Tuesday Poster Session
Category: IBD
P5302 - Demographic Predictors of Bowel Perforation in Ulcerative Colitis Patients: A National Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Vraj P. Shah, MD
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Vraj P. Shah, MD, Amanda A. Rupert, MD, Ahmed Al-Khazraji, MD
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Patients with inflammatory bowel disease, especially ulcerative colitis (UC), are at increased risk for developing bowel perforation. Bowel perforation is associated with significantly increased morbidity and mortality. However, there is a paucity of data regarding risk factors for developing bowel perforations in those admitted with UC. Thus, our study seeks to provide a nationwide inpatient analysis of demographic predictors and disparities associated with risks for developing bowel perforation in patients with UC.
Methods: We performed a retrospective population-based cohort study using the 2016-2020 National Inpatient Sample (NIS). Using ICD-10 diagnosis codes, the NIS was queried for adult inpatients with a diagnosis of UC without a concurrent diagnosis of Crohn’s disease. Bivariate analyses were performed to compare the demographics of patients with and without bowel perforation. A multivariable logistic regression was then performed to identify predictors of bowel perforation.
Results: A total of 624,930 patients with UC met inclusion criteria, with 4,985 (0.8%) experiencing a bowel perforation. On bivariate analysis, female patients had lower rates of perforation (0.7% vs 0.9%, p< 0.001). There were significant differences in race (p< 0.001), income (p< 0.001), and insurance (p< 0.001) in those experiencing perforations. On multivariable analysis controlling for demographic factors, female (OR=0.612, p< 0.001) and Black (OR=0.592, p< 0.001) patients were at decreased risk for developing perforation. Patients with private insurance were at greater risk than those with Medicare (OR=1.511, p< 0.001). Clostridium difficile infection (OR=1.828, p< 0.001) and chronic steroid use (OR=1.534, p< 0.001) were associated with increased risk of developing perforations.
