Tuesday Poster Session
Category: GI Bleeding
P5222 - Impact of Direct Oral Anticoagulants (DOACs) vs Warfarin on Outcomes in Acute GI Bleeding
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Maurice Facey, MD
University Hospitals Cleveland Medical Center
Cleveland, OH
Presenting Author(s)
Maurice Facey, MD1, Onoja-Frederick Okwori, MD, MPH2, Sedina Asafu-Adjaye, MD1, Nawaf Alhazmi, MD2, Gregory S. Cooper, MD3, Omar Sims, PhD4, Andrew Catanzaro, MD3, Jaime A. Perez, PhD2, Elleson Harper, BS2
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL
Introduction: Direct-acting oral anticoagulants and Warfarin are being increasingly utilized for anticoagulation but, studies are mixed regarding the comparative risk for gastrointestinal bleeding(GIB) associated with these therapies.1 Some studies suggest that GIBs are lower in patients on DOACs but, there are contradictory studies as well.2 The objective of this study was to evaluate the risk of GIB in patients with atrial fibrillation on DOACs compared to Warfarin and also overall mortality.
Methods: This study was developed using a large de-identified health research network with data from 98 health care organizations (HCO), within the United States (TriNetX). This study consisted of 2 cohorts. The first cohort being on Warfarin and second cohort being on DOACs (Dabigatran, Rivaroxaban, Apixaban, and Edoxaban). Patients were excluded if they had been on the opposite therapy prior, had any other indication for anticoagulation other than atrial fibrillation and were excluded if they were on DVT prophylaxis while hospitalized such as LMWH (Low Molecular Weight Heparin) or unfractionated heparin. This study then consisted of five queries comparing the cohort’s rates of overall GI bleed, bleeding due to anticoagulation, UGIB( Upper GI bleed), LGIB (Lower GI Bleed), and overall mortality. Within each cohort, we collected data on demographics and several risk factors for GIB, including genetic disorders, renal disease, and acquired bleeding disorders. Then performed propensity score matching (PSM) to control for confounding (Table 1).
Results: This study identified 853 patients in the Warfarin group and 3,855 patients in the DOAC group before matching. After matching, there were 826 patients in both cohorts. Our study found that the risk of GI bleeding was higher in the Warfarin group(n=254) vs DOAC group (n=176) (OR 1.64, CI 1.31-2.05, p= 0.00). There was no difference in rates of Upper GI Bleed (OR 0.82, CI 0.41-1.64, p=0.57) and Lower GI Bleed (OR 1.08, CI 0.71-1.65, p=0.71) between the two cohorts. Overall, mortality was also increased in the Warfarin group (n=183) vs DOAC group (n=73) (OR 2.94, CI 2.19-3.93, p=0.00).
Discussion: This retrospective study concluded that patients on Warfarin have a statistically significant increased risk of GI bleeding and mortality as compared to those on DOACs. Future prospective studies are needed to further assess the clinical safety of both therapies in high-risk groups for GI bleeds.
