Tuesday Poster Session
Category: IBD
P5317 - Cannabis Use Disorder and Inpatient Outcomes in Crohn’s Disease Flares: A National Retrospective Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- SG
Shubham Gupta, MD
Virtua Health System
Philadelphia, PA
Presenting Author(s)
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Juan C. Santiago-Gonzalez, MD, MSc4, Mesay Asfaw, MD5, Farshad Aduli, MD4
1Department of Medicine, Howard University Hospital, Washington, DC; 2Virtua Health System, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 4Howard University Hospital, Washington, DC; 5Howard University, Washington, DC
Introduction: Crohn’s disease (CD) affects 200–250 per 100,000 U.S. adults and often leads to hospitalization during flares. Cannabis use is rising, especially among younger adults and those with inflammatory bowel disease (IBD), though its clinical significance remains uncertain. While cannabis may relieve symptoms like pain or anorexia, it has not been shown to reduce inflammation or improve long-term outcomes. Prior studies link cannabis use to more emergency visits and corticosteroid use, but inpatient outcomes remain poorly defined. This study assessed whether cannabis use disorder (CUD) is associated with hospitalization outcomes during CD flares.
Methods: We analyzed the 2020–2021 National Inpatient Sample to identify adult CD flare hospitalizations. CUD was defined by diagnosis. Primary outcomes were length of stay (LOS), total charges, in-hospital mortality, and bowel surgery. Secondary outcomes included depression, alcohol use disorder, and other psychiatric conditions. Comparisons between CUD and non-CUD groups used t-tests and chi-square tests. Multivariable logistic regression adjusted for age, sex, comorbidities, and insurance.
