Tuesday Poster Session
Category: GI Bleeding
P5212 - Patients With a Gastrointestinal Bleed During Hospitalization Have Higher 90-Day Mortality Than Those With GI Bleeding on Hospital Presentation
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MS
Miyabi Saito, MD
Massachusetts General Hospital, Harvard Medical School
Boston, MA
Presenting Author(s)
Miyabi Saito, MD1, Margaret Koester, MD, MPH2, James M. Richter, MD, MA3, Sonali Palchaudhuri, MD, MHCI2
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Mass General Brigham, Boston, MA
Introduction: Gastrointestinal bleeds (GIBs) have a high mortality rate, with reports ranging from 5-24%. Prior studies have shown that upper GIBs that occur during hospitalization are associated with high mortality, though there is limited data in lower GIBs and with development of new management strategies. We sought to evaluate mortality rates of GIBs that occur while inpatient (IP) versus when it is the admitting diagnosis on hospital presentation (bleed while outpatient, OP) for both upper and lower sources.
Methods: We performed a retrospective review of adult patients admitted to a tertiary hospital between 1/2023-12/2023 who had an inpatient diagnosis of GIB and a GI subspecialty consultation. Cases were classified as IP vs OP. Our primary outcome was 90-day all-cause mortality.
Results: Of 755 cases reviewed, 71% (533/755) were OP GIB and 29% (222/755) were IP. A higher proportion of IP GIB received pressor support and underwent endoscopy [Table 1]. OP cases had a higher proportion of bleeds due to malignant and diverticular sources. All-cause 90-day mortality was 31% (69/222) IP compared to 11% (57/533) OP with an OR of 3.77 (p< 0.01). 20% (25/126) of patients died in the setting of GIB after transitioning to comfort care due to comorbidities. The remainder of deaths were outside acute GIB settings [Figure 1]. Similar differences in mortality between IP and OP were seen in both upper (35% IP vs 11% OP, OR 4.4, p< 0.01) and lower GIB (27% IP vs 8% OP, OR 3.8, p< 0.01). Endoscopic or radiologic intervention to address the GIB was not associated with reduced mortality in either group (OR 1.34, p=0.35 for OP; OR 0.67, p=0.17 for IP). Other risk factors associated with higher mortality included having an overt bleed (OR 4.33, p= 0.045) and being on chronic anticoagulation (OR 1.76, p < 0.01).
Discussion: 90-day mortality for patients admitted to a tertiary hospital in 2023 who developed a GIB while inpatient is significantly high for both upper and lower sources (35% and 27%). This likely reflects the increased vulnerability and illness severity of the patient population who develop acute GIBs during admission, irrespective of GIB management. Nonetheless, this finding may guide clinicians in prognostication and mortality risk stratification for their patients. Future work involves adjusting for independent risk factors, which can aid in more detailed prognostication.
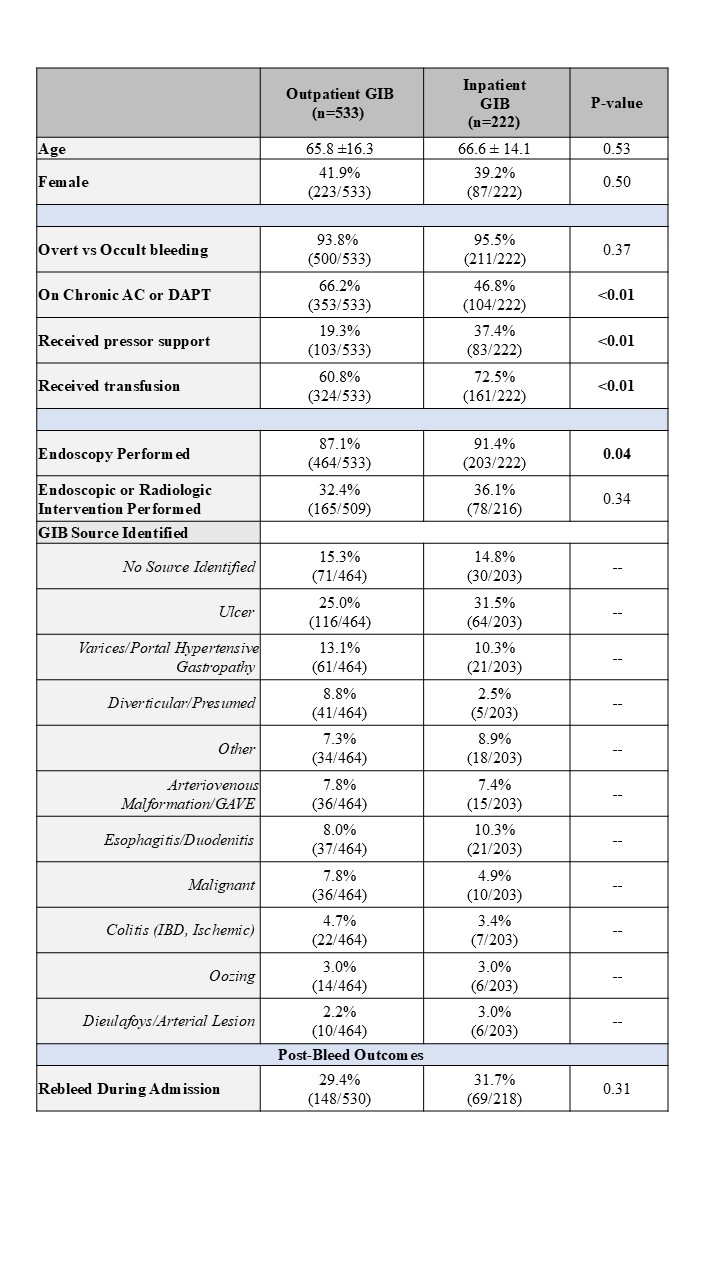
Figure: Table 1. Comparison of patients and bleed characteristics between those who presented with a GIB (outpatient GIB) and those who developed GIB during admission (inpatient GIB). Significance was determined using Chi-squared test. AC: anticoagulation. DAPT: dual antiplatelet therapy. GAVE: gastric antral vascular ectasia. IBD: inflammatory bowel disease.