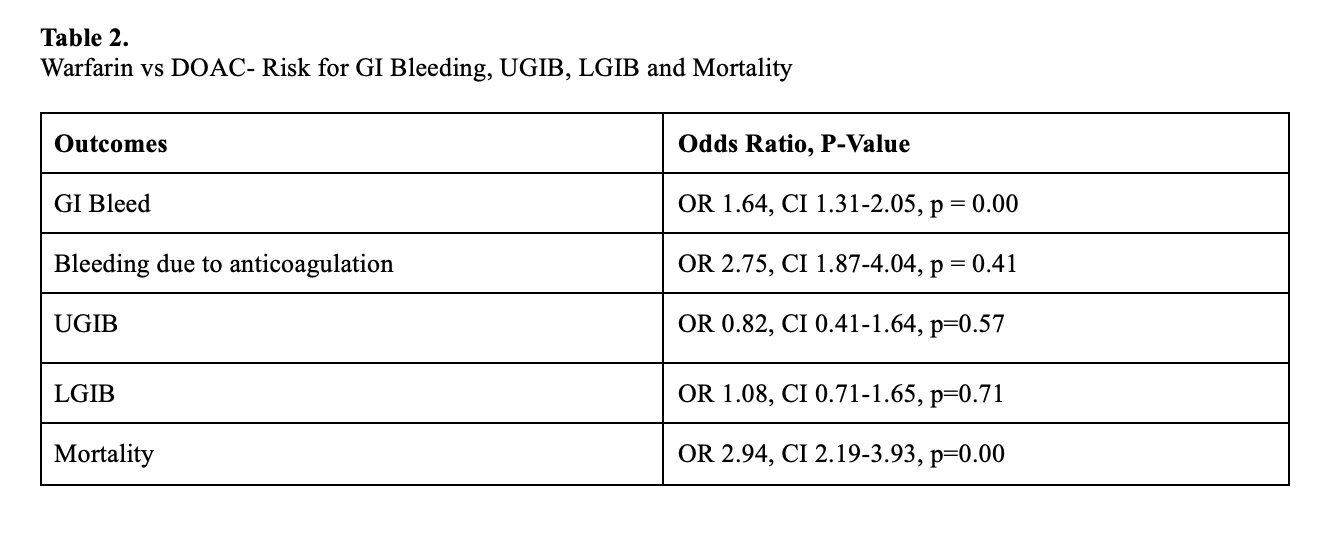
Figure: Baseline Characteristics of Patients with Acute GI bleeding on DOACs vs Warfarin before and after propensity score matching
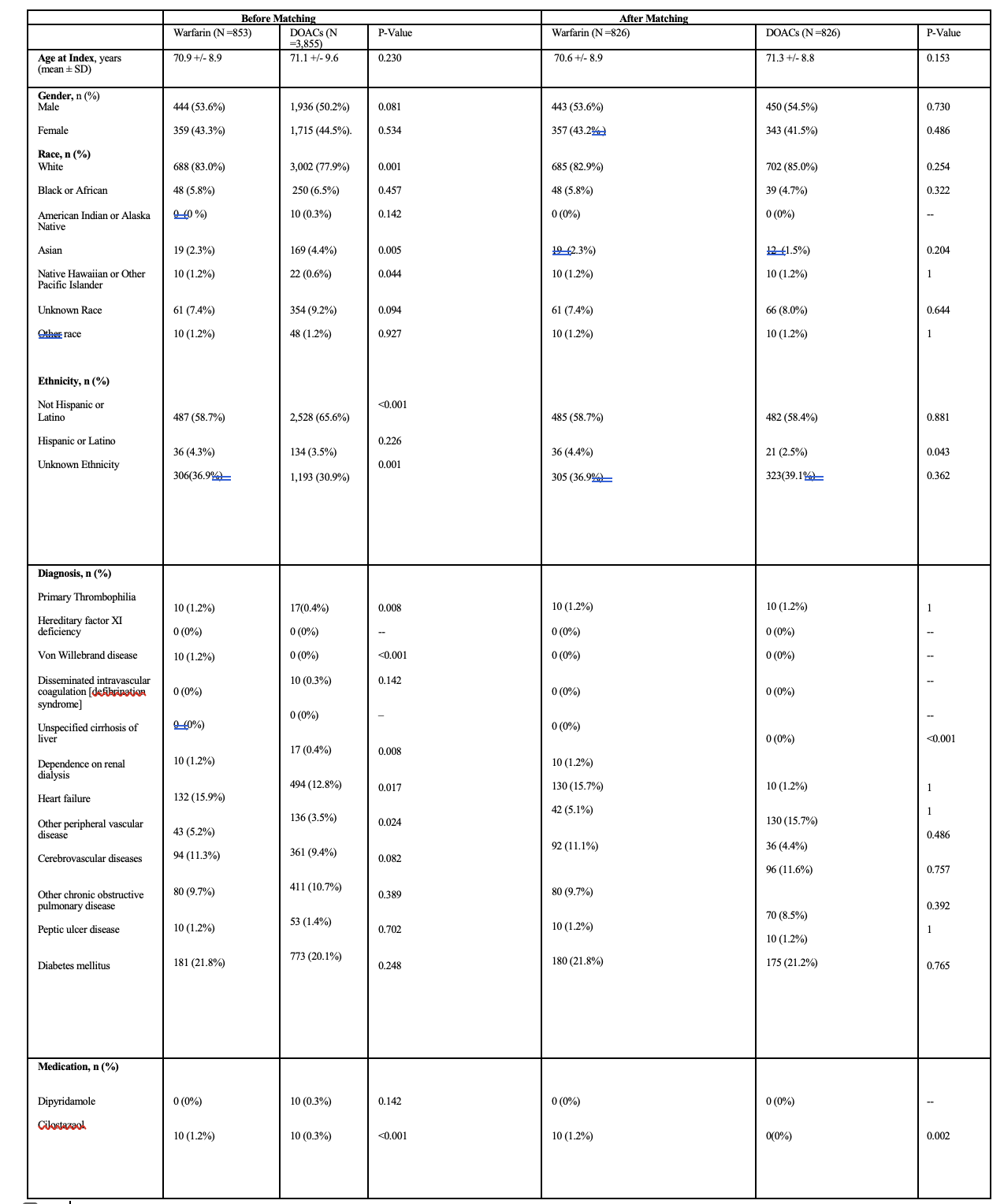
Figure: Warfarin vs DOAC- Risk for GI Bleeding, Bleeding due to anticoagulation,UGIB, LGIB and Mortality
Disclosures:
Maurice Facey indicated no relevant financial relationships.
Onoja-Frederick Okwori indicated no relevant financial relationships.
Sedina Asafu-Adjaye indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Maurice Facey, MD1, Onoja-Frederick Okwori, MD, MPH2, Sedina Asafu-Adjaye, MD1, Nawaf Alhazmi, MD2, Gregory S. Cooper, MD3, Omar Sims, PhD4, Andrew Catanzaro, MD3, Jaime A. Perez, PhD2, Elleson Harper, BS2. P5222 - Impact of Direct Oral Anticoagulants (DOACs) vs Warfarin on Outcomes in Acute GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals Cleveland Medical Center, Cleveland, OH; 2University Hospitals Cleveland Medical Center, Case Western Reserve University, Cleveland, OH; 3Digestive Health Institute, University Hospitals Cleveland Medical Center, Cleveland, OH; 4Cleveland Clinic Foundation, Hoover, AL
Introduction: Direct-acting oral anticoagulants and Warfarin are being increasingly utilized for anticoagulation but, studies are mixed regarding the comparative risk for gastrointestinal bleeding(GIB) associated with these therapies.1 Some studies suggest that GIBs are lower in patients on DOACs but, there are contradictory studies as well.2 The objective of this study was to evaluate the risk of GIB in patients with atrial fibrillation on DOACs compared to Warfarin and also overall mortality.
