Tuesday Poster Session
Category: GI Bleeding
P5223 - Treating More Than the Bleed: Exploring Iron Status and Use of Supplementation in Acute Gastrointestinal Bleed - A Retrospective Cohort Study Using the Trinet-x Databases
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Akshay Sharma, MBBS (he/him/his)
Luminis Health Anne Arundel Medical Center
Annapolis, MD
Presenting Author(s)
Akshay Sharma, MBBS1, Nirav Agrawal, MD, MPH2, Muhammad Kazi, MD1, Mitchell Karpman, PhD1, Rahul Kumar, MD3, Sanmeet Singh, MD1, Nargiz Muganlinskaya, MD, MBA1
1Luminis Health Anne Arundel Medical Center, Annapolis, MD; 2Anne Arundel Medical Center, Luminus Health, Annapolis, MD; 3North Central Bronx Hospital, Bronx, NY
Introduction: While the primary focus in managing gastrointestinal bleeding (GIB) is controlling the bleed source, addressing iron deficiency anemia (IDA) is equally critical. Without initiating iron supplementation during hospitalization, up to 70% of acute GIB patients may experience persistent IDA at three months, leading to significant comorbidities and an annual economic burden of up to $29,511 per patient. Although, American College of Gastroenterology guidelines recommend a restrictive blood transfusion strategy for acute GIB [maintaining hemoglobin (Hb) >7 g/dL] and emphasizes iron supplementation for chronic GIB, however, no clear guidelines exist on iron assessment and deficiency management in setting of acute GIB. This study examines the gap by analyzing data from Trinet-X database to evaluate iron status assessment and supplementation initiation practices during acute GIB hospitalization.
Methods: This 5-year retrospective cohort study utilized TriNetX data (2020–2024) and included adults aged ≥18 hospitalized due to acute GIB and divided into 2 cohorts: requiring red blood cell (RBC) or whole blood transfusion. Table 1 details. We performed descriptive analysis using SQL and excel.
Results: 2,656,344 patients (45.1% female) were hospitalized with acute GIB, of which 115,325 (4.3%)patients required PRBC transfusion. Patients who received transfusions were older (mean age 66.2 vs. 59.9 years) and more likely to be female (54.2% vs. 50.5%) and non-white (41.9% vs. 36.2%) compared to those who did not require transfusion. Admission hemoglobin levels were significantly lower in the transfusion group (6.3 ± 3.8 g/dL) compared to the non-transfusion group (8.7 ± 4.7 g/dL), and discharge hemoglobin remained lower (7.2 ± 3.3 g/dL vs. 8.3 ± 4.0 g/dL). The mean pre-transfusion hemoglobin level was 7.7 g/dL. Despite severe anemia majority of patients (88.1%) in the transfused cohort had no iron panel assessment, and only 3.7% were formally diagnosed with iron deficiency anemia (IDA). Furthermore, 97.2% of transfused patients did not receive iron supplementation, highlighting a large treatment gap
