Tuesday Poster Session
Category: GI Bleeding
P5229 - A Tale of Two Duodenal Diverticula: An Unusual Case Series of Upper GI Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Jeremy Polman, DO, MS, MBA
Lenox Hill Hospital, Northwell Health
New York, NY
Presenting Author(s)
Jeremy Polman, DO, MS, MBA, Joshua Wynne, MD, Isabella Bergagnini, DO, Steven Shamah, MD
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Duodenal diverticula are an uncommon anatomical variant and are typically asymptomatic. Duodenal diverticula can rarely lead to a wide range of pathologies, some of which could become life threatening. Here we present two patients with clinically relevant duodenal diverticula, one of which is life threatening.
Case Description/
Methods: A 77-year-old male with chronic iron deficiency anemia presented to the Emergency Department with fatigue and weakness. Patient was first diagnosed with iron deficiency anemia as an outpatient four months prior. He completed EGD and colonoscopy at that time, which were normal. His symptoms increased in severity, culminating in pre-syncopal episodes. Outpatient CBC identified hemoglobin of 6.4 g/dL for which he presented to the Emergency Department. Upon presentation, patient appeared comfortable with normal vital signs and rectal exam. Given recent bidirectional endoscopic evaluation, capsule endoscopy was performed which identified many drops of bright red blood in the proximal duodenum. A push enteroscopy was then performed which identified numerous large, not actively bleeding duodenal diverticula with many large superficial blood vessels along the interior of the diverticula. Given self-resolution of diverticular bleeding, no intervention was required. The patient remained hemodynamically stable and was discharged with plans to continue iron supplementation. A 79-year-old female presented to the Emergency Department with dizziness and melena. At the time of presentation, patient was hypotensive with blood pressure of 77/39, hemoglobin of 6.9 g/dL, and with large volume melena. An emergent upper endoscopy was performed, which identified large volume bright red liquid blood diffusely in stomach and duodenum. Inspection of the second portion of the duodenum identified a large duodenal diverticula filled with an adherent clot. After clot removal, an actively hemorrhaging superficial blood vessel was identified inside the duodenal diverticula. Hemostasis was achieved with four 1cc injections of epinephrine along the walls of the diverticula and application of hemostatic powder. Post procedurally, the patient became hemodynamically stable with resolution of melena. Patient was ultimately discharged without recurrence of presenting complaints.
Discussion: This case series outlines two cases of duodenal diverticular bleeding and should encourage physicians to consider this diagnosis as a potential source of both hemodynamically stable and unstable upper GI bleeding.
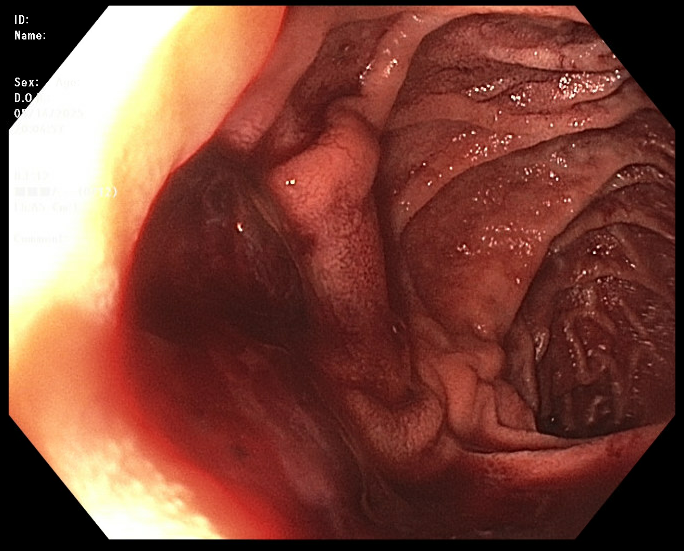
Figure: Case 1: Three large non-bleeding duodenal diverticula in second portion of duodenum with a prominent blood vessel seen in most proximal diverticula.

Figure: Case 2: One large, actively bleeding duodenal diverticula in the second portion of the duodenum.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Joshua Wynne indicated no relevant financial relationships.
Isabella Bergagnini indicated no relevant financial relationships.
Steven Shamah: Boston Scientific – Consultant.