Results: Of 24,506 CD hospitalizations, 835 (4.2%) involved CUD. These patients were younger and had higher rates of depression (16.3% vs 14.9%, p< 0.001), alcohol use (3.7% vs 1.2%, p< 0.001), and other psychiatric conditions (27.2% vs 23.8%, p< 0.001). LOS was slightly shorter in the CUD group (4.6 vs 4.8 days, p=0.0045); charges and mortality were similar (p=0.33, p=0.29). Bowel surgery was less frequent (30.4% vs 37.2%, p< 0.001). In adjusted analysis (n=20,011), CUD was independently linked to lower odds of surgery (aOR=0.76, 95% CI: 0.66–0.89, p=0.0006). Alcohol use also predicted lower odds (aOR=0.78, p=0.040). Age, sex, and depression were not significant; private insurance was linked to higher odds. Charlson Comorbidity Index was similar (p=0.35).
Discussion: CUD was associated with lower bowel surgery rates and shorter LOS in hospitalized CD patients, without increased mortality or cost. These findings suggest cannabis use may influence hospitalization patterns but is not tied to worse outcomes. Although cannabis lacks anti-inflammatory effects, behavioral or care-related factors may explain these trends. Higher psychiatric comorbidity among CUD users highlights the need for integrated behavioral care. Understanding these associations may support risk stratification and multidisciplinary care in IBD.
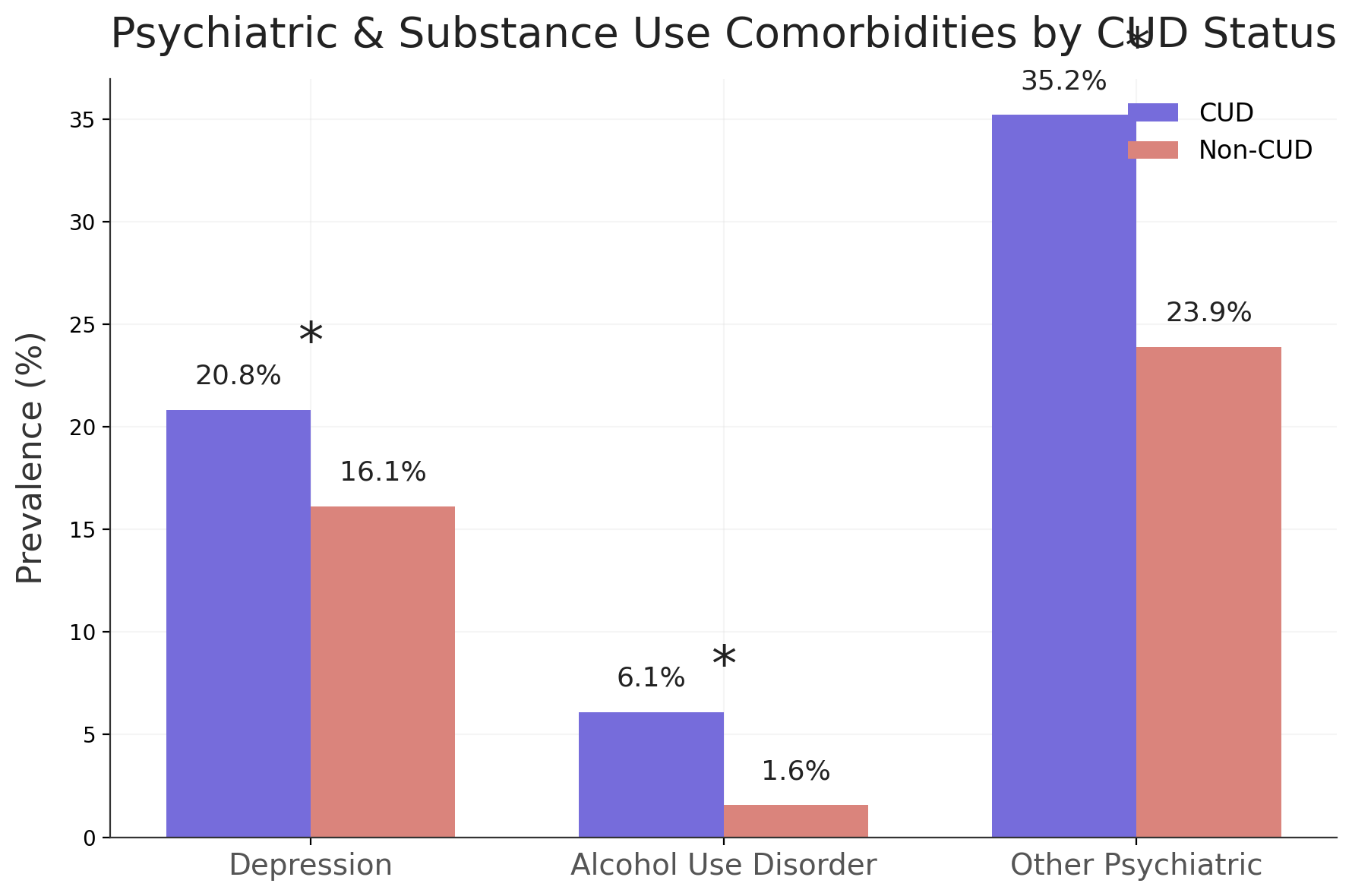
Figure: Figure 1. Comparison of inpatient outcomes—length of stay, hospital charges, and bowel surgery—among Crohn’s disease hospitalizations with vs without Cannabis Use Disorder.
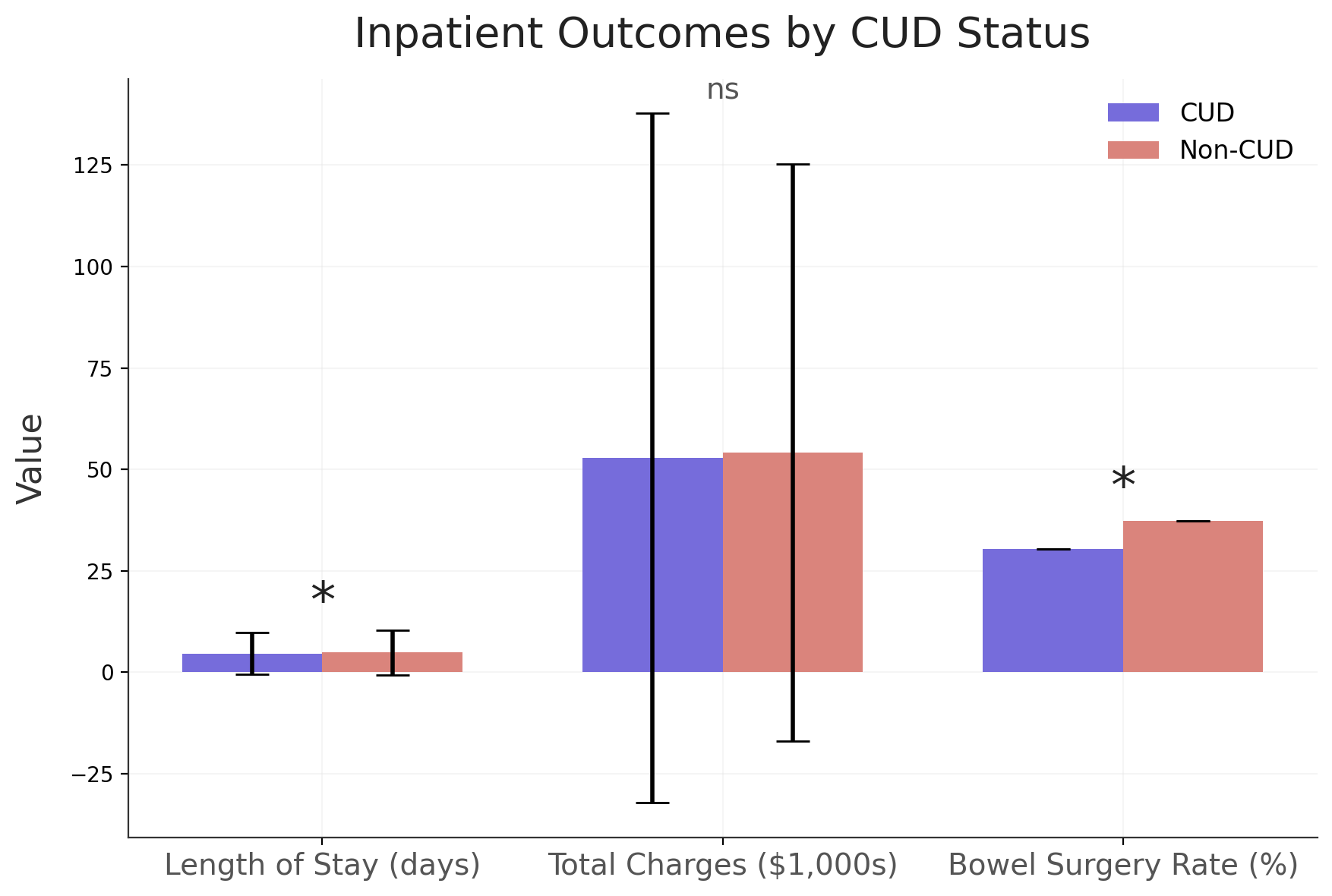
Figure: Figure 2. Prevalence of psychiatric and substance use comorbidities among Crohn’s disease hospitalizations, stratified by Cannabis Use Disorder status.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Shubham Gupta indicated no relevant financial relationships.
Shaunak Ganju indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Juan C. Santiago-Gonzalez, MD, MSc4, Mesay Asfaw, MD5, Farshad Aduli, MD4. P5317 - Cannabis Use Disorder and Inpatient Outcomes in Crohn’s Disease Flares: A National Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Medicine, Howard University Hospital, Washington, DC; 2Virtua Health System, Philadelphia, PA; 3Sidney Kimmel Medical College at Thomas Jefferson University, Philadelphia, PA; 4Howard University Hospital, Washington, DC; 5Howard University, Washington, DC
