Tuesday Poster Session
Category: GI Bleeding
P5278 - Aortoesophageal Fistula Secondary to Infected TEVAR Graft: A Fatal Complication Following UTI Bacteremia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Toru Nakata, MD, PhD
University of Hawaii, John A. Burns School of Medicine, Department of Medicine
Honolulu, HI
Presenting Author(s)
Toru Nakata, MD, PhD1, Arvin Jeremy N. Tan, MD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci Murakami, MD, FACG2
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2Queens west, Honolulu, HI
Introduction: Aortoesophageal fistula (AEF) is a rare but acutely life-threatening condition¹. In a study involving 123 surgically treated cases, 61% were secondary AEFs—most commonly due to aortic grafting (32.5%), followed by thoracic endovascular aortic repair (TEVAR) (24.4%).² Other reports have identified esophageal cancer as a cause³. We present a case of AEF secondary to an infected TEVAR graft in a patient with recent type B thoracoabdominal aortic dissection and aneurysm.
Case Description/
Methods: A 68-year-old Asian male with a remote history of type A aortic dissection s/p surgical repair, recent hx of type B thoracoabdominal dissection and aneurysm s/p two TEVARs, and chronic urinary obstruction managed with a suprapubic catheter (SPC), was admitted for evaluation of a urinary tract infection (UTI). He had been well until one week prior, when he developed fever, chills, and dysuria. His SPC was exchanged, and a five-day course of oral ciprofloxacin resolved the fever, though urinary symptoms persisted. On admission, he was started on IV cefepime and vancomycin. Blood cultures grew Gemella haemolysans. Two days later, he had hematemesis with a hemoglobin drop from 9.9 to 6.9 g/dL. EGD showed an esophageal ulcer with recent bleeding in the mid-esophagus (Fig. 1). CTA revealed multifocal gas within the aneurysm sac and false lumen around the stent graft, consistent with an aorto-esophageal fistula (AEF) (Fig. 2). Vascular surgery was consulted, but due to his frailty, graft explantation was deferred. He was transitioned to comfort care and passed away the following day.
Discussion: AEF is an extremely rare but critically life-threatening condition¹. Reported outcomes in a series of 10 patients with TEVAR graft infections complicated by AEF had a perioperative mortality rate of 70%. Seven of the ten patients died from hemorrhage and infection, and only three survived to hospital discharge 4. In our case, the patient developed bacteremia from a urinary tract infection, which led to graft infection and subsequently resulted in an AEF.
Clinicians should maintain a high index of suspicion for AEF in patients presenting with hematemesis, particularly those with a history of aortic surgery, thoracic aortic aneurysm, TEVAR, or thoracic and gastrointestinal malignancies.
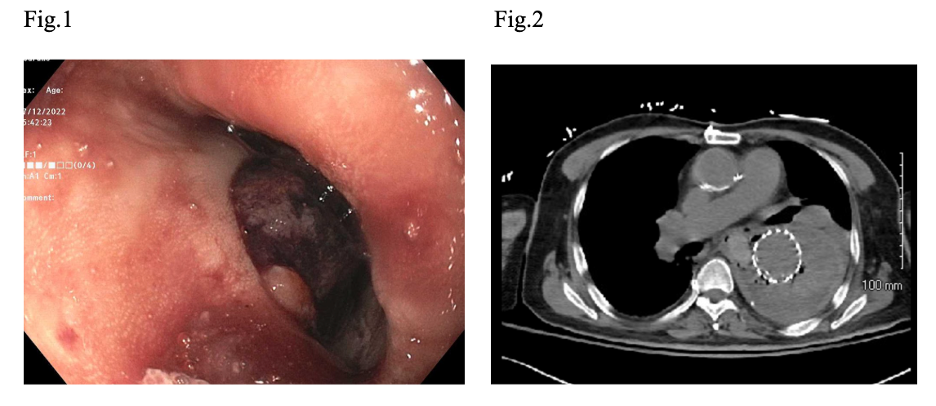
Figure: Fig.1. EGD. Aortoesophageal fistula was observed in the middle third of esophagus.
Fig.2. Abdominal CT. Multifocal gas was observed within the aneurysm sac and false lumen around the stent graft.
Disclosures:
Toru Nakata indicated no relevant financial relationships.
Arvin Jeremy Tan indicated no relevant financial relationships.
Yusuke Miyatani indicated no relevant financial relationships.
