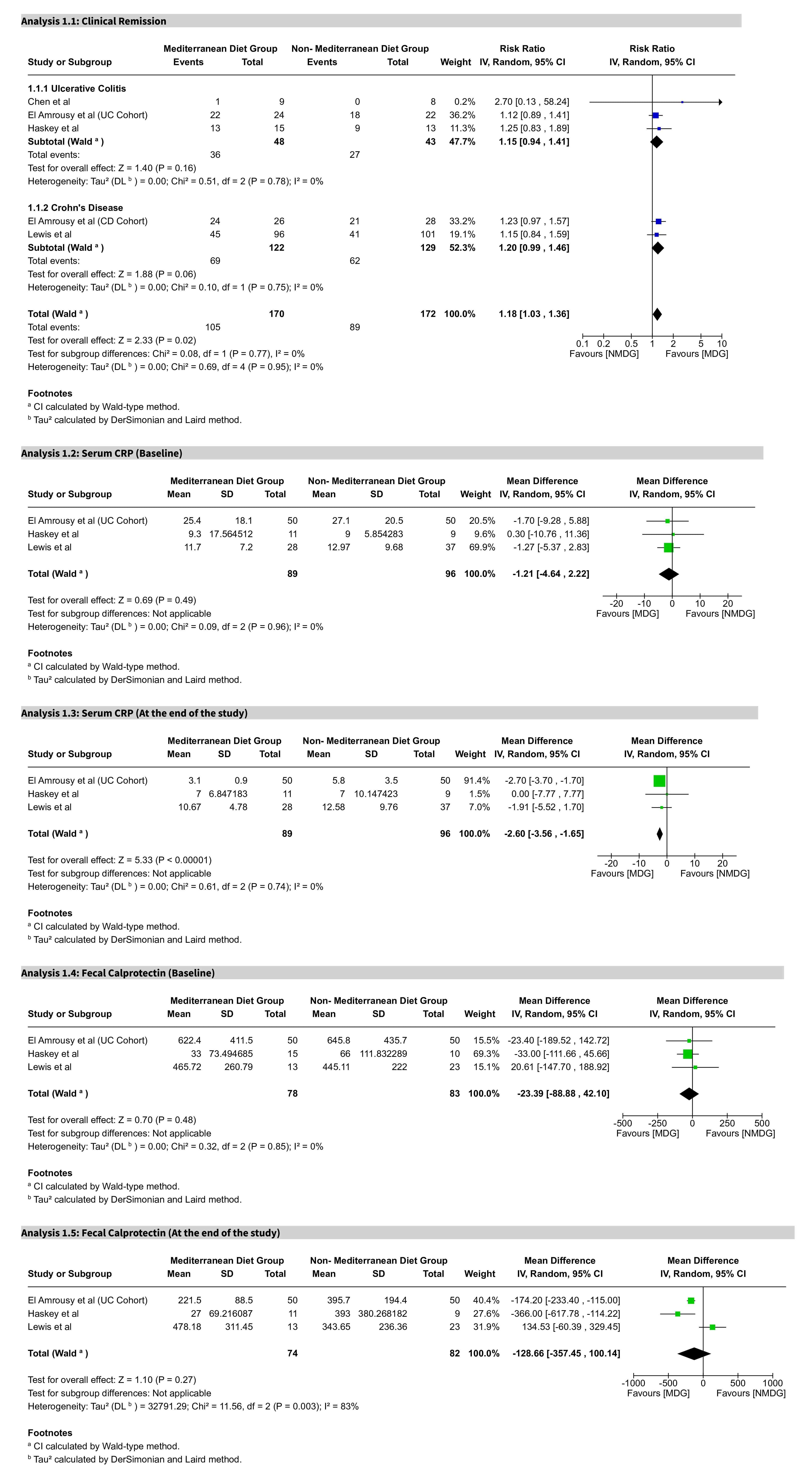
Figure: Figure 1. Forest plots comparing the Mediterranean Diet (MD) to non-Mediterranean diets (NMD) in patients with Inflammatory Bowel Disease (IBD).
(A) Clinical remission across ulcerative colitis (UC) and Crohn’s disease (CD) cohorts shows a significant benefit in favor of MD (RR 1.18, 95% CI [1.03, 1.36], P = 0.02).
(B) No significant difference in baseline serum CRP between MD and NMD groups (MD -1.21, 95% CI [-4.64, 2.22], P = 0.49).
(C) At study end, serum CRP was significantly lower in the MD group (MD -2.60, 95% CI [-3.56, -1.65], P < 0.00001).
(D) No significant baseline difference in fecal calprotectin between MD and NMD groups (MD -23.39, 95% CI [-88.88, 42.10], P = 0.48).
(E) At study end, fecal calprotectin was lower in the MD group, though with considerable heterogeneity (MD -128.66, 95% CI [-357.45, 100.14], P = 0.22).
