Tuesday Poster Session
Category: GI Bleeding
P5213 - Efficacy and Safety of Tranexamic Acid in Acute Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Khadija Mohib, MD (she/her/hers)
Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas
Las Vegas, NV
Presenting Author(s)
Khadija Mohib, MD1, Abu-Bakr Ahmed, BA1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Mian Uman Anwer, MBBS6, Prasun K.. Jalal, MD7
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Quetta Institute of Medical Sciences, Quetta, Balochistan, Pakistan; 5University of Texas Southwestern Medical Center, Dallas, TX; 6Punjab Medical College, Faisalabad, Punjab, Pakistan; 7Baylor College of Medicine, Houston, TX
Introduction: Acute gastrointestinal bleeding (AGIB) is a significant cause of emergency admissions associated with high morbidity and mortality. Tranexamic acid (TXA), an antifibrinolytic agent, has been proposed for controlling AGIB but concerns remain regarding its safety and effectiveness. This meta-analysis aimed to assess the safety and efficacy of TXA in AGIB.
Methods: Electronic databases like PubMed, Cochrane Library, and ScienceDirect were searched from inception till January 2025. This review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The Risk Ratios (RR) and Mean Differences (MD) along with 95% Confidence intervals (CI) were pooled under the random effects model using Review Manager version 5.4.1 for the dichotomous and continuous outcomes. The quality was assessed by the Cochrane RoB 2.0 tool and the Newcastle Ottawa Scale. Publication bias was assessed by the funnel plots and Egger’s regression test.
Results: Eighteen studies pooling a total of 15,014 patients were included in this meta-analysis. Mortality was significantly reduced in the TXA group with a pooled RR of 0.83 (95%CI:[0.73,0.95]; p=0.008; I2=0%). Rebleeding risk was also significantly decreased in the TXA arm (RR= 0.75; 95%CI:[0.62,0.92]; p=0.005; I2=41%). The transfusion requirement (RR= 0.99; 95%CI:[0.93,1.06]; p=0.74; I2=37%) and the need for overall interventions (RR= 0.87; 95%CI:[0.69,1.10]; p=0.25; I2=38%) showed no significant difference between the two arms . Other outcomes including the need for therapeutic endoscopic intervention (RR= 0.86; 95%CI:[0.62,1.21]; p=0.39; I2=50%), need for surgical intervention (RR= 0.76; 95%CI:[0.54,1.07]; p=0.11; I2=47%), venous thromboembolic events (RR= 1.29; 95%CI:[0.53,3.16]; p=0.58; I2=39%), arterial thromboembolic events (RR= 0.95; 95%CI:[0.64,1.42]; p=0.82; I2=0%), transfusion volume (MD= -0.64; 95%CI:[-1.37,0.08]; p=0.08; I2=77%), and length of hospital stay (MD= -0.17; 95%CI:[-0.48,0.14]; p=0.28; I2=42%) were comparable between the two groups.
Discussion: Tranexamic acid significantly reduces mortality and rebleeding in AGIB, but shows no significant differences in transfusion requirements, interventions, or thromboembolic risks, indicating potential benefits with comparable safety.