Discussion: Demographic disparities, including sex and race, are evident among UC patients who develop bowel perforations. Black patients and female patients are at lower risk for developing perforations compared to their White and male counterparts, respectively. As established in previous studies, Clostridium difficile infection and chronic steroid use are associated with increased risk for perforation. These findings highlight the presence of racial and gender disparities in healthcare, including the complications of UC. Given that bowel perforation portends poorer outcomes in UC, further research is needed to explore the underlying cause of these disparities and to develop targeted interventions to reduce them.
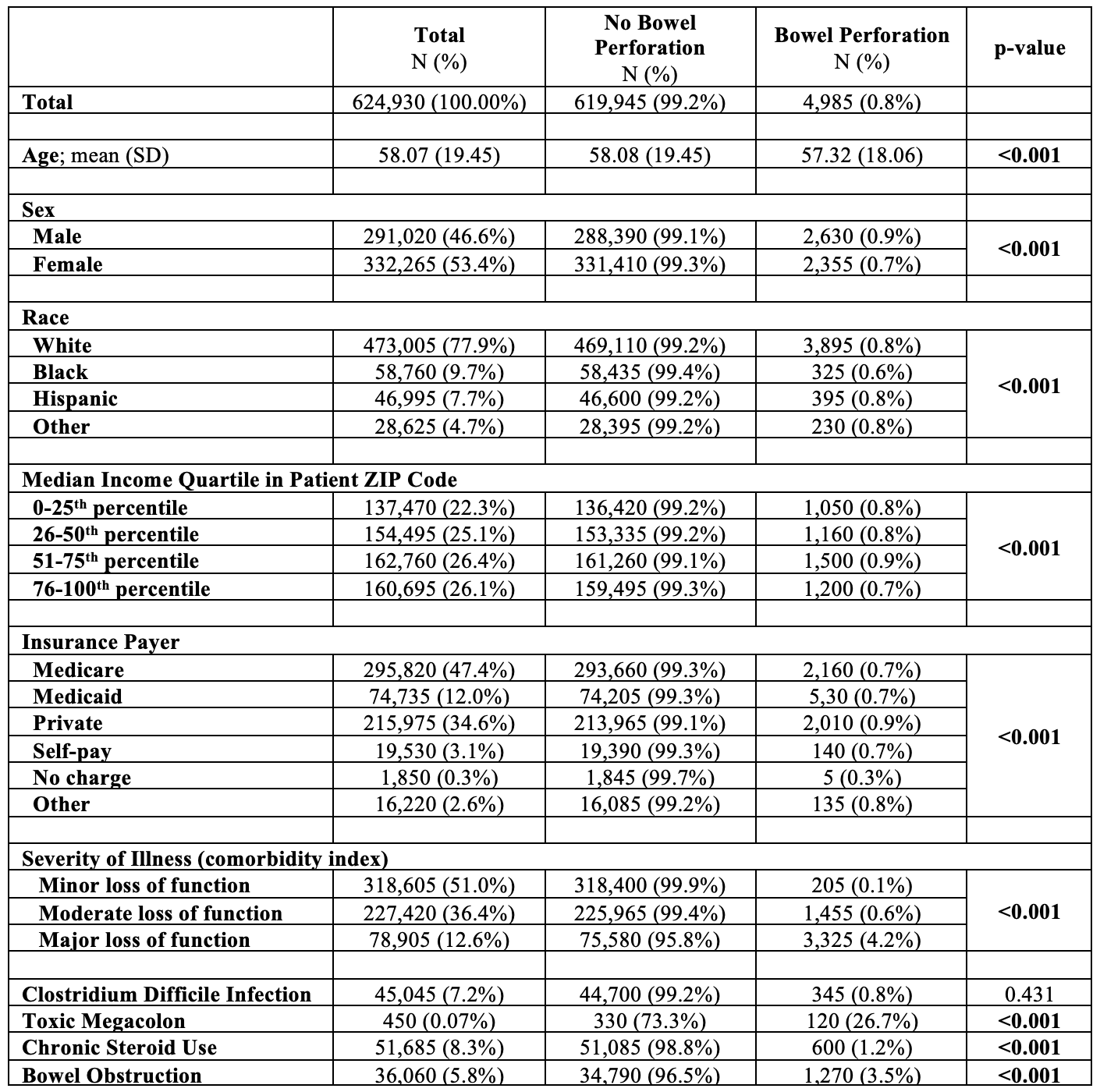
Figure: Table 1: Bivariate Analysis of Ulcerative Colitis Patients with and without Bowel Perforation
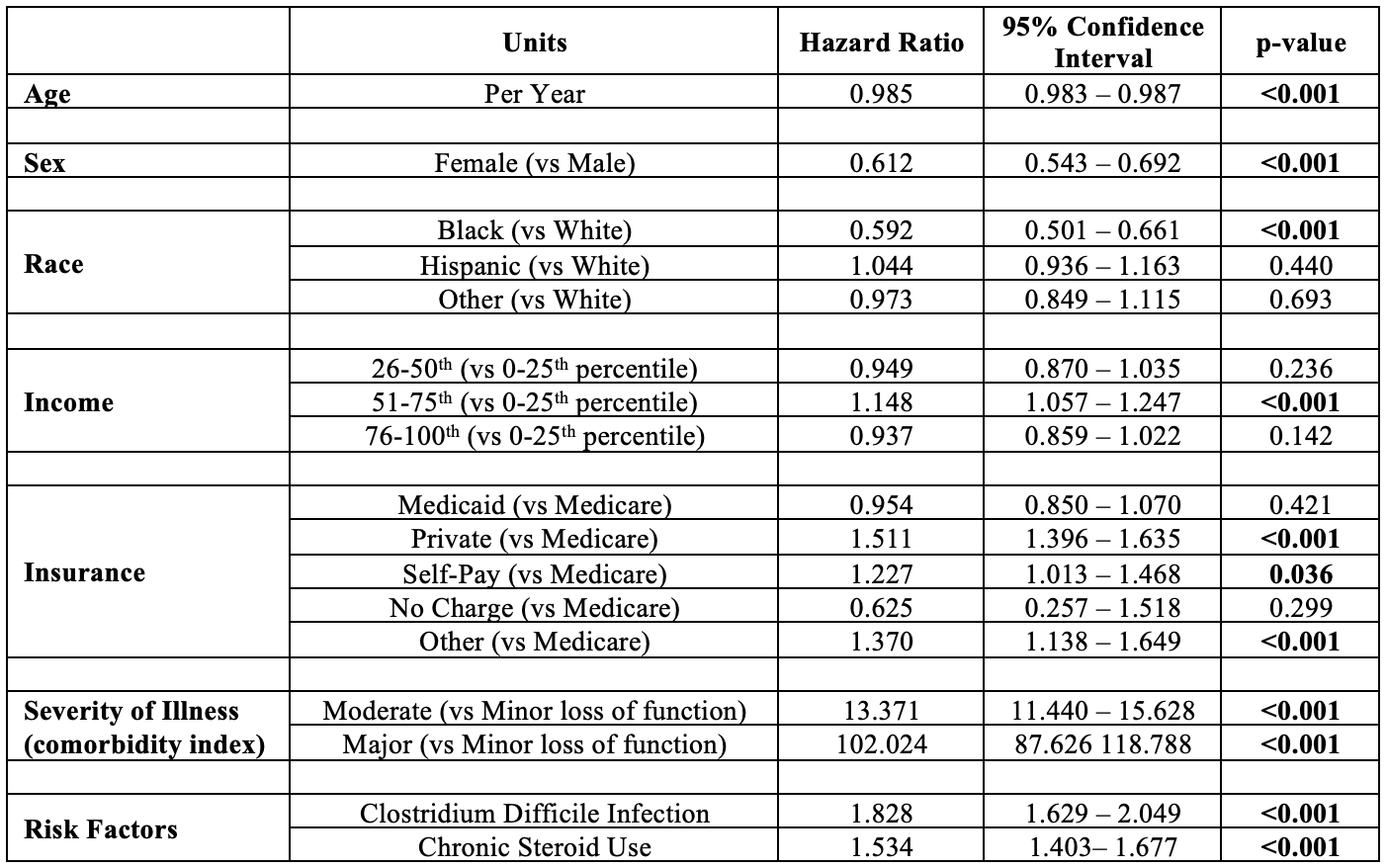
Figure: Table 2: Predictors of Bowel Perforation in Patients with Ulcerative Colitis (multivariable logistic regression)
Disclosures:
Vraj Shah indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Vraj P. Shah, MD, Amanda A. Rupert, MD, Ahmed Al-Khazraji, MD. P5302 - Demographic Predictors of Bowel Perforation in Ulcerative Colitis Patients: A National Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Rutgers New Jersey Medical School, Newark, NJ
Introduction: Patients with inflammatory bowel disease, especially ulcerative colitis (UC), are at increased risk for developing bowel perforation. Bowel perforation is associated with significantly increased morbidity and mortality. However, there is a paucity of data regarding risk factors for developing bowel perforations in those admitted with UC. Thus, our study seeks to provide a nationwide inpatient analysis of demographic predictors and disparities associated with risks for developing bowel perforation in patients with UC.