Jeremy Polman, DO, MS, MBA, Joshua Wynne, MD, Isabella Bergagnini, DO, Steven Shamah, MD. P5229 - A Tale of Two Duodenal Diverticula: An Unusual Case Series of Upper GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Duodenal diverticula are an uncommon anatomical variant and are typically asymptomatic. Duodenal diverticula can rarely lead to a wide range of pathologies, some of which could become life threatening. Here we present two patients with clinically relevant duodenal diverticula, one of which is life threatening.
Case Description/
Methods: A 77-year-old male with chronic iron deficiency anemia presented to the Emergency Department with fatigue and weakness. Patient was first diagnosed with iron deficiency anemia as an outpatient four months prior. He completed EGD and colonoscopy at that time, which were normal. His symptoms increased in severity, culminating in pre-syncopal episodes. Outpatient CBC identified hemoglobin of 6.4 g/dL for which he presented to the Emergency Department. Upon presentation, patient appeared comfortable with normal vital signs and rectal exam. Given recent bidirectional endoscopic evaluation, capsule endoscopy was performed which identified many drops of bright red blood in the proximal duodenum. A push enteroscopy was then performed which identified numerous large, not actively bleeding duodenal diverticula with many large superficial blood vessels along the interior of the diverticula. Given self-resolution of diverticular bleeding, no intervention was required. The patient remained hemodynamically stable and was discharged with plans to continue iron supplementation. A 79-year-old female presented to the Emergency Department with dizziness and melena. At the time of presentation, patient was hypotensive with blood pressure of 77/39, hemoglobin of 6.9 g/dL, and with large volume melena. An emergent upper endoscopy was performed, which identified large volume bright red liquid blood diffusely in stomach and duodenum. Inspection of the second portion of the duodenum identified a large duodenal diverticula filled with an adherent clot. After clot removal, an actively hemorrhaging superficial blood vessel was identified inside the duodenal diverticula. Hemostasis was achieved with four 1cc injections of epinephrine along the walls of the diverticula and application of hemostatic powder. Post procedurally, the patient became hemodynamically stable with resolution of melena. Patient was ultimately discharged without recurrence of presenting complaints.
Discussion: This case series outlines two cases of duodenal diverticular bleeding and should encourage physicians to consider this diagnosis as a potential source of both hemodynamically stable and unstable upper GI bleeding.
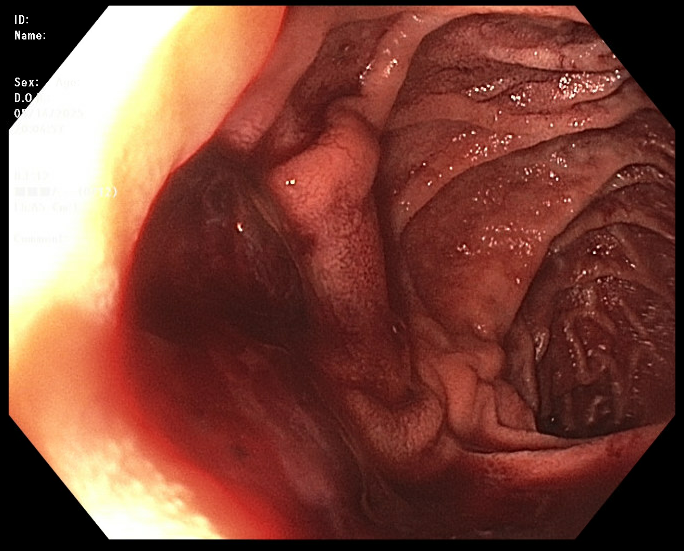
Figure: Case 1: Three large non-bleeding duodenal diverticula in second portion of duodenum with a prominent blood vessel seen in most proximal diverticula.

Figure: Case 2: One large, actively bleeding duodenal diverticula in the second portion of the duodenum.
Disclosures:
Jeremy Polman indicated no relevant financial relationships.
Joshua Wynne indicated no relevant financial relationships.
Isabella Bergagnini indicated no relevant financial relationships.
Steven Shamah: Boston Scientific – Consultant.
Jeremy Polman, DO, MS, MBA, Joshua Wynne, MD, Isabella Bergagnini, DO, Steven Shamah, MD. P5229 - A Tale of Two Duodenal Diverticula: An Unusual Case Series of Upper GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
