Tuesday Poster Session
Category: GI Bleeding
P5295 - Bleeding and Thrombosis: Navigating Competing Risks in the Management of Downhill Esophageal Varices
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Amen I. Javaid, MD (she/her/hers)
INOVA Fairfax Hospital
Woodbridge, VA
Presenting Author(s)
Amen I. Javaid, MD
INOVA Fairfax Hospital, Woodbridge, VA
Introduction: Downhill esophageal varices are an uncommon but important cause of upper GI bleeding. Unlike the more familiar varices caused by portal HTN, these develop from superior vena cava (SVC) obstruction, often related to prior central venous access. Management can be particularly challenging when bleeding occurs, as endoscopic therapy alone is rarely definitive. This case illustrates the clinical decision making involved in treating downhill varices in a medically complex patient with elevated risk for both bleeding and thrombosis.
Case Description/
Methods: A 54 year old man with ESRD on dialysis, HIV on antiretroviral therapy, nonischemic, cardiac amyloidosis, and prostate cancer treated with pelvic radiation presented with hematemesis and hematochezia. His history also included radiation proctitis and a known chronic SVC occlusion from prior long term central venous catheters.
On arrival, he was tachycardic and profoundly anemic with a hemoglobin of 6 g/d. CT angiography revealed extensive collateral vessels including thoracoabdominal varices and high grade SVC stenosis. Physical exam was significant for venous engorgement of the chest wall. EGD showed large esophageal varices without signs of portal hypertension. Colonoscopy showed large sessile polyp with radiation proctitis. Abdominal ultrasound was pursued which confirmed the absence of cirrhosis.
Given his bleeding risk from radiation proctitis, the gastroenterology and interventional radiology teams initially considered performing endoscopic banding to stabilize him before intervening on the SVC. However, after further literature review and collaborative discussion, the teams elected to proceed directly with venous intervention. Venography confirmed severe stenosis of the SVC and right innominate vein, along with occlusion of the right internal jugular vein. The patient underwent successful percutaneous transluminal angioplasty with placement of a 12 x 60 mm stent. He was started on apixaban to maintain stent patency after GI deemed the bleeding risk acceptable. At one month follow up, CTA demonstrated continued stent patency and the patient reported no further bleeding episodes.
Discussion: This case underscores the importance of recognizing downhill varices as a distinct clinical entity requiring a different approach than portal hypertensive varices. While endoscopic therapy may offer temporary control, definitive management depends on relieving the underlying venous obstruction.
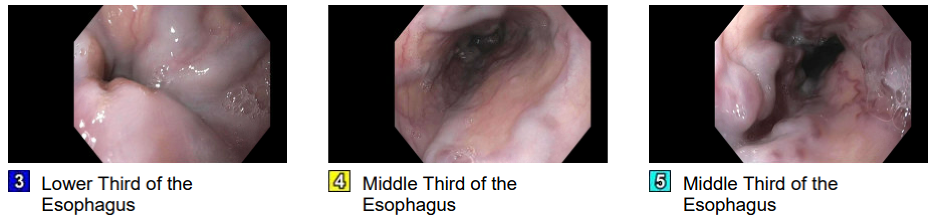
Figure: Large esophageal varices visualized on initial endoscopy
Disclosures:
Amen Javaid indicated no relevant financial relationships.
Amen I. Javaid, MD. P5295 - Bleeding and Thrombosis: Navigating Competing Risks in the Management of Downhill Esophageal Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
INOVA Fairfax Hospital, Woodbridge, VA
Introduction: Downhill esophageal varices are an uncommon but important cause of upper GI bleeding. Unlike the more familiar varices caused by portal HTN, these develop from superior vena cava (SVC) obstruction, often related to prior central venous access. Management can be particularly challenging when bleeding occurs, as endoscopic therapy alone is rarely definitive. This case illustrates the clinical decision making involved in treating downhill varices in a medically complex patient with elevated risk for both bleeding and thrombosis.
Case Description/
Methods: A 54 year old man with ESRD on dialysis, HIV on antiretroviral therapy, nonischemic, cardiac amyloidosis, and prostate cancer treated with pelvic radiation presented with hematemesis and hematochezia. His history also included radiation proctitis and a known chronic SVC occlusion from prior long term central venous catheters.
On arrival, he was tachycardic and profoundly anemic with a hemoglobin of 6 g/d. CT angiography revealed extensive collateral vessels including thoracoabdominal varices and high grade SVC stenosis. Physical exam was significant for venous engorgement of the chest wall. EGD showed large esophageal varices without signs of portal hypertension. Colonoscopy showed large sessile polyp with radiation proctitis. Abdominal ultrasound was pursued which confirmed the absence of cirrhosis.
Given his bleeding risk from radiation proctitis, the gastroenterology and interventional radiology teams initially considered performing endoscopic banding to stabilize him before intervening on the SVC. However, after further literature review and collaborative discussion, the teams elected to proceed directly with venous intervention. Venography confirmed severe stenosis of the SVC and right innominate vein, along with occlusion of the right internal jugular vein. The patient underwent successful percutaneous transluminal angioplasty with placement of a 12 x 60 mm stent. He was started on apixaban to maintain stent patency after GI deemed the bleeding risk acceptable. At one month follow up, CTA demonstrated continued stent patency and the patient reported no further bleeding episodes.
Discussion: This case underscores the importance of recognizing downhill varices as a distinct clinical entity requiring a different approach than portal hypertensive varices. While endoscopic therapy may offer temporary control, definitive management depends on relieving the underlying venous obstruction.
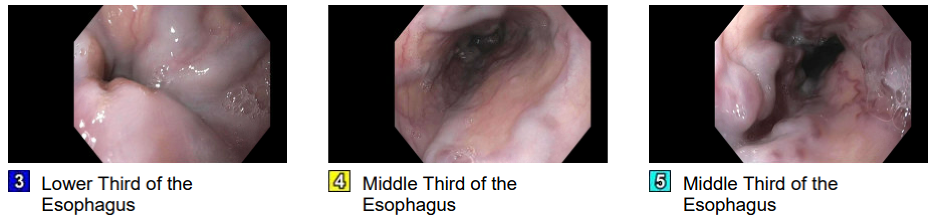
Figure: Large esophageal varices visualized on initial endoscopy
Disclosures:
Amen Javaid indicated no relevant financial relationships.
Amen I. Javaid, MD. P5295 - Bleeding and Thrombosis: Navigating Competing Risks in the Management of Downhill Esophageal Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