Introduction: Crohn’s disease (CD) affects 200–250 per 100,000 U.S. adults and often leads to hospitalization during flares. Cannabis use is rising, especially among younger adults and those with inflammatory bowel disease (IBD), though its clinical significance remains uncertain. While cannabis may relieve symptoms like pain or anorexia, it has not been shown to reduce inflammation or improve long-term outcomes. Prior studies link cannabis use to more emergency visits and corticosteroid use, but inpatient outcomes remain poorly defined. This study assessed whether cannabis use disorder (CUD) is associated with hospitalization outcomes during CD flares.
Methods: We analyzed the 2020–2021 National Inpatient Sample to identify adult CD flare hospitalizations. CUD was defined by diagnosis. Primary outcomes were length of stay (LOS), total charges, in-hospital mortality, and bowel surgery. Secondary outcomes included depression, alcohol use disorder, and other psychiatric conditions. Comparisons between CUD and non-CUD groups used t-tests and chi-square tests. Multivariable logistic regression adjusted for age, sex, comorbidities, and insurance.
Results: Of 24,506 CD hospitalizations, 835 (4.2%) involved CUD. These patients were younger and had higher rates of depression (16.3% vs 14.9%, p< 0.001), alcohol use (3.7% vs 1.2%, p< 0.001), and other psychiatric conditions (27.2% vs 23.8%, p< 0.001). LOS was slightly shorter in the CUD group (4.6 vs 4.8 days, p=0.0045); charges and mortality were similar (p=0.33, p=0.29). Bowel surgery was less frequent (30.4% vs 37.2%, p< 0.001). In adjusted analysis (n=20,011), CUD was independently linked to lower odds of surgery (aOR=0.76, 95% CI: 0.66–0.89, p=0.0006). Alcohol use also predicted lower odds (aOR=0.78, p=0.040). Age, sex, and depression were not significant; private insurance was linked to higher odds. Charlson Comorbidity Index was similar (p=0.35).