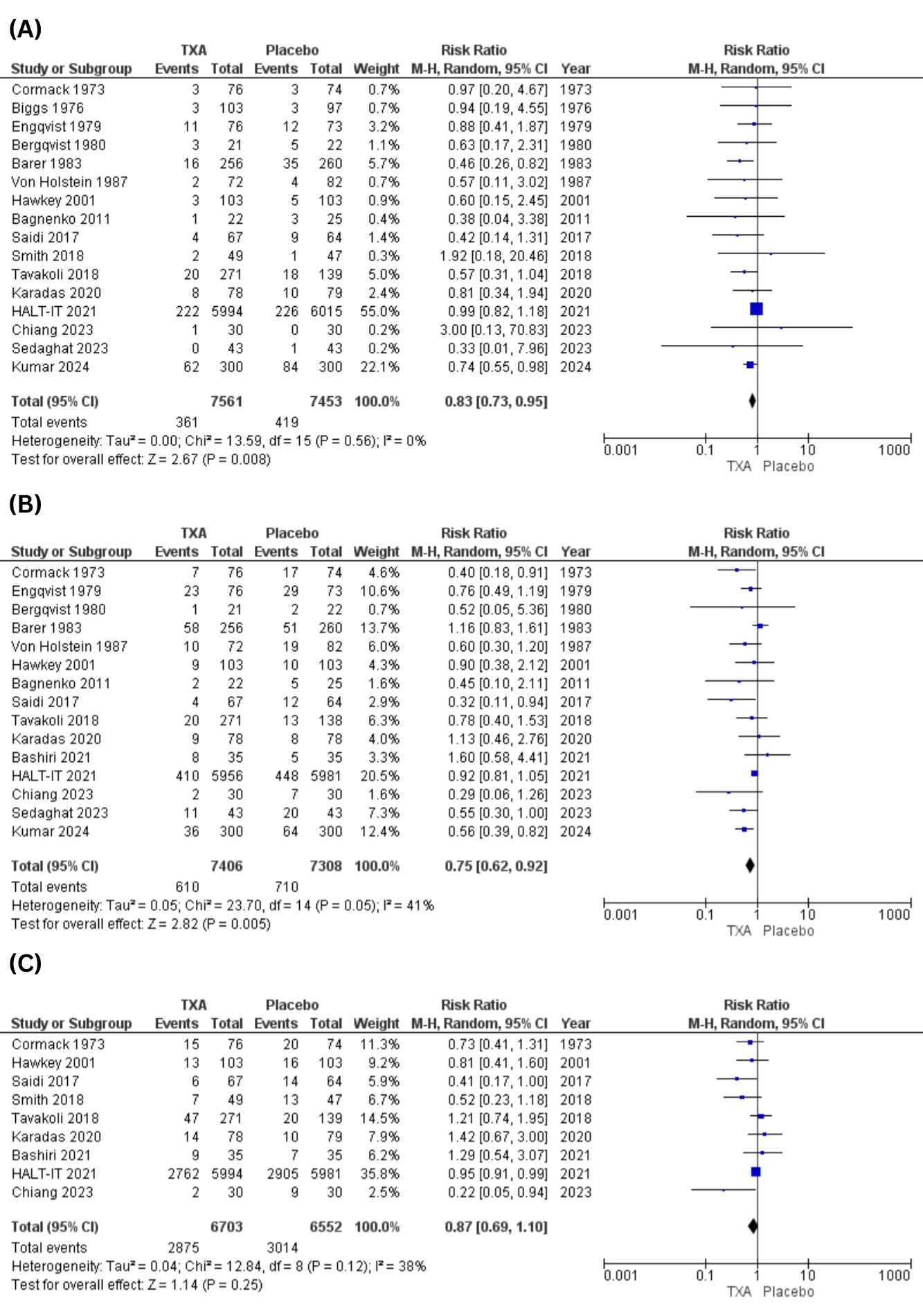
Figure: Figure 1: Forest Plots for (A)Mortality (B)Rebleeding (C)Need for Intervention
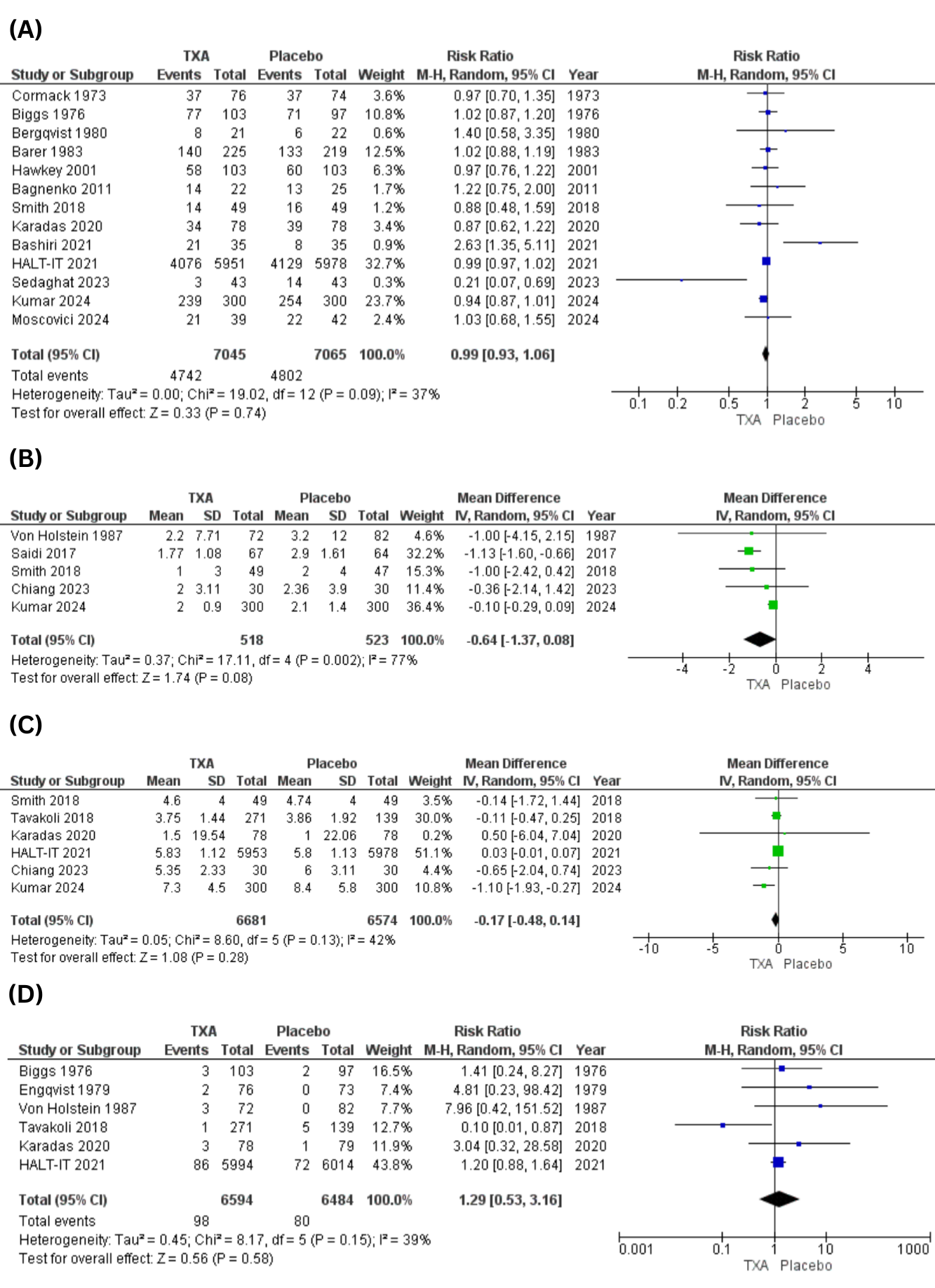
Figure: Figure 2: Forest Plots for (A)Transfusion Requirement (B)Transfusion Volume (C)Length of Hospital Stay (D) Venous Thromboembolic Events
Disclosures:
Khadija Mohib indicated no relevant financial relationships.
Abu-Bakr Ahmed indicated no relevant financial relationships.
Zain Ul Abideen indicated no relevant financial relationships.
Muhammad Hassan Waseem indicated no relevant financial relationships.
Sania Aimen indicated no relevant financial relationships.
Noor Ul Huda Ramzan indicated no relevant financial relationships.
Mian Uman Anwer indicated no relevant financial relationships.
Prasun Jalal: AbbVie – Consultant. Gilead Sciences – Consultant.
