Tuesday Poster Session
Category: GI Bleeding
P5245 - Endoscopic Ultrasound as a Diagnostic Tool in Obscure GI Bleeding: A Rare Case of Left Gastric Artery Pseudoaneurysm Mimicking Gastric Varices
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sharifeh Almasaid, MD, MPH (she/her/hers)
SUNY Upstate Medical University
Syracuse, NY
Presenting Author(s)
Sharifeh Almasaid, MD, MPH1, Avleen Kaur, MD1, Dayana Nasr, MD2, Mark M. Aloysius, PhD, ABOM, NBPNS1, Bishnu Sapkota, MD, FACG1
1SUNY Upstate Medical University, Syracuse, NY; 2SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Obscure gastrointestinal bleeding (OGIB) accounts for ~5% of all GI bleeds. Diagnosis may require advanced tests after a negative initial workup, including capsule endoscopy, balloon-assisted enteroscopy, CT/MR enterography, tagged RBC scans, or angiography. Common causes include angiodysplasia, small bowel tumors, NSAID enteropathy, Meckel’s diverticulum, and Crohn’s disease. Rarely, life-threatening sources like visceral artery pseudoaneurysms (VAPA) occur. We present a rare case of OGIB from a left gastric artery pseudoaneurysm in an 81-year-old man.
Case Description/
Methods: An 81-year-old man presented with worsening exertional dyspnea and two episodes of bright red blood per rectum. He had no history of cirrhosis or pancreatitis and was hemodynamically stable. Labs showed acute chronic anemia (Hgb drop from 12 to 7 g/dL), with normal platelets and a coagulation profile. An esophagogastroduodenoscopy, colonoscopy, and tagged RBC scan were non-diagnostic. Single balloon enteroscopy revealed slow oozing in the gastric body and fundus, concerning for gastric varices. EUS showed submucosal vascular structures consistent with gastric and perigastric varices and a 3 cm complex cystic lesion between the posterior gastric body and pancreas, involving the splenic artery and vein (figure 1). Hemostasis was temporarily achieved with epinephrine and Endo Clot; the varices were unsuitable for banding. CT angiogram showed a pseudoaneurysm near the lesser curvature from a branch of the left gastric artery. IR angiogram (figure 2) confirmed this and coil embolization was successfully performed.
Discussion: VAPAs cause < 1% of GI bleeds and are often asymptomatic, making diagnosis difficult despite mortality rates up to 50%. Etiologies include trauma, atherosclerosis, or chronic inflammation like pancreatitis. The splenic artery is most affected (~60%), followed by the gastroduodenal and hepatic arteries. Left gastric artery (LGA) pseudoaneurysms are extremely rare, typically diagnosed via CT angiography. This is the first reported LGA pseudoaneurysm diagnosed with EUS. While EUS is useful for submucosal and extraluminal lesions, no guidelines exist for its use in OGIB. It should be considered when vascular or extrinsic causes are suspected, and standard tests are negative. More research is needed to clarify its diagnostic role and establish protocols.