Methods: This study was developed using a large de-identified health research network with data from 98 health care organizations (HCO), within the United States (TriNetX). This study consisted of 2 cohorts. The first cohort being on Warfarin and second cohort being on DOACs (Dabigatran, Rivaroxaban, Apixaban, and Edoxaban). Patients were excluded if they had been on the opposite therapy prior, had any other indication for anticoagulation other than atrial fibrillation and were excluded if they were on DVT prophylaxis while hospitalized such as LMWH (Low Molecular Weight Heparin) or unfractionated heparin. This study then consisted of five queries comparing the cohort’s rates of overall GI bleed, bleeding due to anticoagulation, UGIB( Upper GI bleed), LGIB (Lower GI Bleed), and overall mortality. Within each cohort, we collected data on demographics and several risk factors for GIB, including genetic disorders, renal disease, and acquired bleeding disorders. Then performed propensity score matching (PSM) to control for confounding (Table 1).
Results: This study identified 853 patients in the Warfarin group and 3,855 patients in the DOAC group before matching. After matching, there were 826 patients in both cohorts. Our study found that the risk of GI bleeding was higher in the Warfarin group(n=254) vs DOAC group (n=176) (OR 1.64, CI 1.31-2.05, p= 0.00). There was no difference in rates of Upper GI Bleed (OR 0.82, CI 0.41-1.64, p=0.57) and Lower GI Bleed (OR 1.08, CI 0.71-1.65, p=0.71) between the two cohorts. Overall, mortality was also increased in the Warfarin group (n=183) vs DOAC group (n=73) (OR 2.94, CI 2.19-3.93, p=0.00).