Khadija Mohib, MD1, Abu-Bakr Ahmed, BA1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Mian Uman Anwer, MBBS6, Prasun K.. Jalal, MD7. P5213 - Efficacy and Safety of Tranexamic Acid in Acute Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Kirk Kerkorian School of Medicine at the University of Nevada Las Vegas, Las Vegas, NV; 2King Edward Medical University, Lahore, Punjab, Pakistan; 3Allama Iqbal Medical College, Lahore, Punjab, Pakistan; 4Quetta Institute of Medical Sciences, Quetta, Balochistan, Pakistan; 5University of Texas Southwestern Medical Center, Dallas, TX; 6Punjab Medical College, Faisalabad, Punjab, Pakistan; 7Baylor College of Medicine, Houston, TX
Introduction: Acute gastrointestinal bleeding (AGIB) is a significant cause of emergency admissions associated with high morbidity and mortality. Tranexamic acid (TXA), an antifibrinolytic agent, has been proposed for controlling AGIB but concerns remain regarding its safety and effectiveness. This meta-analysis aimed to assess the safety and efficacy of TXA in AGIB.
Methods: Electronic databases like PubMed, Cochrane Library, and ScienceDirect were searched from inception till January 2025. This review followed the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines. The Risk Ratios (RR) and Mean Differences (MD) along with 95% Confidence intervals (CI) were pooled under the random effects model using Review Manager version 5.4.1 for the dichotomous and continuous outcomes. The quality was assessed by the Cochrane RoB 2.0 tool and the Newcastle Ottawa Scale. Publication bias was assessed by the funnel plots and Egger’s regression test.
Results: Eighteen studies pooling a total of 15,014 patients were included in this meta-analysis. Mortality was significantly reduced in the TXA group with a pooled RR of 0.83 (95%CI:[0.73,0.95]; p=0.008; I2=0%). Rebleeding risk was also significantly decreased in the TXA arm (RR= 0.75; 95%CI:[0.62,0.92]; p=0.005; I2=41%). The transfusion requirement (RR= 0.99; 95%CI:[0.93,1.06]; p=0.74; I2=37%) and the need for overall interventions (RR= 0.87; 95%CI:[0.69,1.10]; p=0.25; I2=38%) showed no significant difference between the two arms . Other outcomes including the need for therapeutic endoscopic intervention (RR= 0.86; 95%CI:[0.62,1.21]; p=0.39; I2=50%), need for surgical intervention (RR= 0.76; 95%CI:[0.54,1.07]; p=0.11; I2=47%), venous thromboembolic events (RR= 1.29; 95%CI:[0.53,3.16]; p=0.58; I2=39%), arterial thromboembolic events (RR= 0.95; 95%CI:[0.64,1.42]; p=0.82; I2=0%), transfusion volume (MD= -0.64; 95%CI:[-1.37,0.08]; p=0.08; I2=77%), and length of hospital stay (MD= -0.17; 95%CI:[-0.48,0.14]; p=0.28; I2=42%) were comparable between the two groups.
Discussion: Tranexamic acid significantly reduces mortality and rebleeding in AGIB, but shows no significant differences in transfusion requirements, interventions, or thromboembolic risks, indicating potential benefits with comparable safety.
