Tuesday Poster Session
Category: GI Bleeding
P5282 - Gastric Involvement Is an Uncommon Presentation of Systemic Amyloidosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Sarah Yang, MD, BA (she/her/hers)
University of Maryland School of Medicine
Baltimore, MD
Presenting Author(s)
Sarah Yang, MD, BA, Cerise Kleb, MD, Elsadig Abdalla, MD, Kirti Shetty, MD
University of Maryland School of Medicine, Baltimore, MD
Introduction: Systemic amyloidosis is the extracellular deposition of fibrillar proteins that deposit into various tissues such as the heart, kidney, liver, or nerves, resulting in organ dysfunction. Amyloidosis of the gastrointestinal (GI) tract is uncommon, affecting only 4% of those with systemic amyloidosis.
Case Description/
Methods: Mr. S is a 41-year-old male with a past medical history of end stage renal disease on hemodialysis (previously deferring kidney biopsy), IV drug use, Hepatitis C post treatment, type 2 diabetes, presenting for altered mental status. He was noted to have decompensated cirrhosis with hepatic encephalopathy and spontaneous bacterial peritonitis. An esophagogastroduodenoscopy (EGD) was performed to evaluate for anemia. Findings revealed diffuse gastric mucosal congestion and erythema, attributed to portal hypertensive gastropathy. No biopsy was taken at the time. He was discharged and then readmitted one month later. A repeat EGD was done to evaluate for recurrent anemia showing friable and erythematous gastric mucosa in the antrum. Biopsy from the antrum revealed gastric glands with eosinophilic material diffusely present in the interstitial space (Figure A). Congo red staining confirmed amyloidosis (Figure B). A bone marrow biopsy revealed mild polytypic plasmacytosis and amyloid deposition with no evidence of plasma cells suggestive of secondary systemic (AA) amyloidosis. He was eventually discharged home with close follow-up.
