Tuesday Poster Session
Category: IBD
P5303 - Risk Factors and Outcomes of Urolithiasis Amongst Veterans With Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- JK
Jin Sun Kim, MD
University of California, Riverside
Riverside, CA
Presenting Author(s)
Jin Sun Kim, MD1, Edward Lee, DO1, Muhammad Shabbir, MD1, Peerapol Wangrattanapranee, MD1, Ammar Qureshi, MD1, Ashujot Dang, MD2, George Saffouri, MD1, Muhammad B. Hammami, MD1
1University of California, Riverside, Riverside, CA; 2University of California Riverside School of Medicine, Redlands, CA
Introduction: Inflammatory Bowel Disease (IBD), particularly Crohn’s Disease (CD), has been associated with an increased risk of urolithiasis in some studies. However, other risk factors for urinary tract stone formation in IBD patients remain unknown. This study aims to evaluate the characteristics and outcomes of IBD patients with urolithiasis and identify potential risk factors for urolithiasis in IBD.
Methods: We conducted a retrospective study of IBD patients followed at the Jerry L. Pettis Memorial Veterans' IBD clinic from January to June 2024. Patient charts were reviewed dating back to 1999. Data collected included patient demographics, IBD type, Charles Comorbidity Index (CCI), abdominal surgery, IBD medications, development of urolithiasis, and outcomes. Major abdominal surgery included small bowel or colon resection or ileal pouch anal anastomosis. Minor surgery included stricturoplasty, incision and drainage, or seton placement. Other surgery included cholecystectomy and appendectomy. Descriptive analysis was used.
