Tuesday Poster Session
Category: GI Bleeding
P5277 - Severe Duodenal Ulcer Bleeding Mimicking a Pancreatic Mass and Presenting With Hematochezia
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abdelaziz Mohamed, MBBS (he/him/his)
One Brooklyn Health-Interfaith Medical Center
Brooklyn, NY
Presenting Author(s)
Abdelaziz Mohamed, MBBS1, Adedeji Adenusi, MD, MPH1, Emad Tawadros Boshra, MD2, Yasir Ali, MD3, Mohammad Hassan, MD4, Sam brooklyn Health - Interfa. Weissman, MD1
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Brookdale University Hospital Medical Center, Brooklyn, NY; 3One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 4One Brooklyn Health, Interfaith Medical Center, Brooklyn, NY
Introduction: Duodenal ulcers are the most common subtype of peptic ulcer disease and are associated with an increased risk of bleeding and poor clinical outcomes. The clinical presentation can vary widely depending on the severity at diagnosis, ranging from asymptomatic cases to severe gastrointestinal bleeding or perforation. Pancreatic masses often raise significant concern for malignancy, especially when accompanied by gastrointestinal symptoms. We present a case of a bleeding duodenal ulcer that mimicked a pancreatic mass on imaging and manifested with massive hematochezia.
Case Description/
Methods: A 60-year-old man with a history of hypertension, type 2 diabetes mellitus, and end-stage renal disease presented with abdominal pain and non-bloody vomiting for three weeks. His vital signs were stable, and physical examination was unremarkable. Initial laboratory findings showed a hemoglobin (Hb) level of 8.5 g/dL. A CT scan of the abdomen revealed an 8 × 6 cm soft tissue mass in the head of the pancreas involving the first and second portions of the duodenum, with obliteration of the bowel lumen (Figure 1, Image A). Six hours after presentation, the patient experienced massive rectal bleeding estimated at 150–200 mL, resulting in hypotension and a drop in Hb to 5.3 g/dL. Upper endoscopy (EGD) revealed severe duodenitis and a duodenal ulcer with an actively oozing artery (Forest classification Ib) (Figure 2). Hemostasis was achieved using epinephrine and argon plasma coagulation (APC). CT abdominal angiography showed no active bleeding vessel and demonstrated a significant reduction in the size of the previously noted soft tissue mass at the head of the pancreas (Figure 1, Image B). Follow-up MRI confirmed resolution of the pancreatic soft tissue mass, with no evidence of an underlying pancreatic lesion.
Discussion: A localized hemorrhage from a bleeding duodenal ulcer can mimic a pancreatic or periampullary soft tissue mass on imaging. Accurate diagnosis and a high index of clinical suspicion are crucial for differentiating a true pancreatic mass from mimicking lesions, especially in cases of severe duodenal ulcer bleeding.
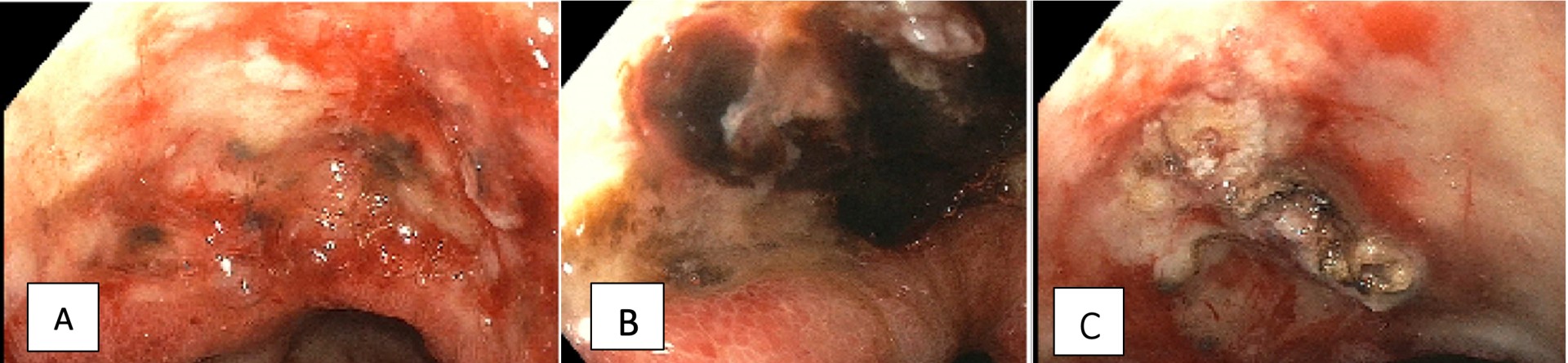
Figure: Figure 1. CT Abdomen on day 1 (Image A) showing a 6 cm soft tissue mass in the head of the pancreas. CT Abdomen on day 2 (Image B) showing a reduction of the soft tissue mass to 3 cm.