Discussion: GI Amyloidosis proven by GI biopsy is relatively rare, found in only 3.3% of patients in a retrospective study. GI amyloidosis is associated with bleeding due to the mucosal lesions and vascular friability. Other symptoms include diarrhea, ascites, weight loss, and abnormal peristalsis. GI amyloidosis is a difficult diagnosis given the nonspecific clinical presentation, with patients undergoing unnecessary testing. Clinicians should suspect amyloidosis if history includes involvement of other organs (renal failure, proteinuria, neuropathy), inflammatory conditions like rheumatoid or inflammatory bowel disease, or a positive family history. Laboratory testing may reveal anemia, elevations in alkaline phosphatase, and increases in acute-phase reactants. Tissue biopsy is the diagnostic gold standard. Endoscopic view may reveal a granular appearance with erosions, wall thickening, or friability. Treatment focuses on controlling the underlying inflammatory disease to reduce the production of amyloid protein.
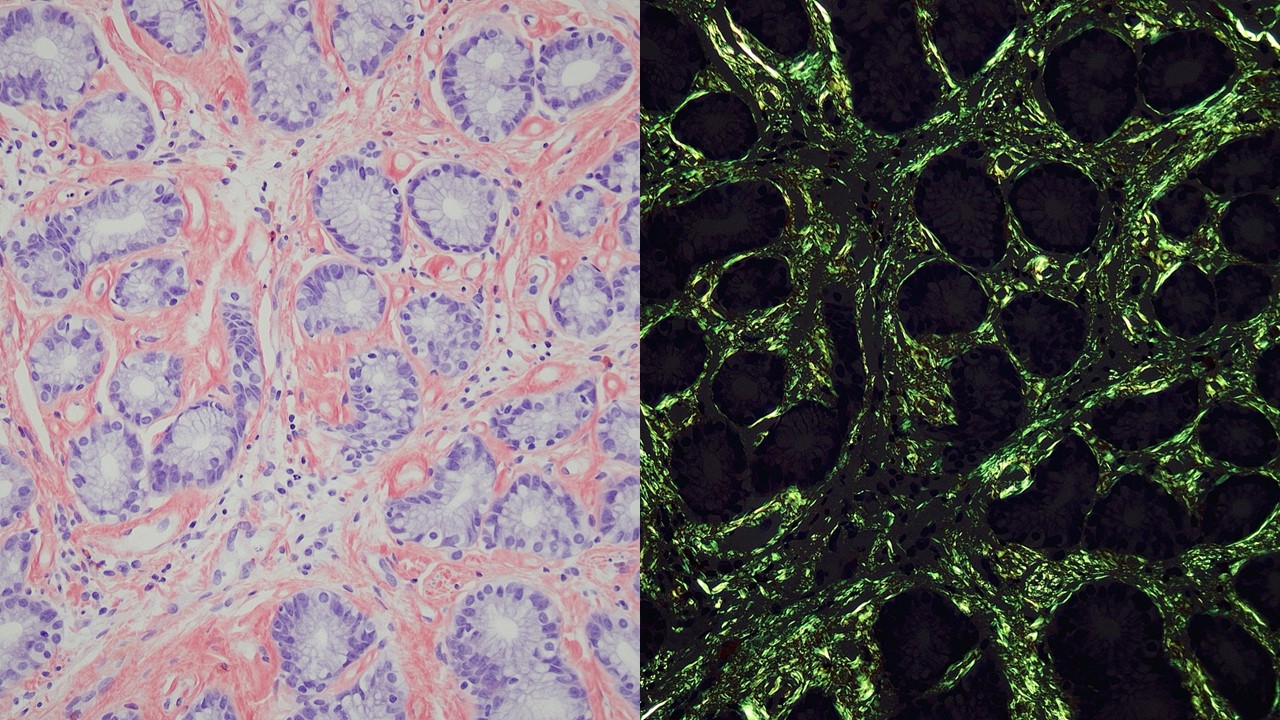
Figure: Figure A: Hematoxylin and eosin staining shows amorphous and homogenous pale-pink material diffusely involving the interstitial space. (20x magnification)
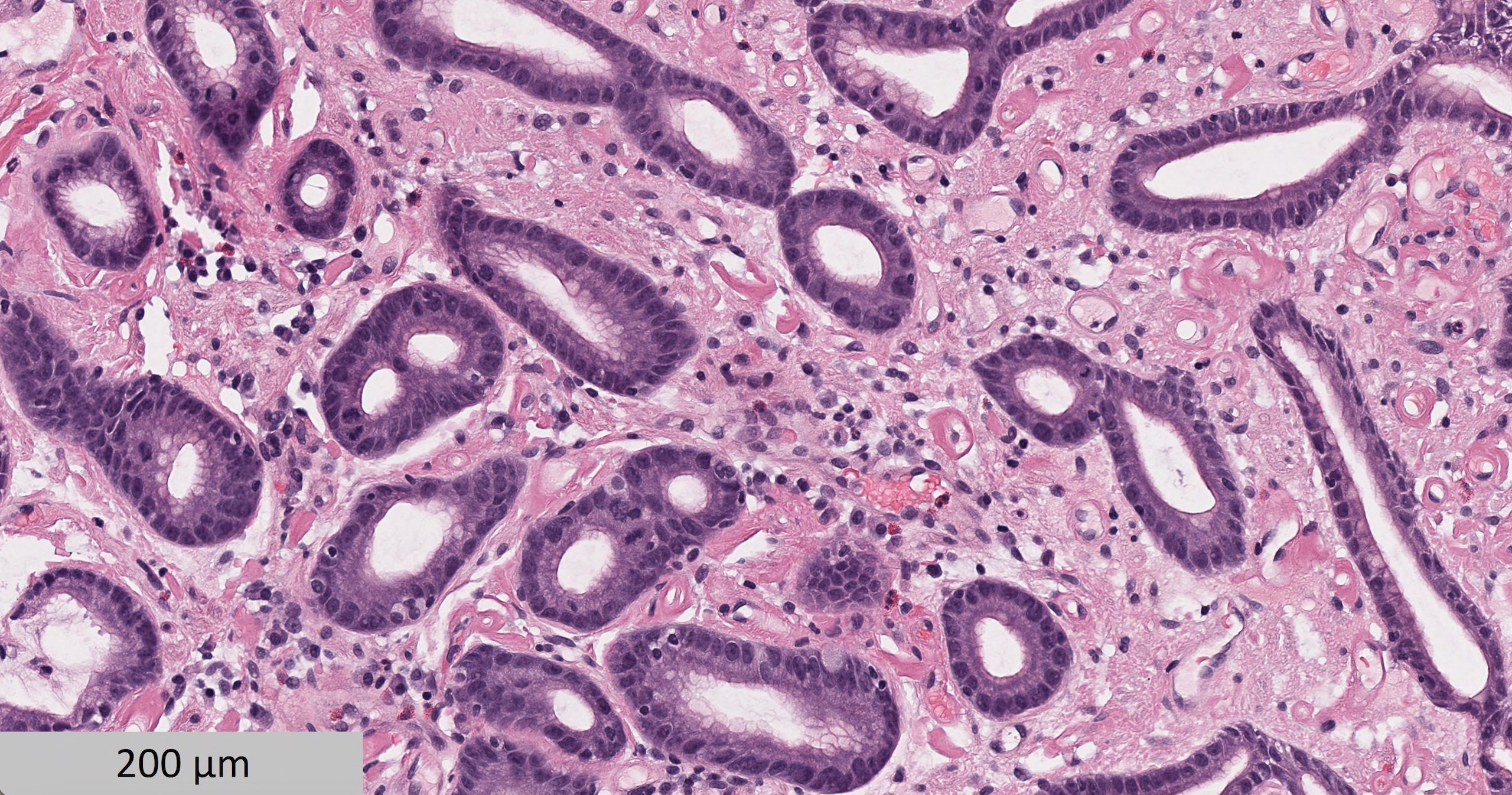
Figure: Figure B: Congo red staining highlights abundant salmon colored amorphous material in the interstitial space (left). Under polarized right the material demonstrates green birefringence (right). (20x magnification)
Disclosures:
Sarah Yang indicated no relevant financial relationships.
Cerise Kleb indicated no relevant financial relationships.
Elsadig Abdalla indicated no relevant financial relationships.