Results: Among 328 patients with IBD (8.8% female), 186 (56.7%) had Ulcerative Colitis (UC), 120 (36.6%) had CD, and 22 (6.7%) had Indeterminate Colitis. 41 patients (12.5%) developed urolithiasis, with 33 (80.5%) experiencing nephrolithiasis. Patients with urolithiasis were older (67.1 ± 14.7 years vs. 61.1 ± 16.3 years; P = 0.031), had higher CCI (4.6 ± 3.0 vs. 3.0 ± 2.7; P < 0.001), and were more likely to have had major abdominal surgery (46.3% vs. 16.4%; P < 0.001). 46.3% of these patients had CD, whereas 35.2% of patients without urolithiasis had CD (P = 0.017) (Table 1).
Among the 41 patients with urolithiasis, 23 (56.1%) were symptomatic, and 12 (29.3%) required urologic intervention. 4 patients underwent shock wave lithotripsy, 7 underwent ureteroscopy, 6 underwent laser lithotripsy, and 1 underwent percutaneous nephrolithotomy. No patients required laparoscopic or open surgery (Table 1). One UC patient, on adalimumab, developed a post-procedural urinary tract infection within 90 days. Another CD patient discontinued vedolizumab prior to undergoing ureteroscopy and laser lithotripsy to minimize the risk of infection.
Discussion: IBD patients, particularly those with CD, older age, higher comorbidity, and history of major abdominal surgery, face a higher risk of urolithiasis. Overall, urolithiasis management in IBD appears safe, with minimal complications.
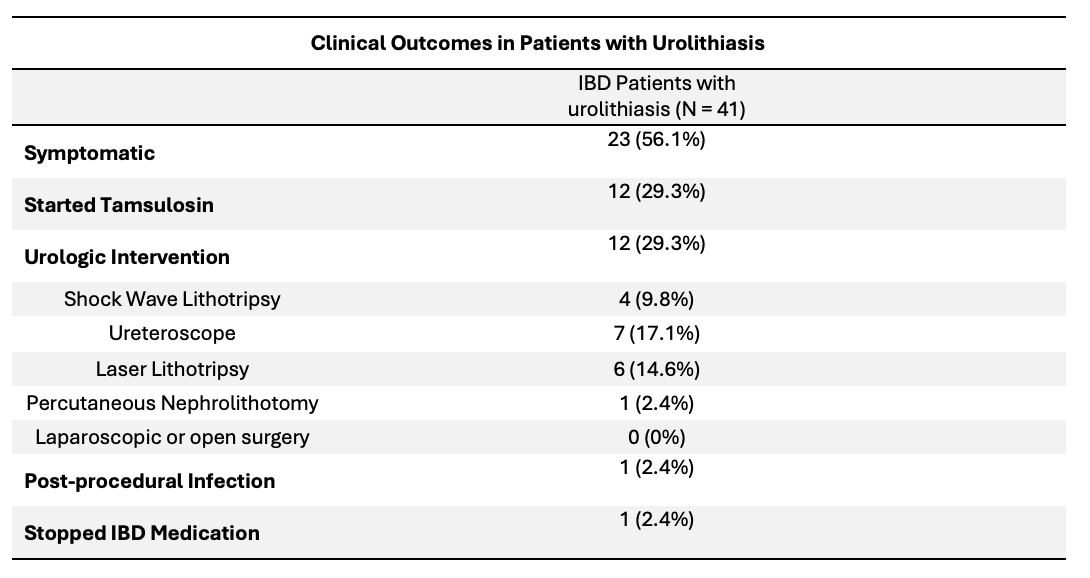
Figure: Table 1. Demographics and Clinical Characteristics of IBD Patients with and without Urolithiasis
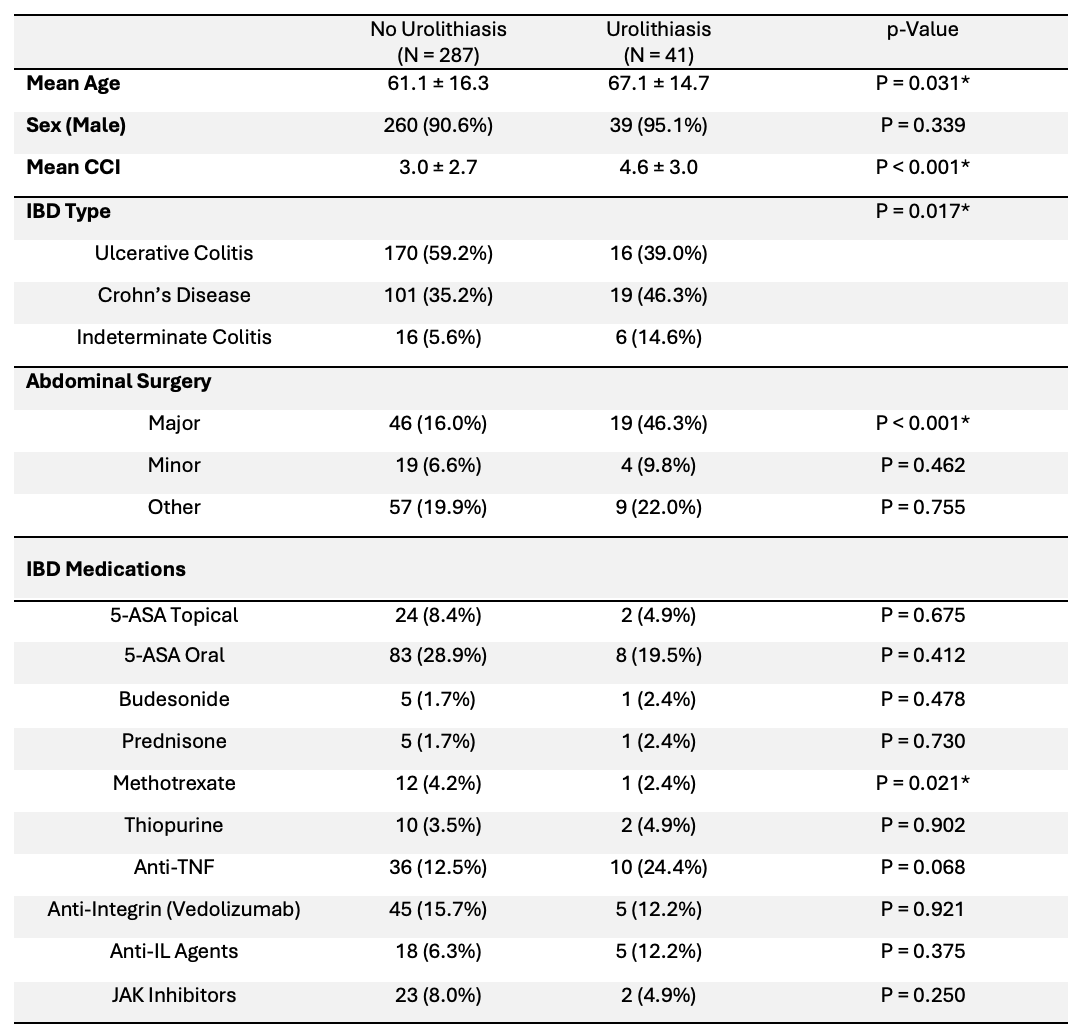
Figure: Table 2. Outcomes of IBD Patients with Urolithiasis
Disclosures:
Jin Sun Kim indicated no relevant financial relationships.
Edward Lee indicated no relevant financial relationships.
Muhammad Shabbir indicated no relevant financial relationships.
Peerapol Wangrattanapranee indicated no relevant financial relationships.
Ammar Qureshi indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
George Saffouri indicated no relevant financial relationships.
Muhammad B. Hammami indicated no relevant financial relationships.