Discussion: CUD was associated with lower bowel surgery rates and shorter LOS in hospitalized CD patients, without increased mortality or cost. These findings suggest cannabis use may influence hospitalization patterns but is not tied to worse outcomes. Although cannabis lacks anti-inflammatory effects, behavioral or care-related factors may explain these trends. Higher psychiatric comorbidity among CUD users highlights the need for integrated behavioral care. Understanding these associations may support risk stratification and multidisciplinary care in IBD.
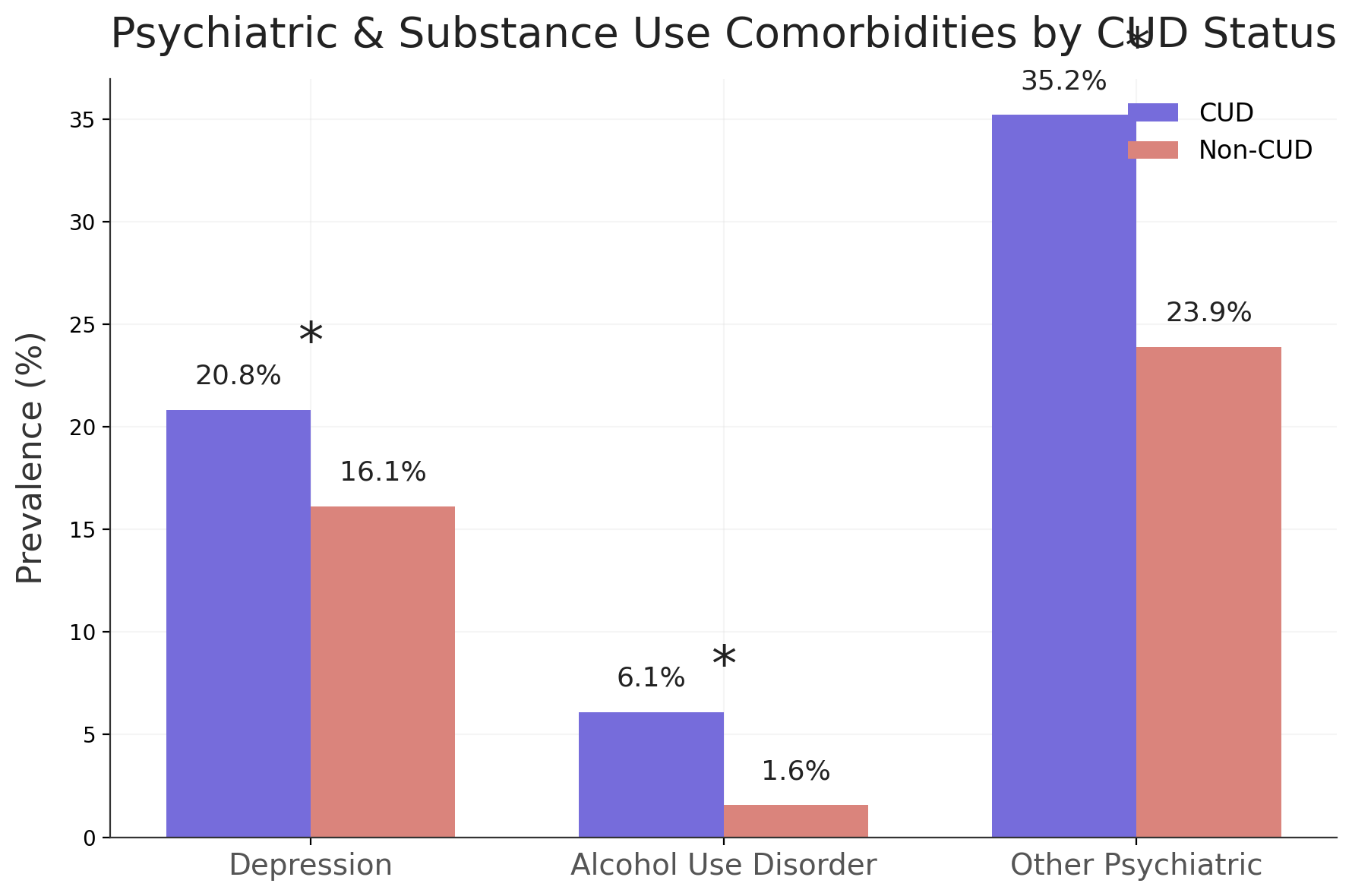
Figure: Figure 1. Comparison of inpatient outcomes—length of stay, hospital charges, and bowel surgery—among Crohn’s disease hospitalizations with vs without Cannabis Use Disorder.