Kirti Shetty indicated no relevant financial relationships.
Sarah Yang, MD, BA, Cerise Kleb, MD, Elsadig Abdalla, MD, Kirti Shetty, MD. P5282 - Gastric Involvement Is an Uncommon Presentation of Systemic Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
University of Maryland School of Medicine, Baltimore, MD
Introduction: Systemic amyloidosis is the extracellular deposition of fibrillar proteins that deposit into various tissues such as the heart, kidney, liver, or nerves, resulting in organ dysfunction. Amyloidosis of the gastrointestinal (GI) tract is uncommon, affecting only 4% of those with systemic amyloidosis.
Case Description/
Methods: Mr. S is a 41-year-old male with a past medical history of end stage renal disease on hemodialysis (previously deferring kidney biopsy), IV drug use, Hepatitis C post treatment, type 2 diabetes, presenting for altered mental status. He was noted to have decompensated cirrhosis with hepatic encephalopathy and spontaneous bacterial peritonitis. An esophagogastroduodenoscopy (EGD) was performed to evaluate for anemia. Findings revealed diffuse gastric mucosal congestion and erythema, attributed to portal hypertensive gastropathy. No biopsy was taken at the time. He was discharged and then readmitted one month later. A repeat EGD was done to evaluate for recurrent anemia showing friable and erythematous gastric mucosa in the antrum. Biopsy from the antrum revealed gastric glands with eosinophilic material diffusely present in the interstitial space (Figure A). Congo red staining confirmed amyloidosis (Figure B). A bone marrow biopsy revealed mild polytypic plasmacytosis and amyloid deposition with no evidence of plasma cells suggestive of secondary systemic (AA) amyloidosis. He was eventually discharged home with close follow-up.
