Tuesday Poster Session
Category: GI Bleeding
P5225 - Rare Cause of Obscure Overt GI Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- DS
David R. Sonnentag, BS (he/him/his)
Emplify Health
La Crosse, Wisconsin
Presenting Author(s)
David R. Sonnestag, BS, Jatinder P. Ahluwalia, MD
Emplify Health, La Crosse, WI
Introduction: Precise and prompt identification of the underlying cause often remains challenging in patients with obscure overt GI bleeding. We describe a patient with recurrent GI bleeding and an extensive endoscopic workup who was ultimately found to have a rare GI malignancy.
Case Description/
Methods: A 65-year-old man with HTN and atrial fibrillation for which he was on Eliquis presented to the ER with marked weakness and fatigue for a few months, but no change in stool color or frequency. Labs showed severe microcytic anemia with hemoglobin (Hb) 3.9 g/dL (baseline 16.7 g/dL 16 months prior), WBC 5.9 K/uL, ferritin 4 ng/mL, total bilirubin 0.3 ng/dL and haptoglobin 69 mg/dL. EGD and colonoscopy did not identify a source of blood loss. Bleeding stopped and he was discharged to home with Hb 7.5 g/dL and recommendation to hold iron supplementation and Eliquis. Outpatient small bowel capsule endoscopy (CE) was negative. Hb rose gradually to 11.4 g/dL. One month later, he returned to the ER with increased weakness, dyspnea, and blood in stool when Hb was 8.1 g/dL. Repeat EGD, colonoscopy, and CE again revealed no bleeding source. Bleeding stopped and he was discharged with Hb 7.9 g/dL which increased gradually to 9.4 g/dL after discharge. Nine days later, he was readmitted to the hospital for the 3rd time after presenting to the ER with 5 days of black-maroon stools associated with lightheadedness. Hb was 5.9 g/dL. Based on the stool color, small bowel (SB) was suspected to be the source and a push enteroscopy was done but was unrevealing. Repeat CE done the same day showed blood-tinged stool in the cecum with increasing intensity of redness over time prompting a repeat colonoscopy that was negative further substantiating a SB source. Hence, prompt angiographic evaluation was requested and showed bleeding in the ileum but bleeding remitted before super-selective catheterization could be done. An embolization coil was placed for localization and he underwent surgical resection of 24 cm of the ileum. Histopathology of the resected specimen revealed follicular lymphoma (FL). He had no bleeding after surgery and was discharged with Hb 8.1 g/dL. He reported no bloody stools at his 1-month follow-up when Hb was 12.4 g/dL.
Discussion: Only a few cases of FL presenting with GI bleeding have been reported. This case underscores challenges in identifying SB bleeding and highlights the importance of prompt utilization of CE and arteriography after negative endoscopy in patients with recurrent obscure overt GI bleeding.
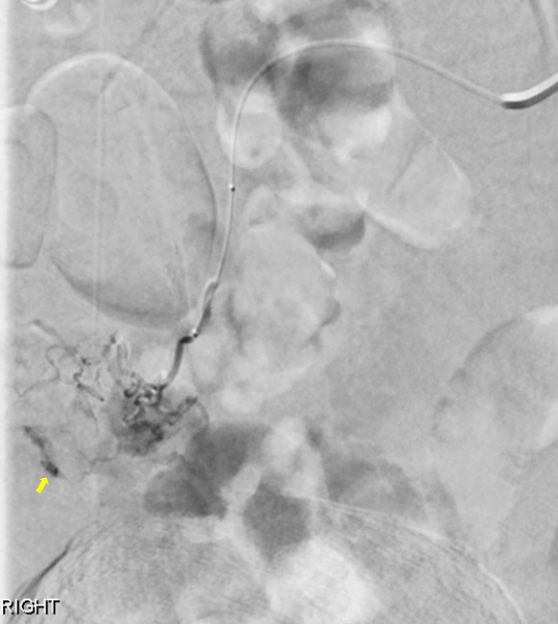
Figure: Arteriography showing catheter in the distal superior mesenteric artery with extravasation of the contrast in the ileum (yellow arrow).

Figure: Histopathology of the resected ileal specimen showing classic follicular lymphoma (H&E, x 40).
Disclosures:
David Sonnestag indicated no relevant financial relationships.
Jatinder Ahluwalia indicated no relevant financial relationships.