Methods: We performed a retrospective population-based cohort study using the 2016-2020 National Inpatient Sample (NIS). Using ICD-10 diagnosis codes, the NIS was queried for adult inpatients with a diagnosis of UC without a concurrent diagnosis of Crohn’s disease. Bivariate analyses were performed to compare the demographics of patients with and without bowel perforation. A multivariable logistic regression was then performed to identify predictors of bowel perforation.
Results: A total of 624,930 patients with UC met inclusion criteria, with 4,985 (0.8%) experiencing a bowel perforation. On bivariate analysis, female patients had lower rates of perforation (0.7% vs 0.9%, p< 0.001). There were significant differences in race (p< 0.001), income (p< 0.001), and insurance (p< 0.001) in those experiencing perforations. On multivariable analysis controlling for demographic factors, female (OR=0.612, p< 0.001) and Black (OR=0.592, p< 0.001) patients were at decreased risk for developing perforation. Patients with private insurance were at greater risk than those with Medicare (OR=1.511, p< 0.001). Clostridium difficile infection (OR=1.828, p< 0.001) and chronic steroid use (OR=1.534, p< 0.001) were associated with increased risk of developing perforations.
Discussion: Demographic disparities, including sex and race, are evident among UC patients who develop bowel perforations. Black patients and female patients are at lower risk for developing perforations compared to their White and male counterparts, respectively. As established in previous studies, Clostridium difficile infection and chronic steroid use are associated with increased risk for perforation. These findings highlight the presence of racial and gender disparities in healthcare, including the complications of UC. Given that bowel perforation portends poorer outcomes in UC, further research is needed to explore the underlying cause of these disparities and to develop targeted interventions to reduce them.