Jin Sun Kim, MD1, Edward Lee, DO1, Muhammad Shabbir, MD1, Peerapol Wangrattanapranee, MD1, Ammar Qureshi, MD1, Ashujot Dang, MD2, George Saffouri, MD1, Muhammad B. Hammami, MD1. P5303 - Risk Factors and Outcomes of Urolithiasis Amongst Veterans With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California, Riverside, Riverside, CA; 2University of California Riverside School of Medicine, Redlands, CA
Introduction: Inflammatory Bowel Disease (IBD), particularly Crohn’s Disease (CD), has been associated with an increased risk of urolithiasis in some studies. However, other risk factors for urinary tract stone formation in IBD patients remain unknown. This study aims to evaluate the characteristics and outcomes of IBD patients with urolithiasis and identify potential risk factors for urolithiasis in IBD.
Methods: We conducted a retrospective study of IBD patients followed at the Jerry L. Pettis Memorial Veterans' IBD clinic from January to June 2024. Patient charts were reviewed dating back to 1999. Data collected included patient demographics, IBD type, Charles Comorbidity Index (CCI), abdominal surgery, IBD medications, development of urolithiasis, and outcomes. Major abdominal surgery included small bowel or colon resection or ileal pouch anal anastomosis. Minor surgery included stricturoplasty, incision and drainage, or seton placement. Other surgery included cholecystectomy and appendectomy. Descriptive analysis was used.
Results: Among 328 patients with IBD (8.8% female), 186 (56.7%) had Ulcerative Colitis (UC), 120 (36.6%) had CD, and 22 (6.7%) had Indeterminate Colitis. 41 patients (12.5%) developed urolithiasis, with 33 (80.5%) experiencing nephrolithiasis. Patients with urolithiasis were older (67.1 ± 14.7 years vs. 61.1 ± 16.3 years; P = 0.031), had higher CCI (4.6 ± 3.0 vs. 3.0 ± 2.7; P < 0.001), and were more likely to have had major abdominal surgery (46.3% vs. 16.4%; P < 0.001). 46.3% of these patients had CD, whereas 35.2% of patients without urolithiasis had CD (P = 0.017) (Table 1).