Vishal Dobaria indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Toru Nakata, MD, PhD1, Arvin Jeremy N. Tan, MD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci Murakami, MD, FACG2. P5278 - Aortoesophageal Fistula Secondary to Infected TEVAR Graft: A Fatal Complication Following UTI Bacteremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Hawaii, John A. Burns School of Medicine, Department of Medicine, Honolulu, HI; 2Queens west, Honolulu, HI
Introduction: Aortoesophageal fistula (AEF) is a rare but acutely life-threatening condition¹. In a study involving 123 surgically treated cases, 61% were secondary AEFs—most commonly due to aortic grafting (32.5%), followed by thoracic endovascular aortic repair (TEVAR) (24.4%).² Other reports have identified esophageal cancer as a cause³. We present a case of AEF secondary to an infected TEVAR graft in a patient with recent type B thoracoabdominal aortic dissection and aneurysm.
Case Description/
Methods: A 68-year-old Asian male with a remote history of type A aortic dissection s/p surgical repair, recent hx of type B thoracoabdominal dissection and aneurysm s/p two TEVARs, and chronic urinary obstruction managed with a suprapubic catheter (SPC), was admitted for evaluation of a urinary tract infection (UTI). He had been well until one week prior, when he developed fever, chills, and dysuria. His SPC was exchanged, and a five-day course of oral ciprofloxacin resolved the fever, though urinary symptoms persisted. On admission, he was started on IV cefepime and vancomycin. Blood cultures grew Gemella haemolysans. Two days later, he had hematemesis with a hemoglobin drop from 9.9 to 6.9 g/dL. EGD showed an esophageal ulcer with recent bleeding in the mid-esophagus (Fig. 1). CTA revealed multifocal gas within the aneurysm sac and false lumen around the stent graft, consistent with an aorto-esophageal fistula (AEF) (Fig. 2). Vascular surgery was consulted, but due to his frailty, graft explantation was deferred. He was transitioned to comfort care and passed away the following day.
Discussion: AEF is an extremely rare but critically life-threatening condition¹. Reported outcomes in a series of 10 patients with TEVAR graft infections complicated by AEF had a perioperative mortality rate of 70%. Seven of the ten patients died from hemorrhage and infection, and only three survived to hospital discharge 4. In our case, the patient developed bacteremia from a urinary tract infection, which led to graft infection and subsequently resulted in an AEF.
Clinicians should maintain a high index of suspicion for AEF in patients presenting with hematemesis, particularly those with a history of aortic surgery, thoracic aortic aneurysm, TEVAR, or thoracic and gastrointestinal malignancies.
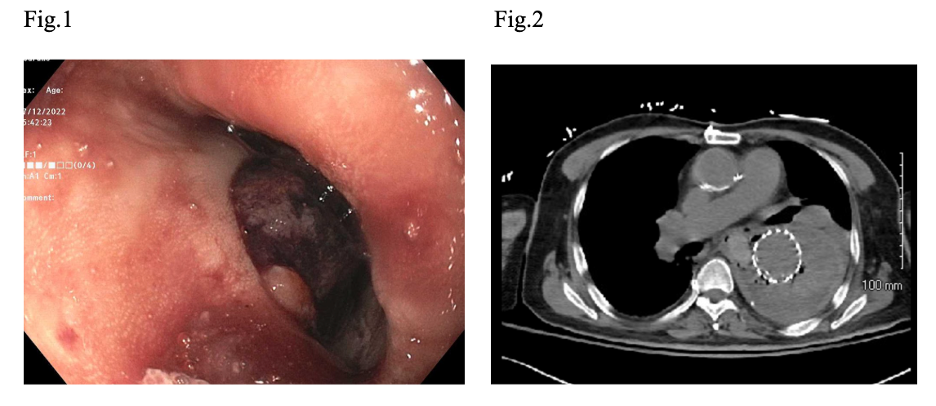
Figure: Fig.1. EGD. Aortoesophageal fistula was observed in the middle third of esophagus.
Fig.2. Abdominal CT. Multifocal gas was observed within the aneurysm sac and false lumen around the stent graft.
Disclosures:
Toru Nakata indicated no relevant financial relationships.
Arvin Jeremy Tan indicated no relevant financial relationships.
Yusuke Miyatani indicated no relevant financial relationships.
Vishal Dobaria indicated no relevant financial relationships.
Traci Murakami indicated no relevant financial relationships.
Toru Nakata, MD, PhD1, Arvin Jeremy N. Tan, MD1, Yusuke Miyatani, MD1, Vishal Dobaria, MD1, Traci Murakami, MD, FACG2. P5278 - Aortoesophageal Fistula Secondary to Infected TEVAR Graft: A Fatal Complication Following UTI Bacteremia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