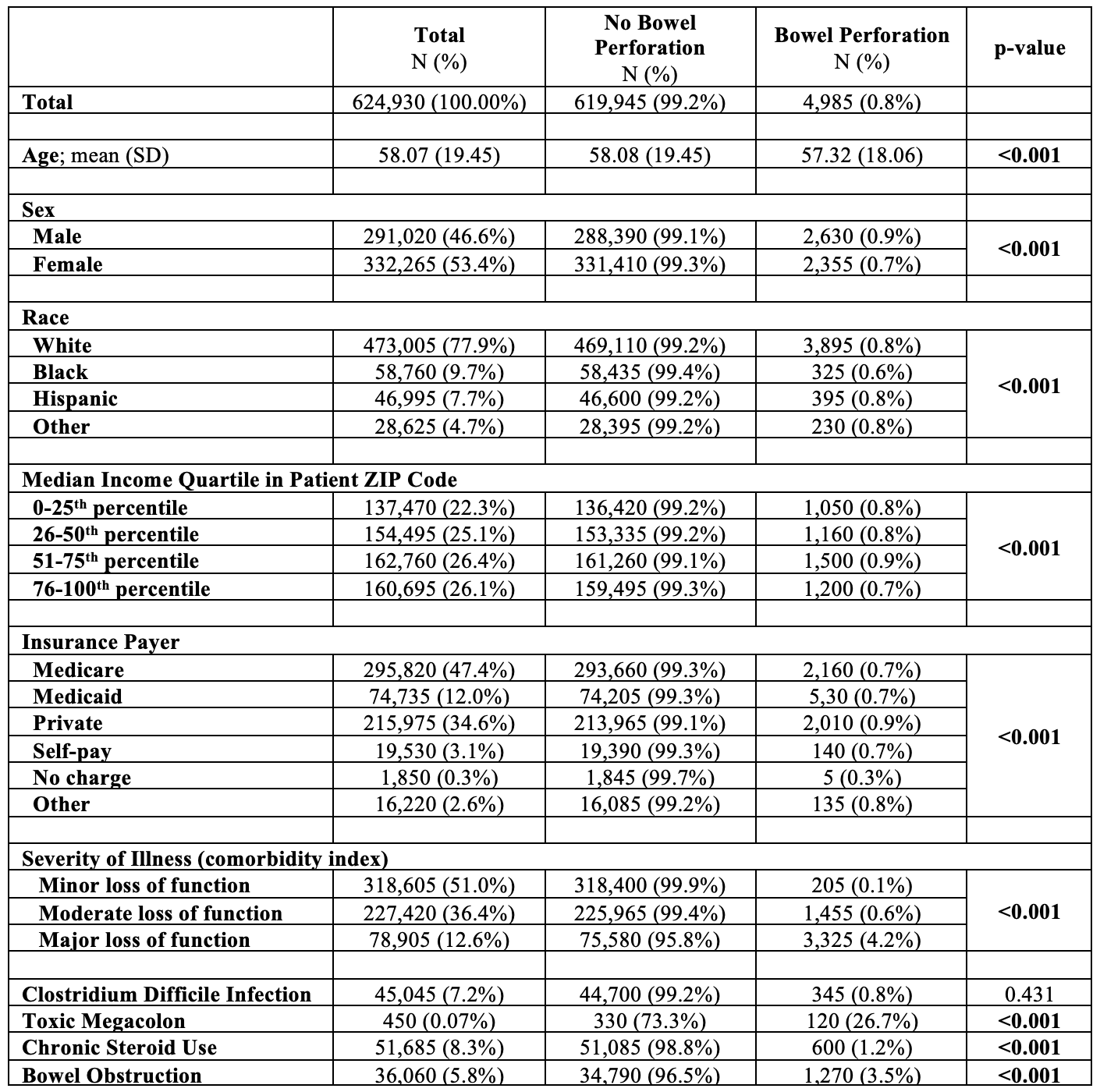
Figure: Table 1: Bivariate Analysis of Ulcerative Colitis Patients with and without Bowel Perforation
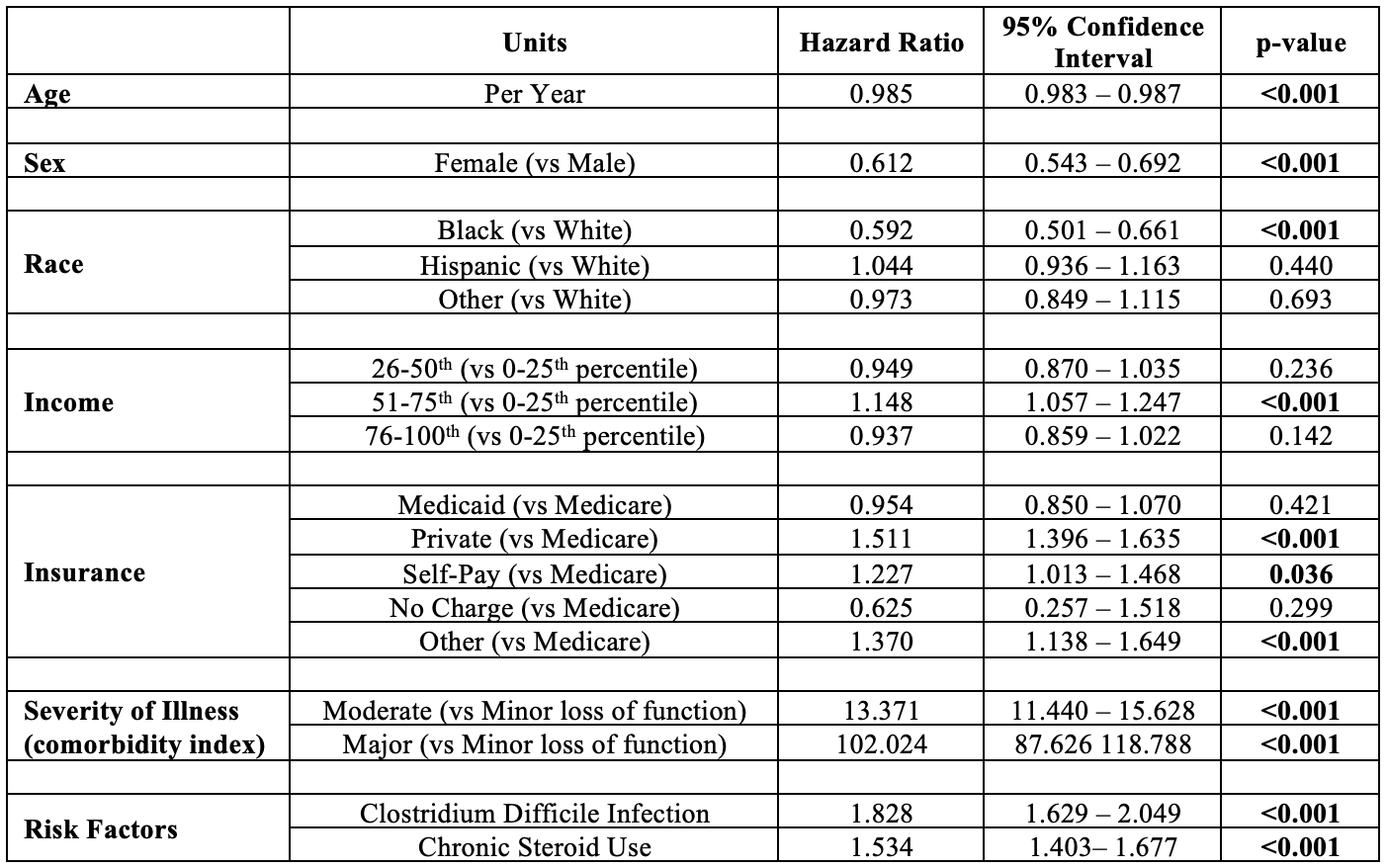
Figure: Table 2: Predictors of Bowel Perforation in Patients with Ulcerative Colitis (multivariable logistic regression)
Disclosures:
Vraj Shah indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Vraj P. Shah, MD, Amanda A. Rupert, MD, Ahmed Al-Khazraji, MD. P5302 - Demographic Predictors of Bowel Perforation in Ulcerative Colitis Patients: A National Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