Among the 41 patients with urolithiasis, 23 (56.1%) were symptomatic, and 12 (29.3%) required urologic intervention. 4 patients underwent shock wave lithotripsy, 7 underwent ureteroscopy, 6 underwent laser lithotripsy, and 1 underwent percutaneous nephrolithotomy. No patients required laparoscopic or open surgery (Table 1). One UC patient, on adalimumab, developed a post-procedural urinary tract infection within 90 days. Another CD patient discontinued vedolizumab prior to undergoing ureteroscopy and laser lithotripsy to minimize the risk of infection.
Discussion: IBD patients, particularly those with CD, older age, higher comorbidity, and history of major abdominal surgery, face a higher risk of urolithiasis. Overall, urolithiasis management in IBD appears safe, with minimal complications.
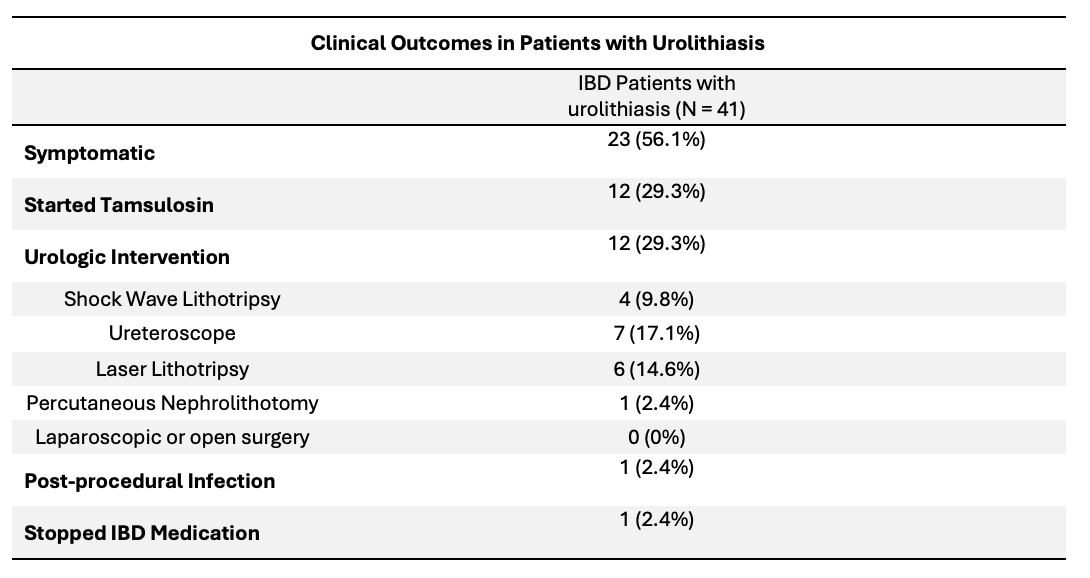
Figure: Table 1. Demographics and Clinical Characteristics of IBD Patients with and without Urolithiasis
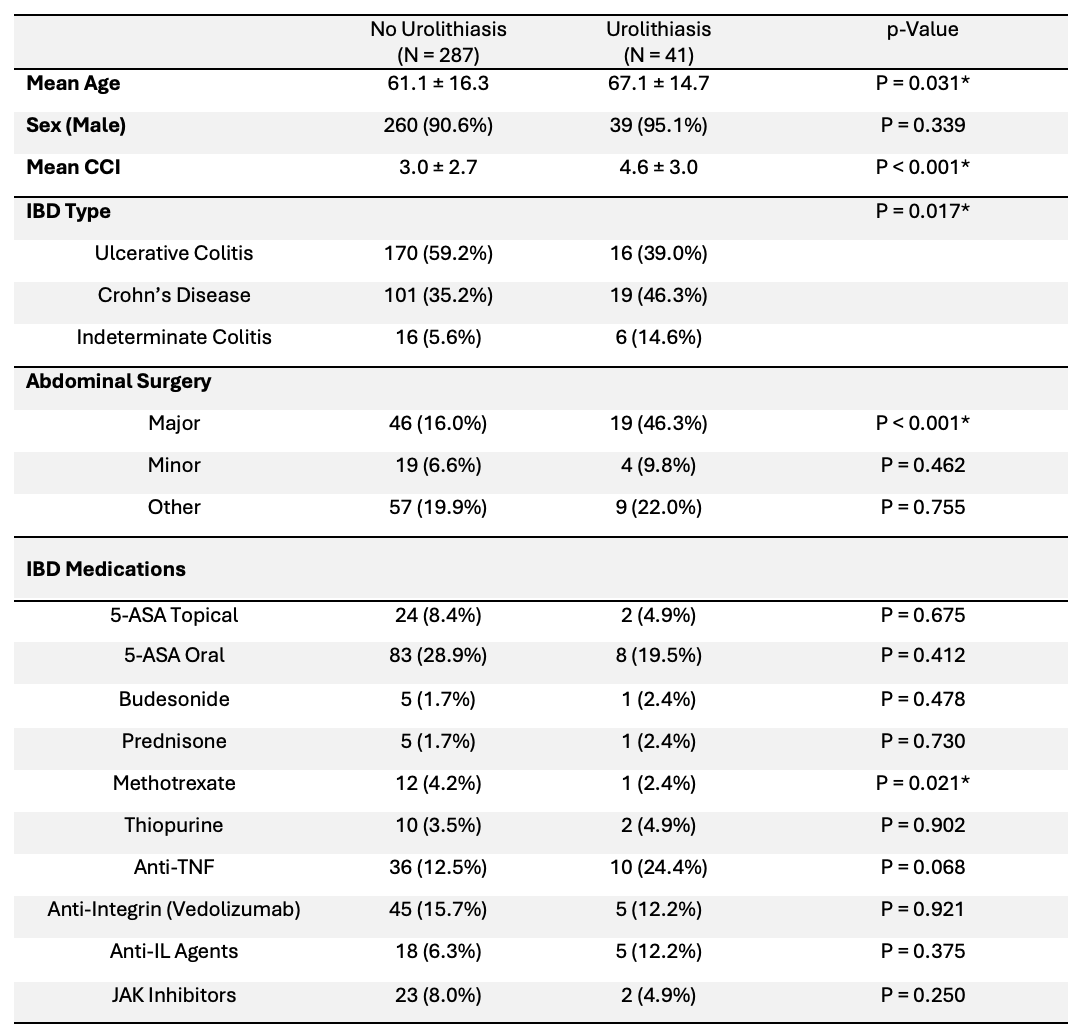
Figure: Table 2. Outcomes of IBD Patients with Urolithiasis
Disclosures:
Jin Sun Kim indicated no relevant financial relationships.
Edward Lee indicated no relevant financial relationships.
Muhammad Shabbir indicated no relevant financial relationships.
Peerapol Wangrattanapranee indicated no relevant financial relationships.
Ammar Qureshi indicated no relevant financial relationships.
Ashujot Dang indicated no relevant financial relationships.
George Saffouri indicated no relevant financial relationships.
Muhammad B. Hammami indicated no relevant financial relationships.
Jin Sun Kim, MD1, Edward Lee, DO1, Muhammad Shabbir, MD1, Peerapol Wangrattanapranee, MD1, Ammar Qureshi, MD1, Ashujot Dang, MD2, George Saffouri, MD1, Muhammad B. Hammami, MD1. P5303 - Risk Factors and Outcomes of Urolithiasis Amongst Veterans With Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