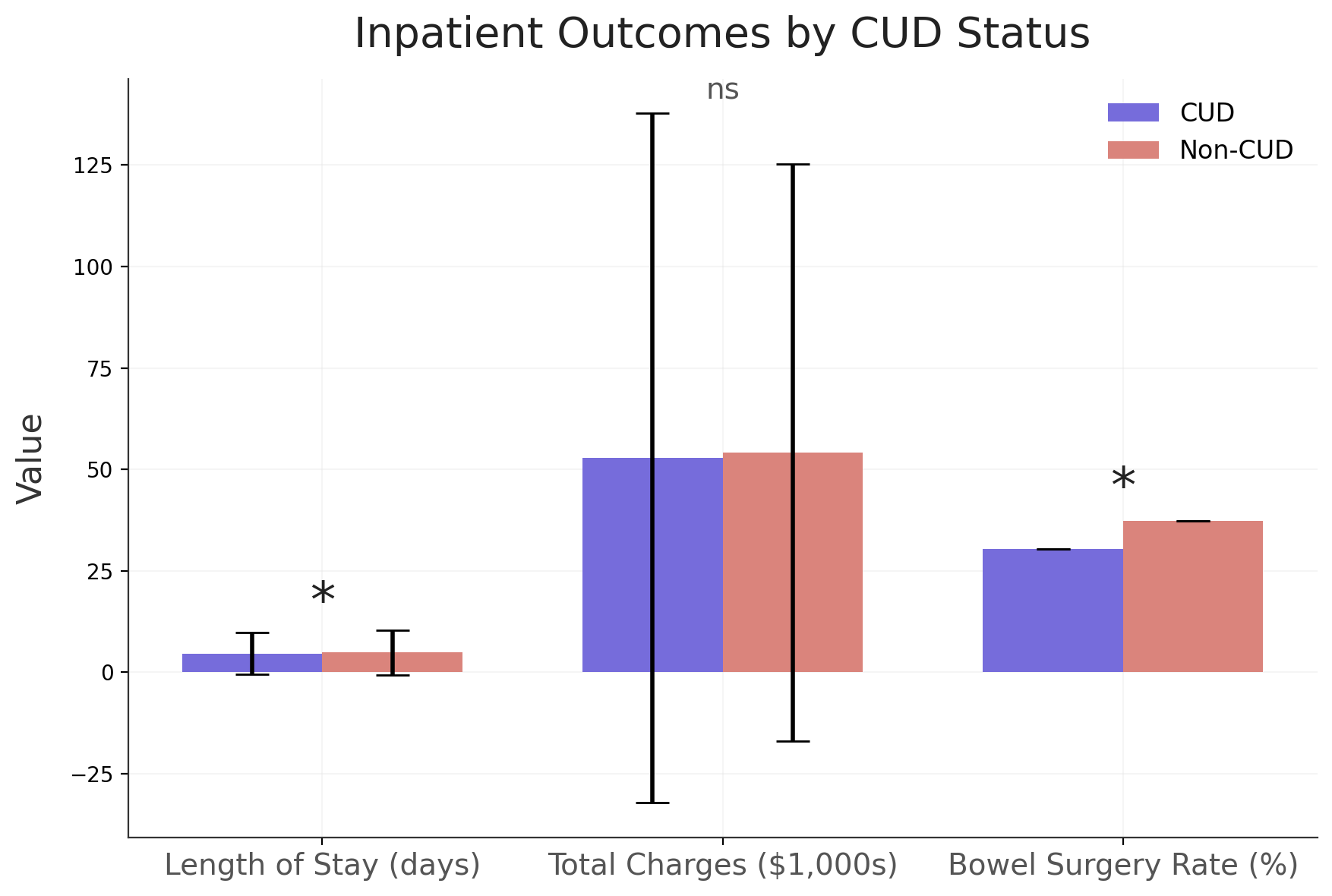
Figure: Figure 2. Prevalence of psychiatric and substance use comorbidities among Crohn’s disease hospitalizations, stratified by Cannabis Use Disorder status.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Shubham Gupta indicated no relevant financial relationships.
Shaunak Ganju indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Mesay Asfaw indicated no relevant financial relationships.
Farshad Aduli indicated no relevant financial relationships.
Nakul Ganju, MD1, Shubham Gupta, MD2, Shaunak Ganju, BS3, Juan C. Santiago-Gonzalez, MD, MSc4, Mesay Asfaw, MD5, Farshad Aduli, MD4. P5317 - Cannabis Use Disorder and Inpatient Outcomes in Crohn’s Disease Flares: A National Retrospective Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