Discussion: In this large cohort of patients admitted with acute GIB, blood transfusion recipients were typically older and more likely to have anemia on admission and discharge. Despite evidence of iron deficiency and a high likelihood of IDA, iron panel testing was underutilized, and iron supplementation was rarely administered
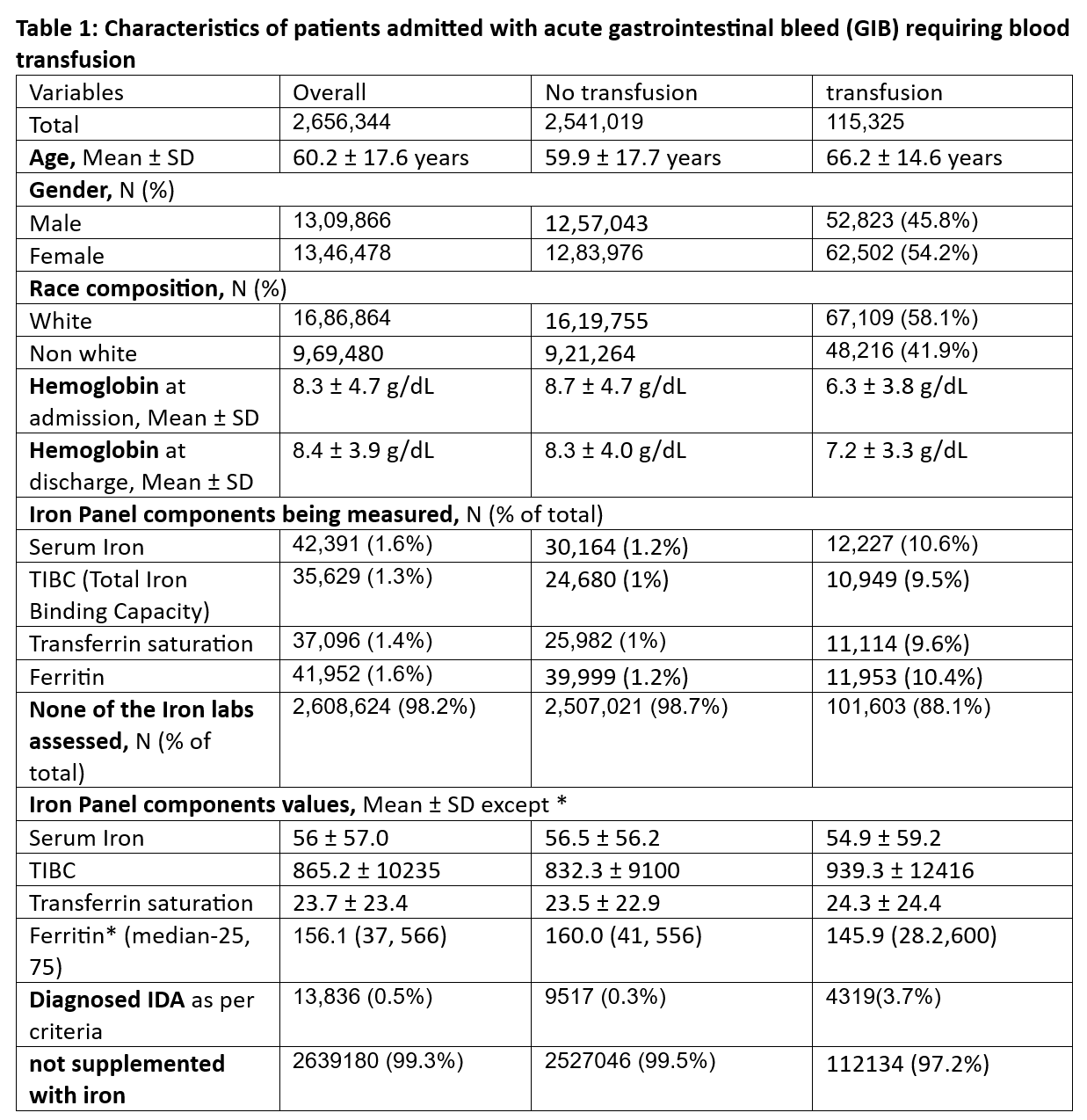
Figure: Characteristics of patients admitted with acute gastrointestinal bleed (GIB)
Disclosures:
Akshay Sharma indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Muhammad Kazi indicated no relevant financial relationships.
Mitchell Karpman indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Sanmeet Singh indicated no relevant financial relationships.
Nargiz Muganlinskaya indicated no relevant financial relationships.
Akshay Sharma, MBBS1, Nirav Agrawal, MD, MPH2, Muhammad Kazi, MD1, Mitchell Karpman, PhD1, Rahul Kumar, MD3, Sanmeet Singh, MD1, Nargiz Muganlinskaya, MD, MBA1. P5223 - Treating More Than the Bleed: Exploring Iron Status and Use of Supplementation in Acute Gastrointestinal Bleed - A Retrospective Cohort Study Using the Trinet-x Databases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Luminis Health Anne Arundel Medical Center, Annapolis, MD; 2Anne Arundel Medical Center, Luminus Health, Annapolis, MD; 3North Central Bronx Hospital, Bronx, NY
Introduction: While the primary focus in managing gastrointestinal bleeding (GIB) is controlling the bleed source, addressing iron deficiency anemia (IDA) is equally critical. Without initiating iron supplementation during hospitalization, up to 70% of acute GIB patients may experience persistent IDA at three months, leading to significant comorbidities and an annual economic burden of up to $29,511 per patient. Although, American College of Gastroenterology guidelines recommend a restrictive blood transfusion strategy for acute GIB [maintaining hemoglobin (Hb) >7 g/dL] and emphasizes iron supplementation for chronic GIB, however, no clear guidelines exist on iron assessment and deficiency management in setting of acute GIB. This study examines the gap by analyzing data from Trinet-X database to evaluate iron status assessment and supplementation initiation practices during acute GIB hospitalization.
Methods: This 5-year retrospective cohort study utilized TriNetX data (2020–2024) and included adults aged ≥18 hospitalized due to acute GIB and divided into 2 cohorts: requiring red blood cell (RBC) or whole blood transfusion. Table 1 details. We performed descriptive analysis using SQL and excel.