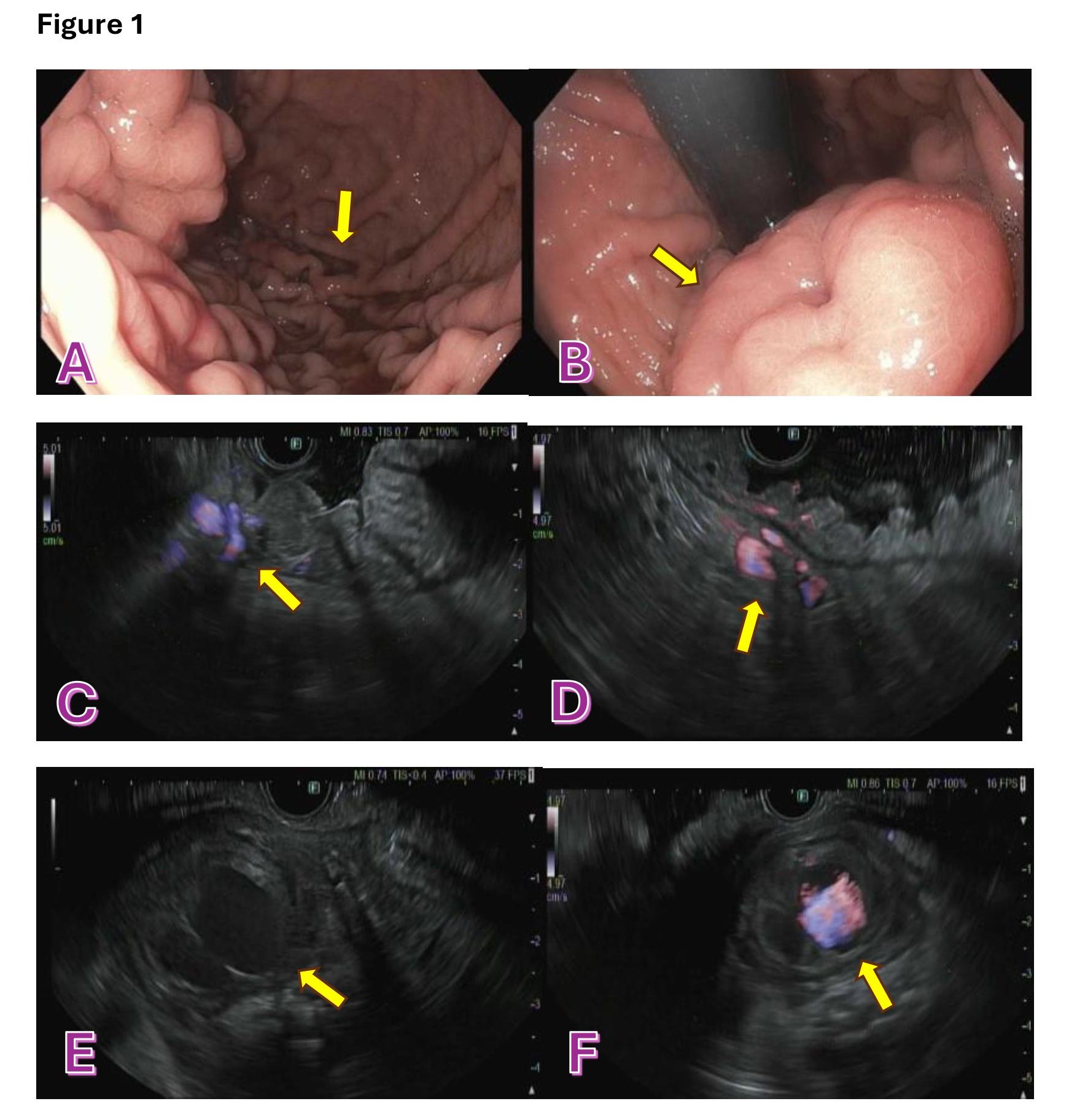
Figure: A: EGD showing active oozing in the gastric body and fundus
B: EGD showing prominent and poorly distensible folds
C,D: EUS showing submucosal vascular structures consistent with gastric and pergastric varices
E: EUS showing a 3 cm complex cystic lesion located between the posterior gastric body and pancreas
F: EUS doppler showing vascular flow in the identified cystic lesion