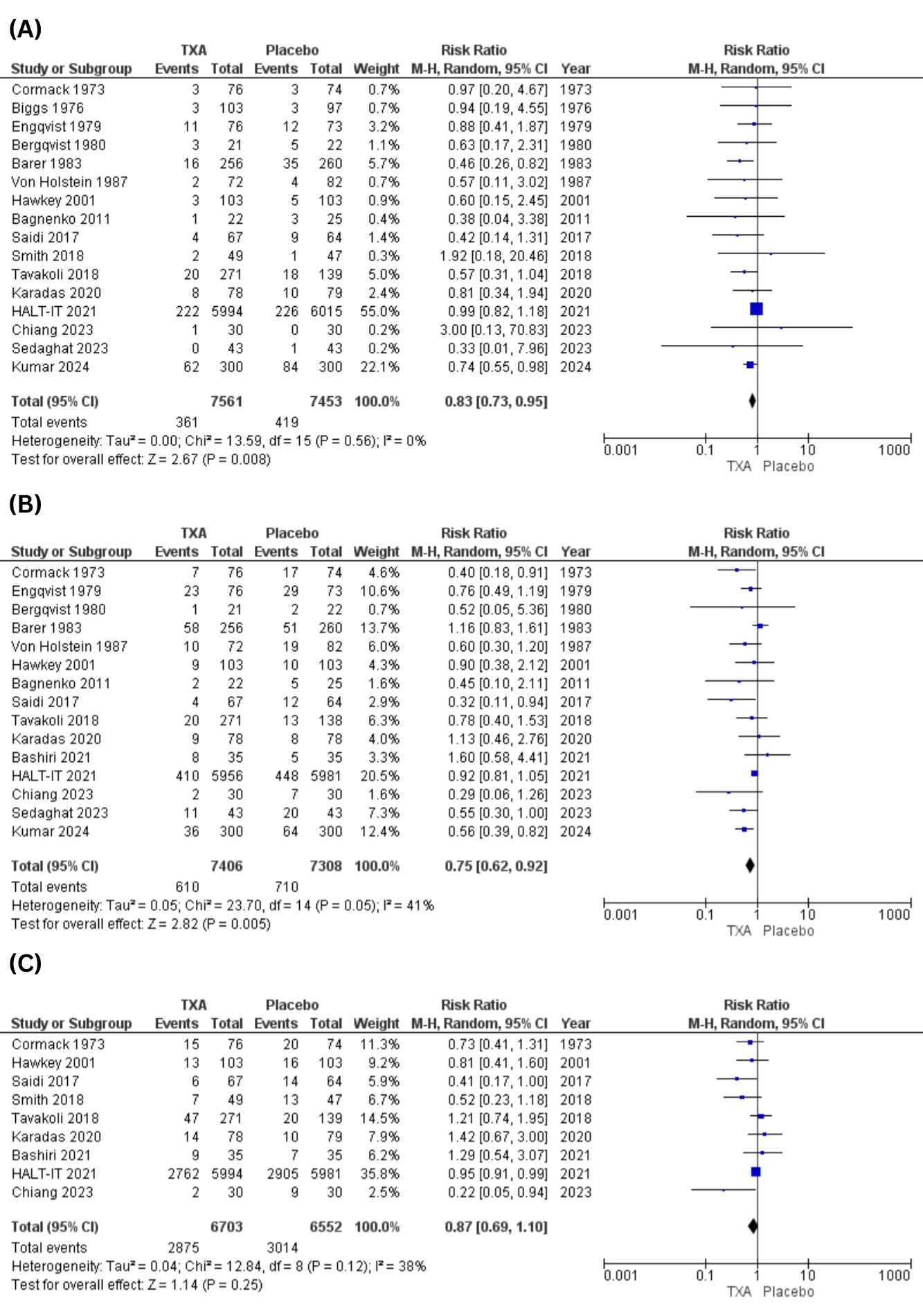
Figure: Figure 1: Forest Plots for (A)Mortality (B)Rebleeding (C)Need for Intervention
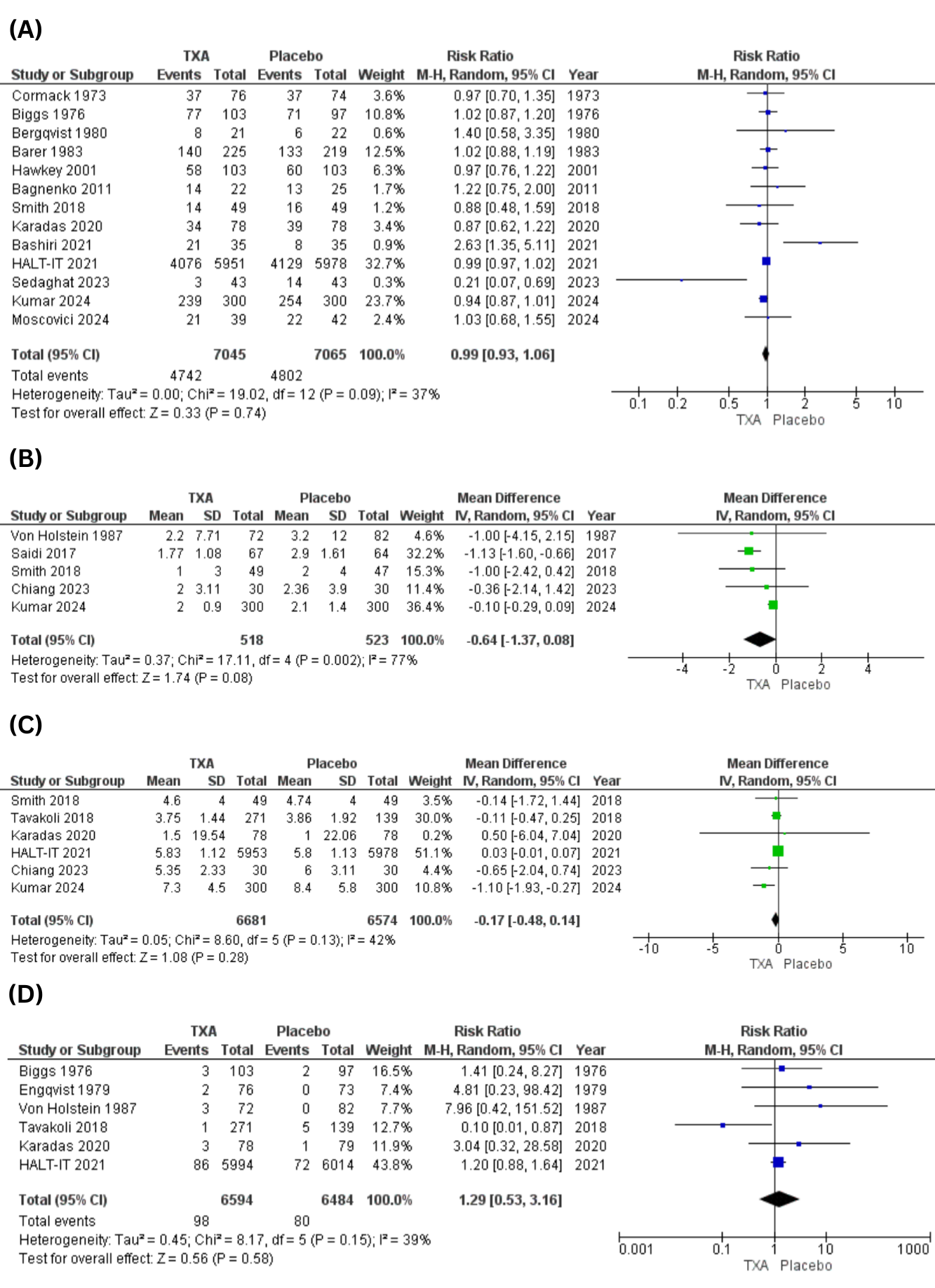
Figure: Figure 2: Forest Plots for (A)Transfusion Requirement (B)Transfusion Volume (C)Length of Hospital Stay (D) Venous Thromboembolic Events
Disclosures:
Khadija Mohib indicated no relevant financial relationships.
Abu-Bakr Ahmed indicated no relevant financial relationships.
Zain Ul Abideen indicated no relevant financial relationships.
Muhammad Hassan Waseem indicated no relevant financial relationships.
Sania Aimen indicated no relevant financial relationships.
Noor Ul Huda Ramzan indicated no relevant financial relationships.
Mian Uman Anwer indicated no relevant financial relationships.
Prasun Jalal: AbbVie – Consultant. Gilead Sciences – Consultant.
Khadija Mohib, MD1, Abu-Bakr Ahmed, BA1, Zain Ul Abideen, MBBS2, Muhammad Hassan Waseem, MBBS3, Sania Aimen, MBBS4, Noor Ul Huda Ramzan, MD5, Mian Uman Anwer, MBBS6, Prasun K.. Jalal, MD7. P5213 - Efficacy and Safety of Tranexamic Acid in Acute Gastrointestinal Bleeding: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