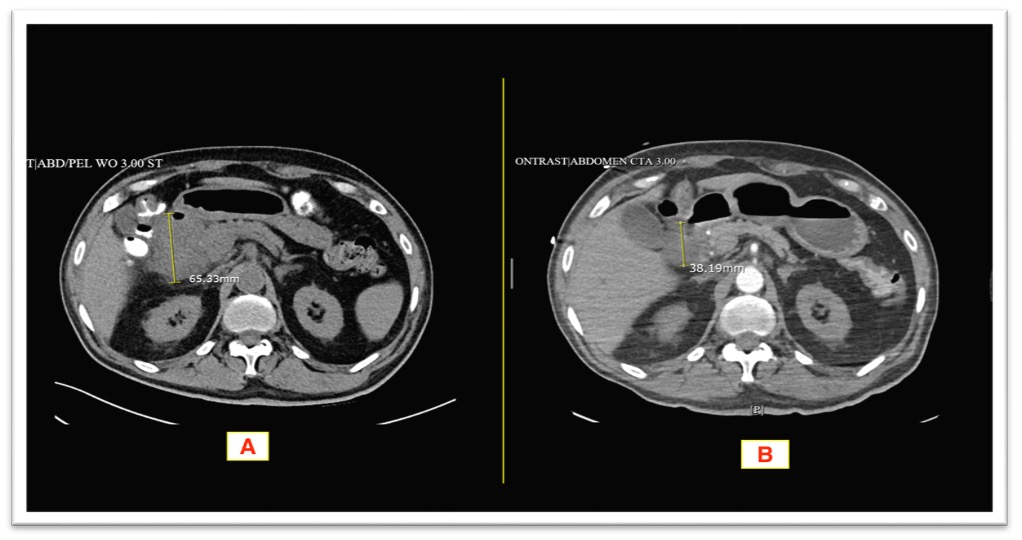
Figure: Figure 2. Showing (A) Duodenitis. (B) Duodenal ulcer with active bleeding. (C) Bleeding vessel following epinephrine and argon plasma coagulation (APC) injection.
Disclosures:
Abdelaziz Mohamed indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Emad Tawadros Boshra indicated no relevant financial relationships.
Yasir Ali indicated no relevant financial relationships.
Mohammad Hassan indicated no relevant financial relationships.
Sam Weissman indicated no relevant financial relationships.
Abdelaziz Mohamed, MBBS1, Adedeji Adenusi, MD, MPH1, Emad Tawadros Boshra, MD2, Yasir Ali, MD3, Mohammad Hassan, MD4, Sam brooklyn Health - Interfa. Weissman, MD1. P5277 - Severe Duodenal Ulcer Bleeding Mimicking a Pancreatic Mass and Presenting With Hematochezia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1One Brooklyn Health-Interfaith Medical Center, Brooklyn, NY; 2Brookdale University Hospital Medical Center, Brooklyn, NY; 3One Brooklyn Health-Brookdale University Hospital Medical Center, Brooklyn, NY; 4One Brooklyn Health, Interfaith Medical Center, Brooklyn, NY
Introduction: Duodenal ulcers are the most common subtype of peptic ulcer disease and are associated with an increased risk of bleeding and poor clinical outcomes. The clinical presentation can vary widely depending on the severity at diagnosis, ranging from asymptomatic cases to severe gastrointestinal bleeding or perforation. Pancreatic masses often raise significant concern for malignancy, especially when accompanied by gastrointestinal symptoms. We present a case of a bleeding duodenal ulcer that mimicked a pancreatic mass on imaging and manifested with massive hematochezia.
Case Description/
Methods: A 60-year-old man with a history of hypertension, type 2 diabetes mellitus, and end-stage renal disease presented with abdominal pain and non-bloody vomiting for three weeks. His vital signs were stable, and physical examination was unremarkable. Initial laboratory findings showed a hemoglobin (Hb) level of 8.5 g/dL. A CT scan of the abdomen revealed an 8 × 6 cm soft tissue mass in the head of the pancreas involving the first and second portions of the duodenum, with obliteration of the bowel lumen (Figure 1, Image A). Six hours after presentation, the patient experienced massive rectal bleeding estimated at 150–200 mL, resulting in hypotension and a drop in Hb to 5.3 g/dL. Upper endoscopy (EGD) revealed severe duodenitis and a duodenal ulcer with an actively oozing artery (Forest classification Ib) (Figure 2). Hemostasis was achieved using epinephrine and argon plasma coagulation (APC). CT abdominal angiography showed no active bleeding vessel and demonstrated a significant reduction in the size of the previously noted soft tissue mass at the head of the pancreas (Figure 1, Image B). Follow-up MRI confirmed resolution of the pancreatic soft tissue mass, with no evidence of an underlying pancreatic lesion.
Discussion: A localized hemorrhage from a bleeding duodenal ulcer can mimic a pancreatic or periampullary soft tissue mass on imaging. Accurate diagnosis and a high index of clinical suspicion are crucial for differentiating a true pancreatic mass from mimicking lesions, especially in cases of severe duodenal ulcer bleeding.