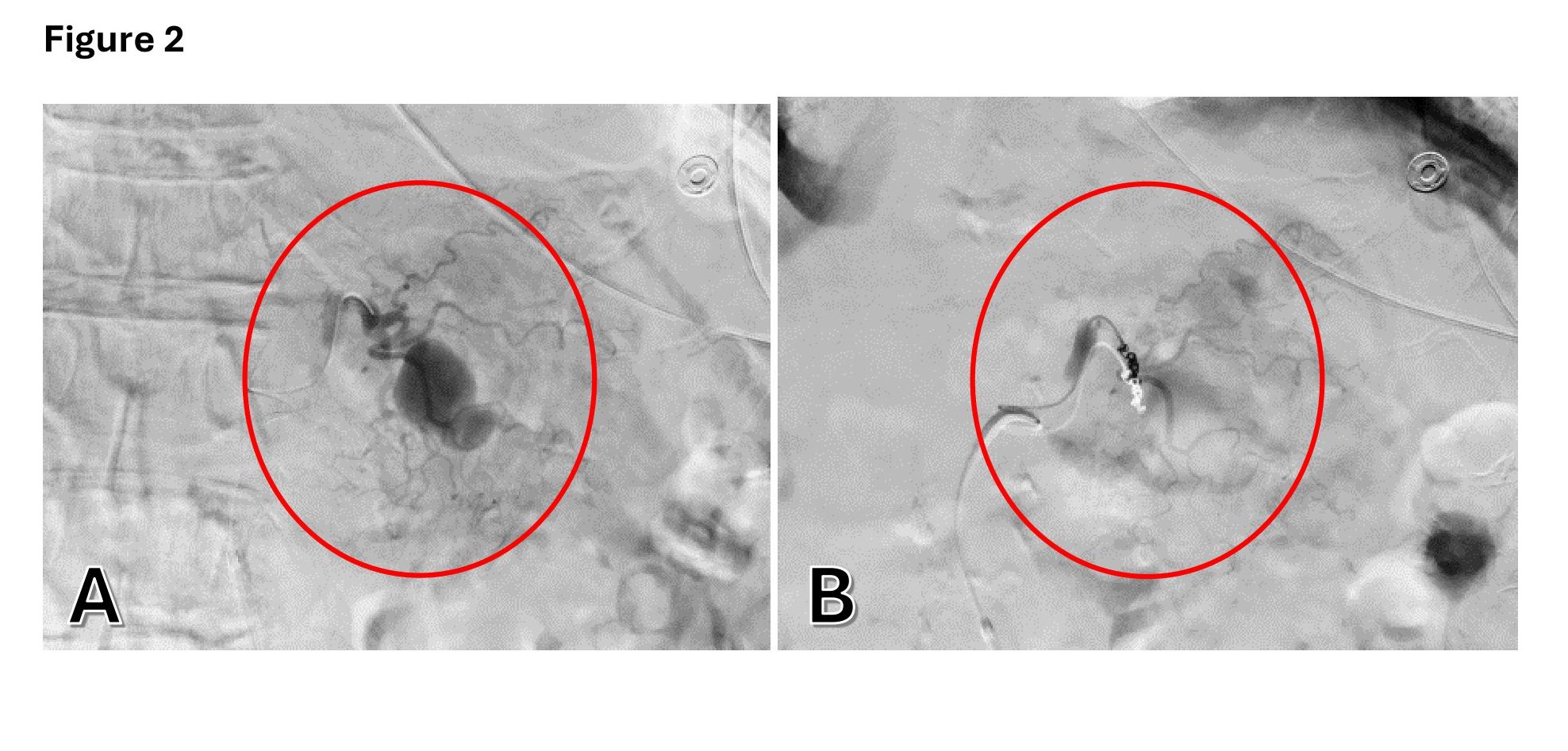
Figure: A: IR angiogram showing a pseudoaneurysm arising from a branch of the left gastric artery stemming from the gastrohepatic trunk.
B: IR angiogram showing a successful coil embolization for the pseudoaneurysm
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Dayana Nasr indicated no relevant financial relationships.