David R. Sonnestag, BS, Jatinder P. Ahluwalia, MD. P5225 - Rare Cause of Obscure Overt GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Emplify Health, La Crosse, WI
Introduction: Precise and prompt identification of the underlying cause often remains challenging in patients with obscure overt GI bleeding. We describe a patient with recurrent GI bleeding and an extensive endoscopic workup who was ultimately found to have a rare GI malignancy.
Case Description/
Methods: A 65-year-old man with HTN and atrial fibrillation for which he was on Eliquis presented to the ER with marked weakness and fatigue for a few months, but no change in stool color or frequency. Labs showed severe microcytic anemia with hemoglobin (Hb) 3.9 g/dL (baseline 16.7 g/dL 16 months prior), WBC 5.9 K/uL, ferritin 4 ng/mL, total bilirubin 0.3 ng/dL and haptoglobin 69 mg/dL. EGD and colonoscopy did not identify a source of blood loss. Bleeding stopped and he was discharged to home with Hb 7.5 g/dL and recommendation to hold iron supplementation and Eliquis. Outpatient small bowel capsule endoscopy (CE) was negative. Hb rose gradually to 11.4 g/dL. One month later, he returned to the ER with increased weakness, dyspnea, and blood in stool when Hb was 8.1 g/dL. Repeat EGD, colonoscopy, and CE again revealed no bleeding source. Bleeding stopped and he was discharged with Hb 7.9 g/dL which increased gradually to 9.4 g/dL after discharge. Nine days later, he was readmitted to the hospital for the 3rd time after presenting to the ER with 5 days of black-maroon stools associated with lightheadedness. Hb was 5.9 g/dL. Based on the stool color, small bowel (SB) was suspected to be the source and a push enteroscopy was done but was unrevealing. Repeat CE done the same day showed blood-tinged stool in the cecum with increasing intensity of redness over time prompting a repeat colonoscopy that was negative further substantiating a SB source. Hence, prompt angiographic evaluation was requested and showed bleeding in the ileum but bleeding remitted before super-selective catheterization could be done. An embolization coil was placed for localization and he underwent surgical resection of 24 cm of the ileum. Histopathology of the resected specimen revealed follicular lymphoma (FL). He had no bleeding after surgery and was discharged with Hb 8.1 g/dL. He reported no bloody stools at his 1-month follow-up when Hb was 12.4 g/dL.
Discussion: Only a few cases of FL presenting with GI bleeding have been reported. This case underscores challenges in identifying SB bleeding and highlights the importance of prompt utilization of CE and arteriography after negative endoscopy in patients with recurrent obscure overt GI bleeding.
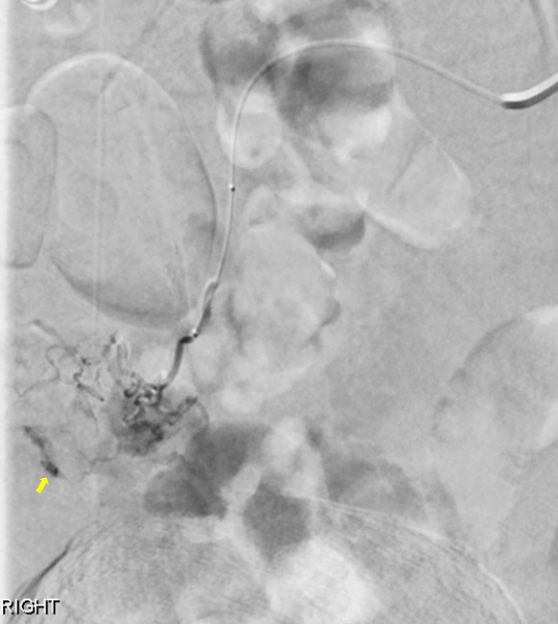
Figure: Arteriography showing catheter in the distal superior mesenteric artery with extravasation of the contrast in the ileum (yellow arrow).

Figure: Histopathology of the resected ileal specimen showing classic follicular lymphoma (H&E, x 40).
Disclosures:
David Sonnestag indicated no relevant financial relationships.
Jatinder Ahluwalia indicated no relevant financial relationships.
David R. Sonnestag, BS, Jatinder P. Ahluwalia, MD. P5225 - Rare Cause of Obscure Overt GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