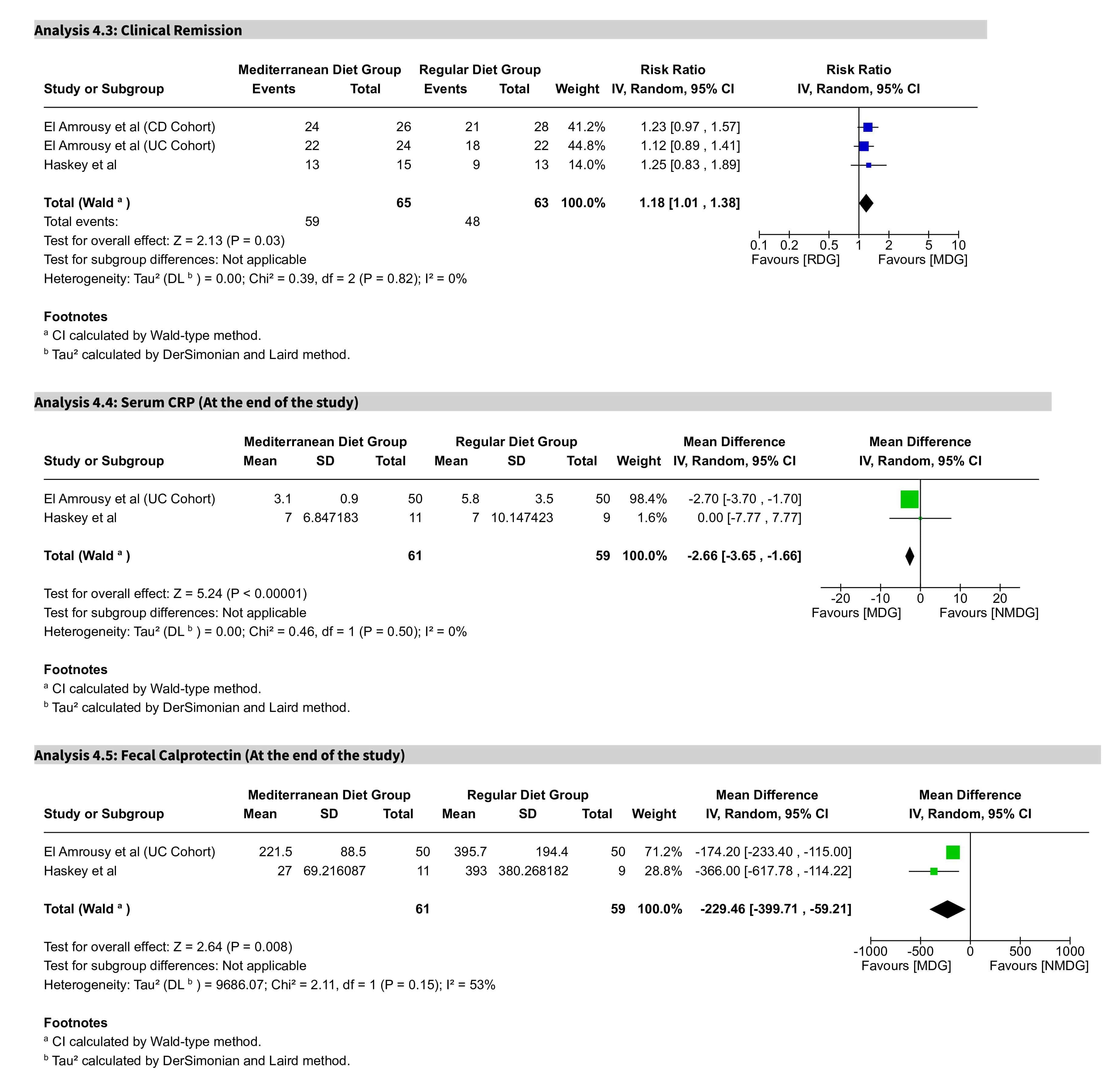
Figure: Figure 2. Subgroup analysis comparing the Mediterranean Diet (MD) to a regular diet (RD) in IBD patients.
(A) Clinical remission was significantly more likely in the MD group compared to RD (RR 1.18, 95% CI [1.01, 1.38], P = 0.03).
(B) At study end, serum CRP levels were significantly reduced in the MD group (MD -2.66, 95% CI [-3.65, -1.66], P < 0.00001).
(C) Fecal calprotectin levels were significantly lower in the MD group compared to RD (MD -229.46, 95% CI [-399.71, -59.21], P = 0.008).
Disclosures:
Muhammad Shahzil indicated no relevant financial relationships.
Syeda Kanza Kazmi indicated no relevant financial relationships.
Minahel Shehzadi indicated no relevant financial relationships.
Fariha Hasan indicated no relevant financial relationships.
Muhammad Saad Faisal indicated no relevant financial relationships.
Anza Muhammad indicated no relevant financial relationships.
Ammad Chaudhary indicated no relevant financial relationships.
Justin Canakis indicated no relevant financial relationships.
Kofi Clarke: Takeda – Clinical Trial Support.
Muhammad Shahzil, MD1, Syeda Kanza Kazmi, MD1, Minahel Shehzadi, MBBS2, Fariha Hasan, MD3, Muhammad Saad Faisal, MD4, Anza Muhammad, MBBS2, Ammad Javaid. Chaudhary, MD4, Justin Canakis, DO1, Kofi Clarke, MD1. P5363 - The Mediterranean Diet and Inflammatory Bowel Disease: A Comprehensive Systematic Review and Meta-Analysis of Efficacy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