Mark Aloysius indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Sharifeh Almasaid, MD, MPH1, Avleen Kaur, MD1, Dayana Nasr, MD2, Mark M. Aloysius, PhD, ABOM, NBPNS1, Bishnu Sapkota, MD, FACG1. P5245 - Endoscopic Ultrasound as a Diagnostic Tool in Obscure GI Bleeding: A Rare Case of Left Gastric Artery Pseudoaneurysm Mimicking Gastric Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1SUNY Upstate Medical University, Syracuse, NY; 2SUNY Upstate Medical University Hospital, Syracuse, NY
Introduction: Obscure gastrointestinal bleeding (OGIB) accounts for ~5% of all GI bleeds. Diagnosis may require advanced tests after a negative initial workup, including capsule endoscopy, balloon-assisted enteroscopy, CT/MR enterography, tagged RBC scans, or angiography. Common causes include angiodysplasia, small bowel tumors, NSAID enteropathy, Meckel’s diverticulum, and Crohn’s disease. Rarely, life-threatening sources like visceral artery pseudoaneurysms (VAPA) occur. We present a rare case of OGIB from a left gastric artery pseudoaneurysm in an 81-year-old man.
Case Description/
Methods: An 81-year-old man presented with worsening exertional dyspnea and two episodes of bright red blood per rectum. He had no history of cirrhosis or pancreatitis and was hemodynamically stable. Labs showed acute chronic anemia (Hgb drop from 12 to 7 g/dL), with normal platelets and a coagulation profile. An