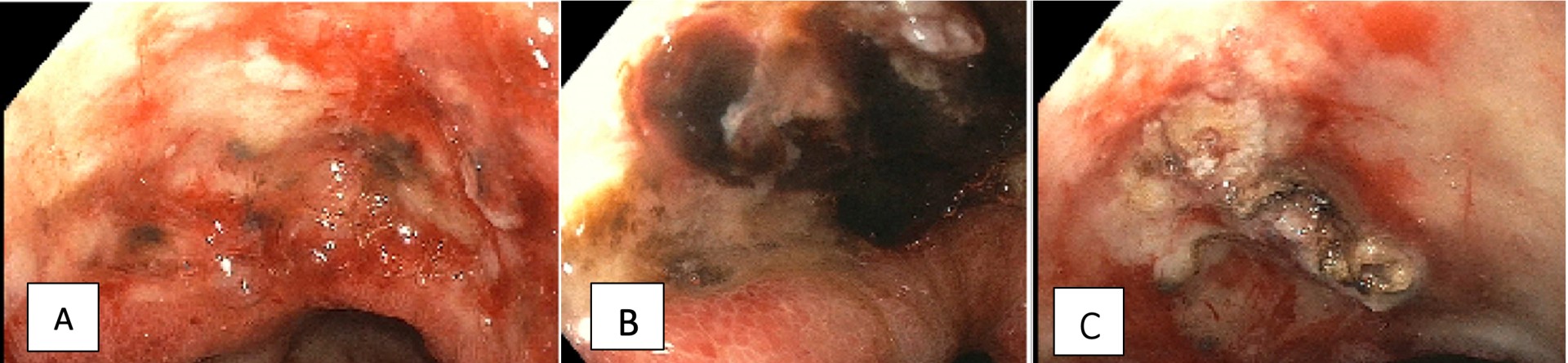
Figure: Figure 1. CT Abdomen on day 1 (Image A) showing a 6 cm soft tissue mass in the head of the pancreas. CT Abdomen on day 2 (Image B) showing a reduction of the soft tissue mass to 3 cm.
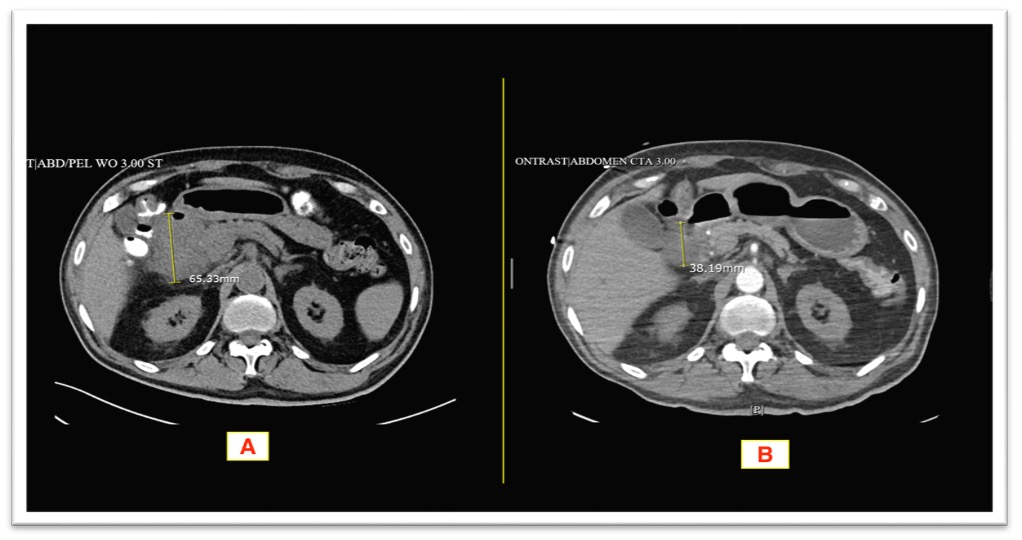
Figure: Figure 2. Showing (A) Duodenitis. (B) Duodenal ulcer with active bleeding. (C) Bleeding vessel following epinephrine and argon plasma coagulation (APC) injection.
Disclosures:
Abdelaziz Mohamed indicated no relevant financial relationships.
Adedeji Adenusi indicated no relevant financial relationships.
Emad Tawadros Boshra indicated no relevant financial relationships.
Yasir Ali indicated no relevant financial relationships.
Mohammad Hassan indicated no relevant financial relationships.
Sam Weissman indicated no relevant financial relationships.
Abdelaziz Mohamed, MBBS1, Adedeji Adenusi, MD, MPH1, Emad Tawadros Boshra, MD2, Yasir Ali, MD3, Mohammad Hassan, MD4, Sam brooklyn Health - Interfa. Weissman, MD1. P5277 - Severe Duodenal Ulcer Bleeding Mimicking a Pancreatic Mass and Presenting With Hematochezia, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