Discussion: GI Amyloidosis proven by GI biopsy is relatively rare, found in only 3.3% of patients in a retrospective study. GI amyloidosis is associated with bleeding due to the mucosal lesions and vascular friability. Other symptoms include diarrhea, ascites, weight loss, and abnormal peristalsis. GI amyloidosis is a difficult diagnosis given the nonspecific clinical presentation, with patients undergoing unnecessary testing. Clinicians should suspect amyloidosis if history includes involvement of other organs (renal failure, proteinuria, neuropathy), inflammatory conditions like rheumatoid or inflammatory bowel disease, or a positive family history. Laboratory testing may reveal anemia, elevations in alkaline phosphatase, and increases in acute-phase reactants. Tissue biopsy is the diagnostic gold standard. Endoscopic view may reveal a granular appearance with erosions, wall thickening, or friability. Treatment focuses on controlling the underlying inflammatory disease to reduce the production of amyloid protein.
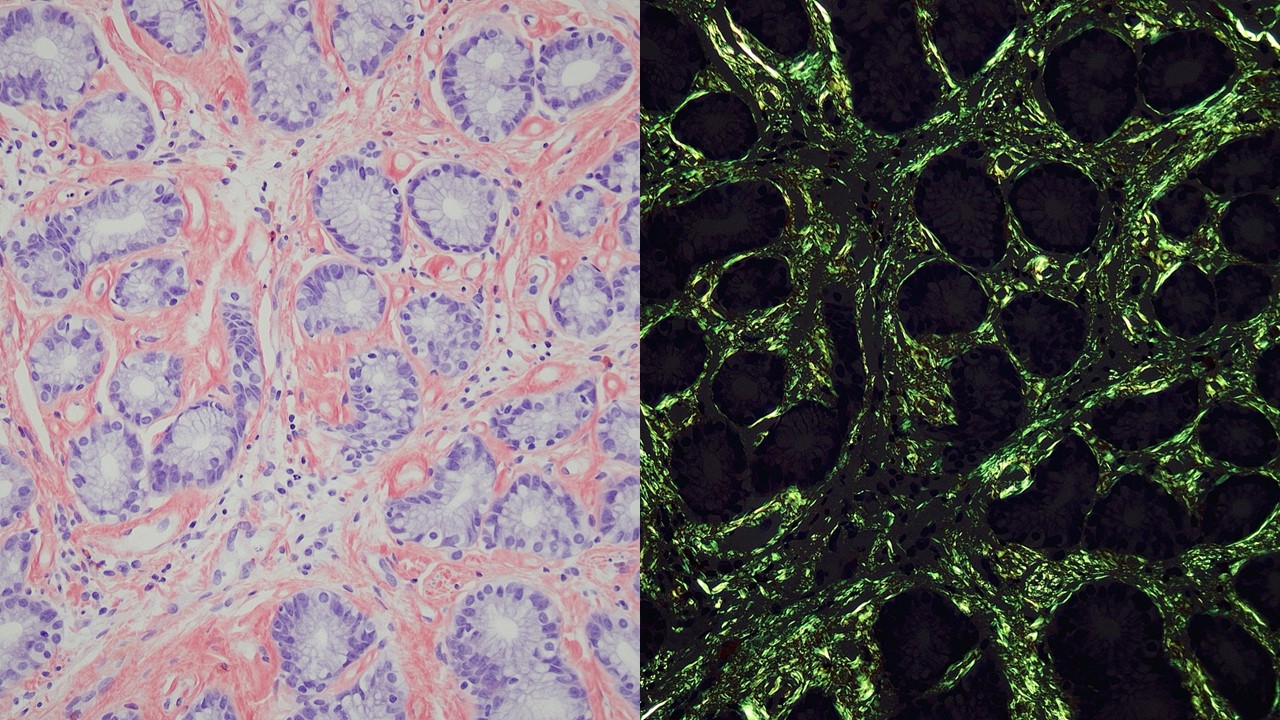
Figure: Figure A: Hematoxylin and eosin staining shows amorphous and homogenous pale-pink material diffusely involving the interstitial space. (20x magnification)
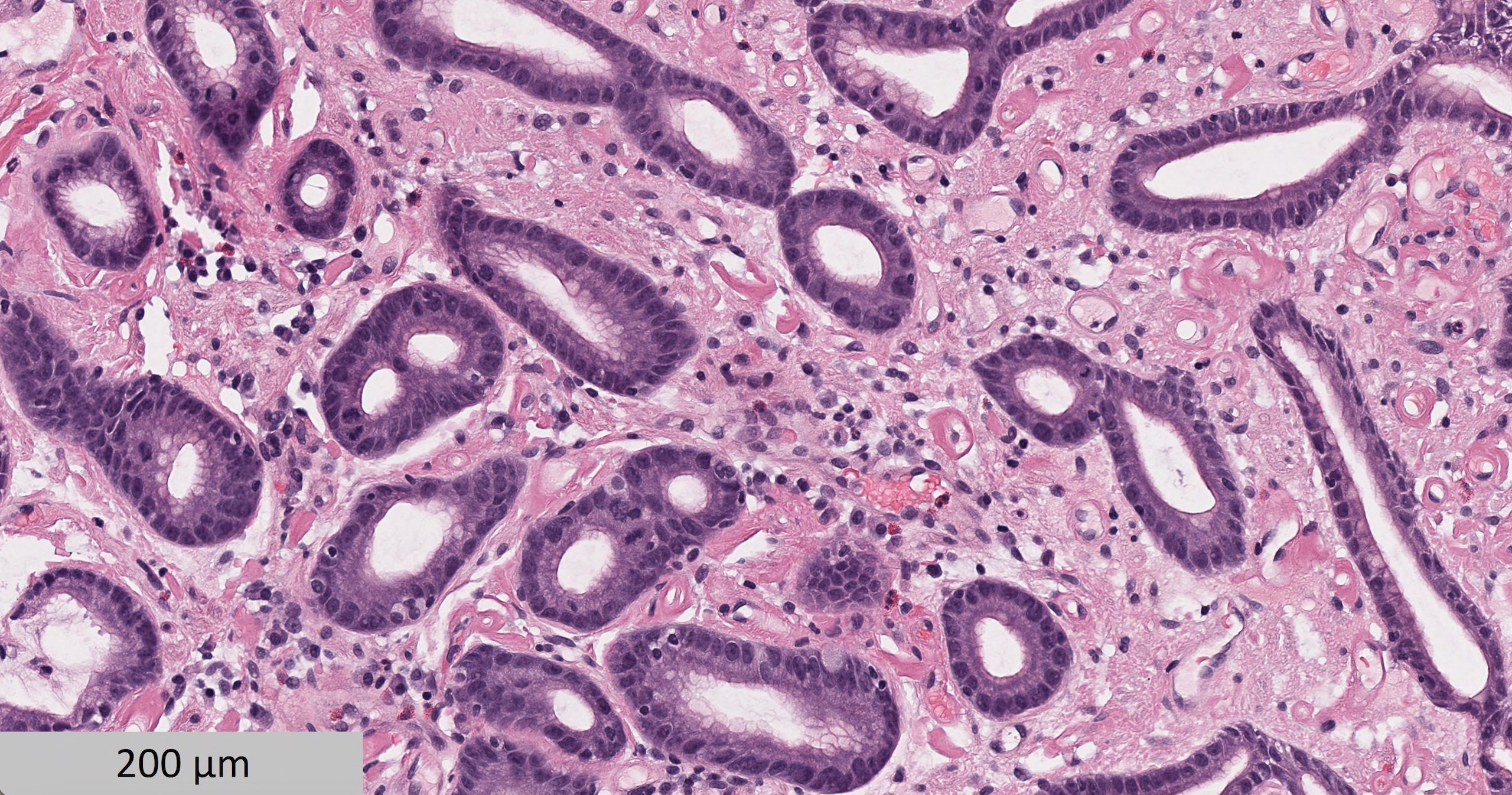
Figure: Figure B: Congo red staining highlights abundant salmon colored amorphous material in the interstitial space (left). Under polarized right the material demonstrates green birefringence (right). (20x magnification)
Disclosures:
Sarah Yang indicated no relevant financial relationships.
Cerise Kleb indicated no relevant financial relationships.
Elsadig Abdalla indicated no relevant financial relationships.
Kirti Shetty indicated no relevant financial relationships.
Sarah Yang, MD, BA, Cerise Kleb, MD, Elsadig Abdalla, MD, Kirti Shetty, MD. P5282 - Gastric Involvement Is an Uncommon Presentation of Systemic Amyloidosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