esophagogastroduodenoscopy, colonoscopy, and tagged RBC scan were non-diagnostic. Single balloon enteroscopy revealed slow oozing in the gastric body and fundus, concerning for gastric varices. EUS showed submucosal vascular structures consistent with gastric and perigastric varices and a 3 cm complex cystic lesion between the posterior gastric body and pancreas, involving the splenic artery and vein (figure 1). Hemostasis was temporarily achieved with epinephrine and Endo Clot; the varices were unsuitable for banding. CT angiogram showed a pseudoaneurysm near the lesser curvature from a branch of the left gastric artery. IR angiogram (figure 2) confirmed this and coil embolization was successfully performed.
Discussion: VAPAs cause < 1% of GI bleeds and are often asymptomatic, making diagnosis difficult despite mortality rates up to 50%. Etiologies include trauma, atherosclerosis, or chronic inflammation like pancreatitis. The splenic artery is most affected (~60%), followed by the gastroduodenal and hepatic arteries. Left gastric artery (LGA) pseudoaneurysms are extremely rare, typically diagnosed via CT angiography. This is the first reported LGA pseudoaneurysm diagnosed with EUS. While EUS is useful for submucosal and extraluminal lesions, no guidelines exist for its use in OGIB. It should be considered when vascular or extrinsic causes are suspected, and standard tests are negative. More research is needed to clarify its diagnostic role and establish protocols.