Results: 2,656,344 patients (45.1% female) were hospitalized with acute GIB, of which 115,325 (4.3%)patients required PRBC transfusion. Patients who received transfusions were older (mean age 66.2 vs. 59.9 years) and more likely to be female (54.2% vs. 50.5%) and non-white (41.9% vs. 36.2%) compared to those who did not require transfusion. Admission hemoglobin levels were significantly lower in the transfusion group (6.3 ± 3.8 g/dL) compared to the non-transfusion group (8.7 ± 4.7 g/dL), and discharge hemoglobin remained lower (7.2 ± 3.3 g/dL vs. 8.3 ± 4.0 g/dL). The mean pre-transfusion hemoglobin level was 7.7 g/dL. Despite severe anemia majority of patients (88.1%) in the transfused cohort had no iron panel assessment, and only 3.7% were formally diagnosed with iron deficiency anemia (IDA). Furthermore, 97.2% of transfused patients did not receive iron supplementation, highlighting a large treatment gap
Discussion: In this large cohort of patients admitted with acute GIB, blood transfusion recipients were typically older and more likely to have anemia on admission and discharge. Despite evidence of iron deficiency and a high likelihood of IDA, iron panel testing was underutilized, and iron supplementation was rarely administered
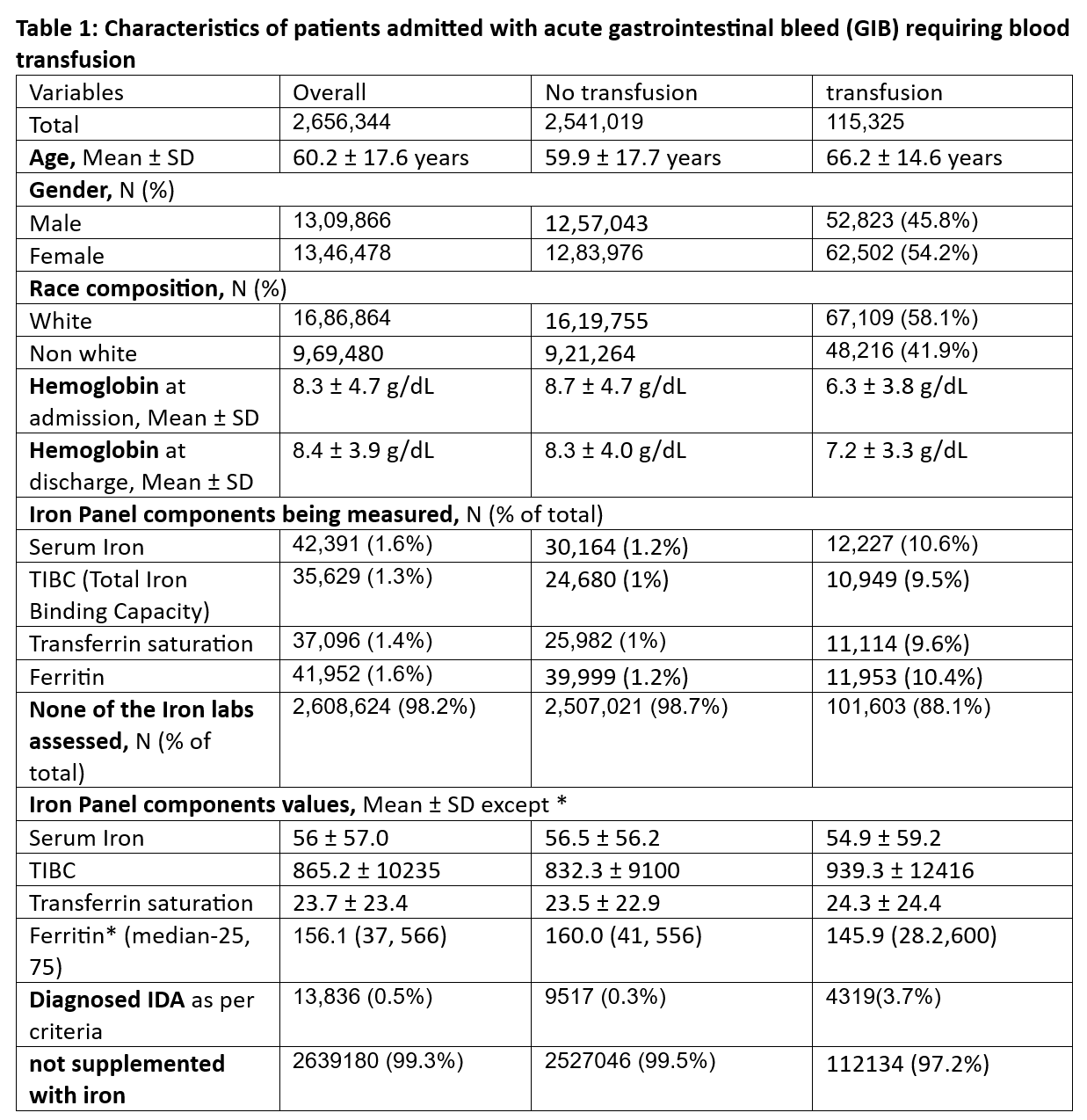
Figure: Characteristics of patients admitted with acute gastrointestinal bleed (GIB)
Disclosures:
Akshay Sharma indicated no relevant financial relationships.
Nirav Agrawal indicated no relevant financial relationships.
Muhammad Kazi indicated no relevant financial relationships.
Mitchell Karpman indicated no relevant financial relationships.
Rahul Kumar indicated no relevant financial relationships.
Sanmeet Singh indicated no relevant financial relationships.
Nargiz Muganlinskaya indicated no relevant financial relationships.
Akshay Sharma, MBBS1, Nirav Agrawal, MD, MPH2, Muhammad Kazi, MD1, Mitchell Karpman, PhD1, Rahul Kumar, MD3, Sanmeet Singh, MD1, Nargiz Muganlinskaya, MD, MBA1. P5223 - Treating More Than the Bleed: Exploring Iron Status and Use of Supplementation in Acute Gastrointestinal Bleed - A Retrospective Cohort Study Using the Trinet-x Databases, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