Discussion: This retrospective study concluded that patients on Warfarin have a statistically significant increased risk of GI bleeding and mortality as compared to those on DOACs. Future prospective studies are needed to further assess the clinical safety of both therapies in high-risk groups for GI bleeds.
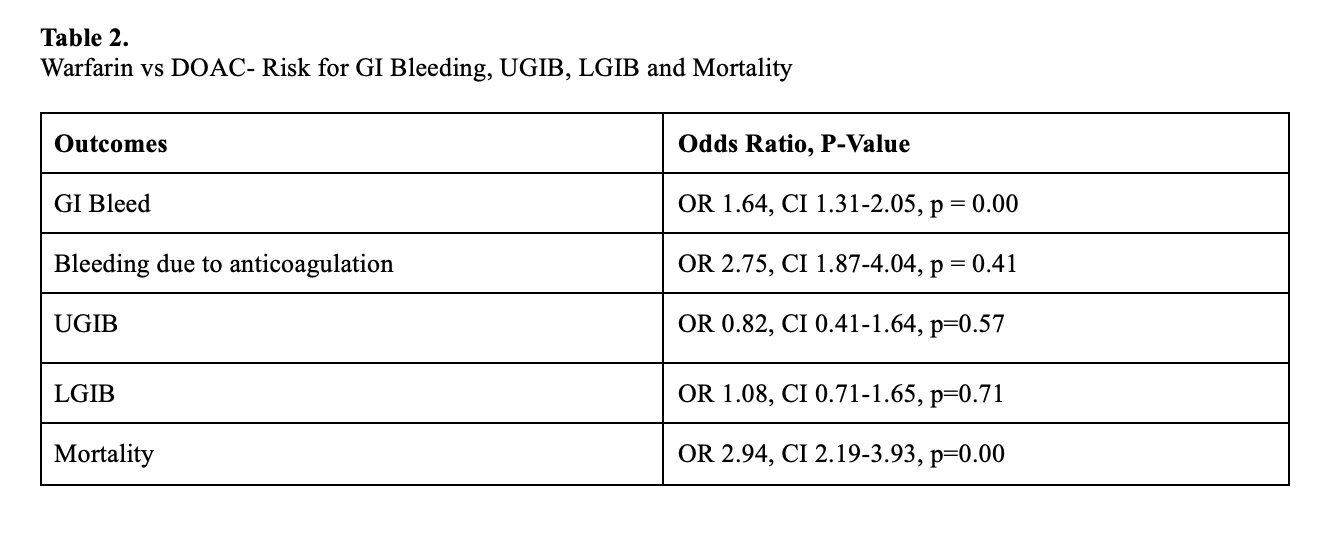
Figure: Baseline Characteristics of Patients with Acute GI bleeding on DOACs vs Warfarin before and after propensity score matching
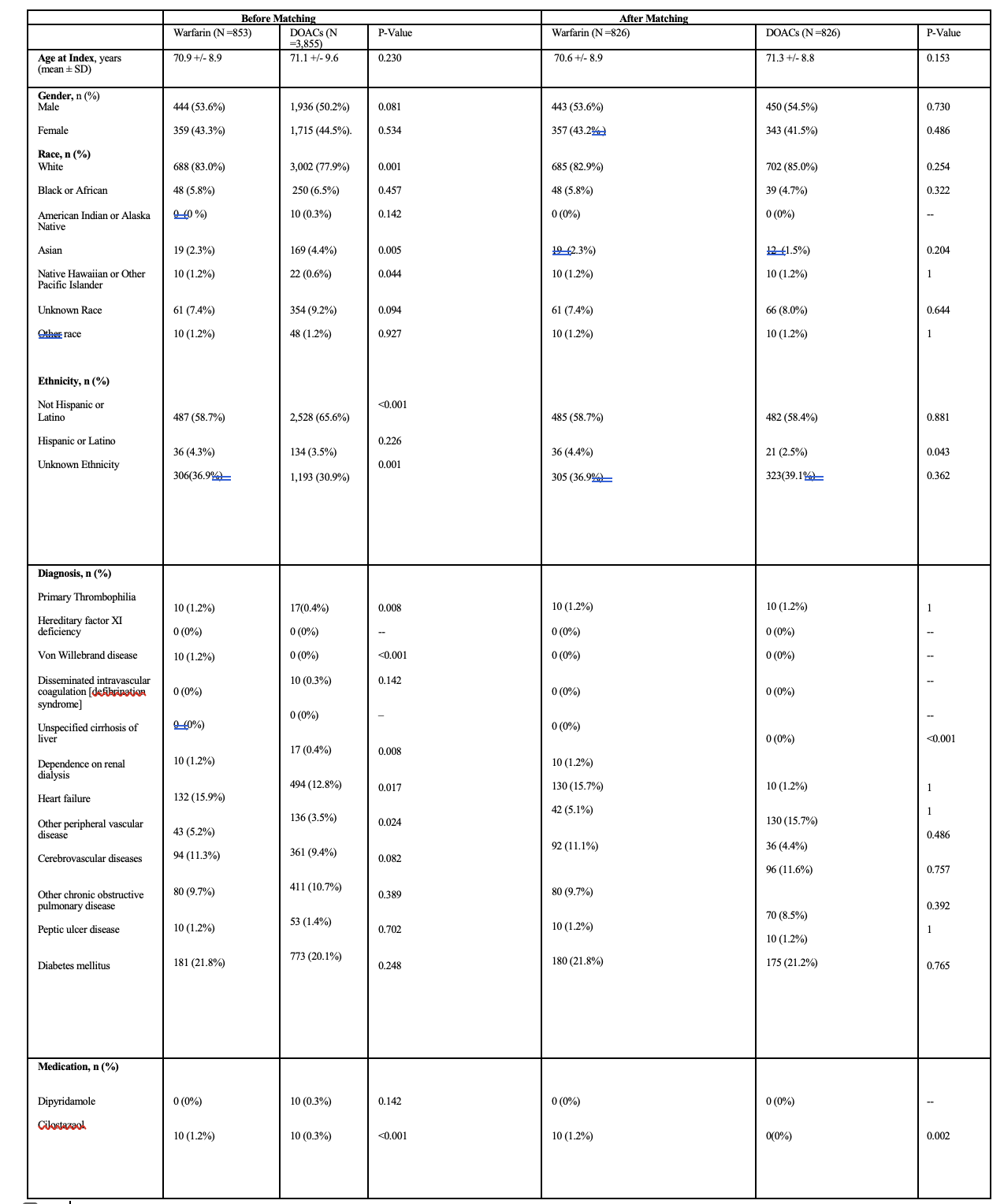
Figure: Warfarin vs DOAC- Risk for GI Bleeding, Bleeding due to anticoagulation,UGIB, LGIB and Mortality
Disclosures:
Maurice Facey indicated no relevant financial relationships.
Onoja-Frederick Okwori indicated no relevant financial relationships.
Sedina Asafu-Adjaye indicated no relevant financial relationships.
Nawaf Alhazmi indicated no relevant financial relationships.
Gregory Cooper indicated no relevant financial relationships.
Omar Sims indicated no relevant financial relationships.
Andrew Catanzaro indicated no relevant financial relationships.
Jaime Perez indicated no relevant financial relationships.
Elleson Harper indicated no relevant financial relationships.
Maurice Facey, MD1, Onoja-Frederick Okwori, MD, MPH2, Sedina Asafu-Adjaye, MD1, Nawaf Alhazmi, MD2, Gregory S. Cooper, MD3, Omar Sims, PhD4, Andrew Catanzaro, MD3, Jaime A. Perez, PhD2, Elleson Harper, BS2. P5222 - Impact of Direct Oral Anticoagulants (DOACs) vs Warfarin on Outcomes in Acute GI Bleeding, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