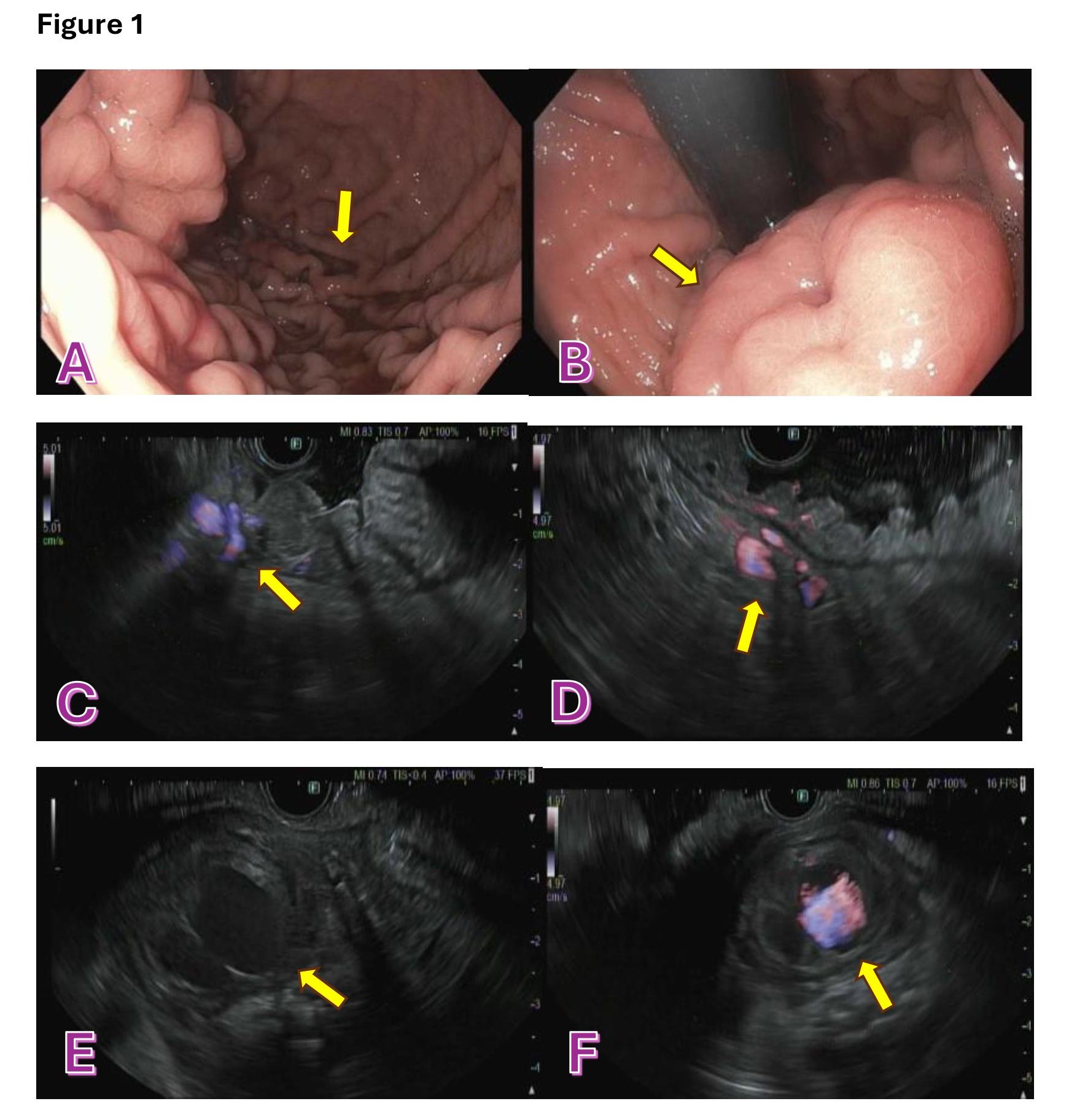
Figure: A: EGD showing active oozing in the gastric body and fundus
B: EGD showing prominent and poorly distensible folds
C,D: EUS showing submucosal vascular structures consistent with gastric and pergastric varices
E: EUS showing a 3 cm complex cystic lesion located between the posterior gastric body and pancreas
F: EUS doppler showing vascular flow in the identified cystic lesion
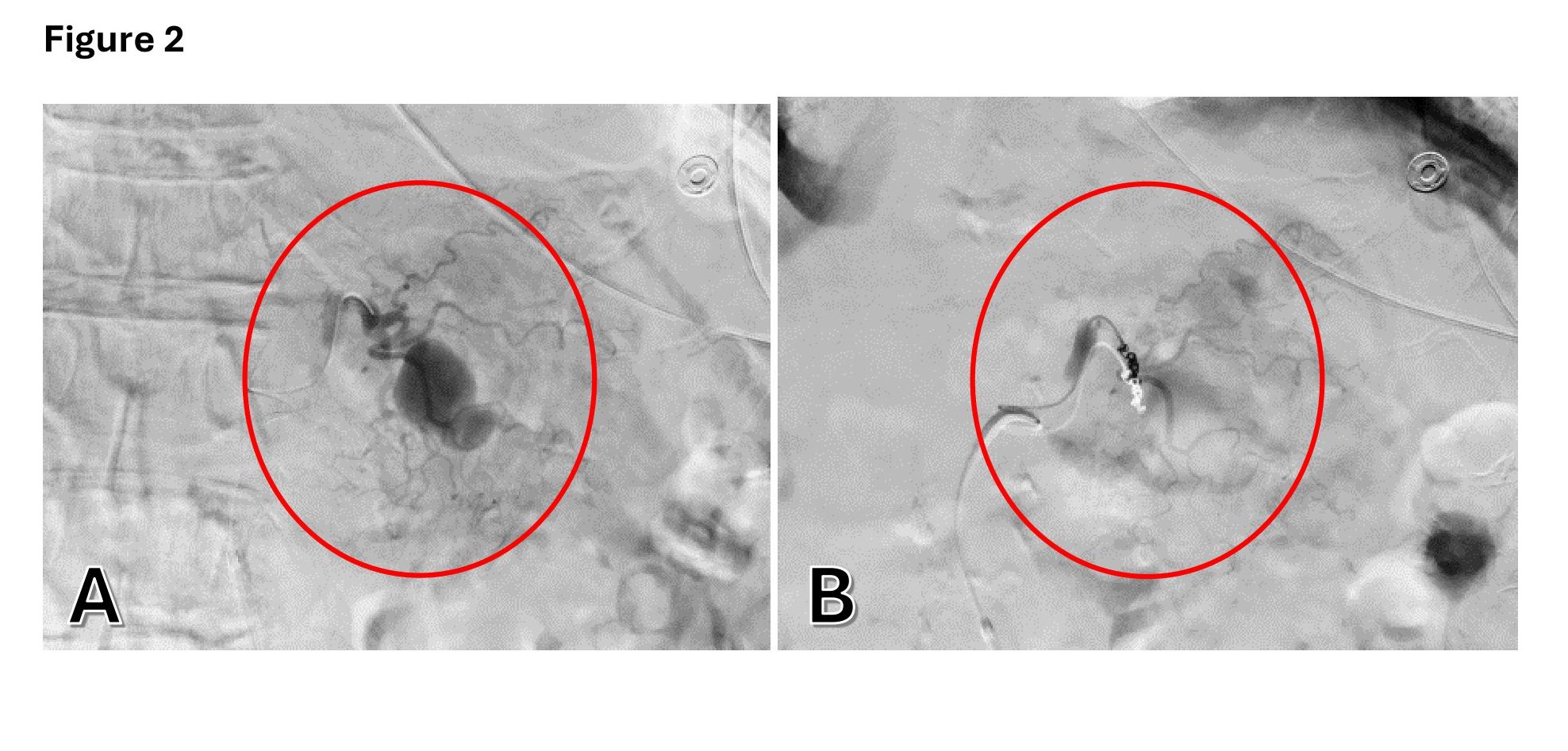
Figure: A: IR angiogram showing a pseudoaneurysm arising from a branch of the left gastric artery stemming from the gastrohepatic trunk.
B: IR angiogram showing a successful coil embolization for the pseudoaneurysm
Disclosures:
Sharifeh Almasaid indicated no relevant financial relationships.
Avleen Kaur indicated no relevant financial relationships.
Dayana Nasr indicated no relevant financial relationships.
Mark Aloysius indicated no relevant financial relationships.
Bishnu Sapkota indicated no relevant financial relationships.
Sharifeh Almasaid, MD, MPH1, Avleen Kaur, MD1, Dayana Nasr, MD2, Mark M. Aloysius, PhD, ABOM, NBPNS1, Bishnu Sapkota, MD, FACG1. P5245 - Endoscopic Ultrasound as a Diagnostic Tool in Obscure GI Bleeding: A Rare Case of Left Gastric Artery Pseudoaneurysm Mimicking Gastric Varices, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