Figure: Figure 1. Kaplan Meier Survival Curve over 90 days post GIB comparing patients who had GIB on hospital presentation (OP) versus developed GIB during admission (IP) (p < 0.01)
Disclosures:
Miyabi Saito indicated no relevant financial relationships.
Margaret Koester indicated no relevant financial relationships.
James M. Richter indicated no relevant financial relationships.
Sonali Palchaudhuri indicated no relevant financial relationships.
Miyabi Saito, MD1, Margaret Koester, MD, MPH2, James M. Richter, MD, MA3, Sonali Palchaudhuri, MD, MHCI2. P5212 - Patients With a Gastrointestinal Bleed During Hospitalization Have Higher 90-Day Mortality Than Those With GI Bleeding on Hospital Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Massachusetts General Hospital, Harvard Medical School, Boston, MA; 2Massachusetts General Hospital, Boston, MA; 3Mass General Brigham, Boston, MA
Introduction: Gastrointestinal bleeds (GIBs) have a high mortality rate, with reports ranging from 5-24%. Prior studies have shown that upper GIBs that occur during hospitalization are associated with high mortality, though there is limited data in lower GIBs and with development of new management strategies. We sought to evaluate mortality rates of GIBs that occur while inpatient (IP) versus when it is the admitting diagnosis on hospital presentation (bleed while outpatient, OP) for both upper and lower sources.
Methods: We performed a retrospective review of adult patients admitted to a tertiary hospital between 1/2023-12/2023 who had an inpatient diagnosis of GIB and a GI subspecialty consultation. Cases were classified as IP vs OP. Our primary outcome was 90-day all-cause mortality.
Results: Of 755 cases reviewed, 71% (533/755) were OP GIB and 29% (222/755) were IP. A higher proportion of IP GIB received pressor support and underwent endoscopy [Table 1]. OP cases had a higher proportion of bleeds due to malignant and diverticular sources. All-cause 90-day mortality was 31% (69/222) IP compared to 11% (57/533) OP with an OR of 3.77 (p< 0.01). 20% (25/126) of patients died in the setting of GIB after transitioning to comfort care due to comorbidities. The remainder of deaths were outside acute GIB settings [Figure 1]. Similar differences in mortality between IP and OP were seen in both upper (35% IP vs 11% OP, OR 4.4, p< 0.01) and lower GIB (27% IP vs 8% OP, OR 3.8, p< 0.01). Endoscopic or radiologic intervention to address the GIB was not associated with reduced mortality in either group (OR 1.34, p=0.35 for OP; OR 0.67, p=0.17 for IP). Other risk factors associated with higher mortality included having an overt bleed (OR 4.33, p= 0.045) and being on chronic anticoagulation (OR 1.76, p < 0.01).
Discussion: 90-day mortality for patients admitted to a tertiary hospital in 2023 who developed a GIB while inpatient is significantly high for both upper and lower sources (35% and 27%). This likely reflects the increased vulnerability and illness severity of the patient population who develop acute GIBs during admission, irrespective of GIB management. Nonetheless, this finding may guide clinicians in prognostication and mortality risk stratification for their patients. Future work involves adjusting for independent risk factors, which can aid in more detailed prognostication.
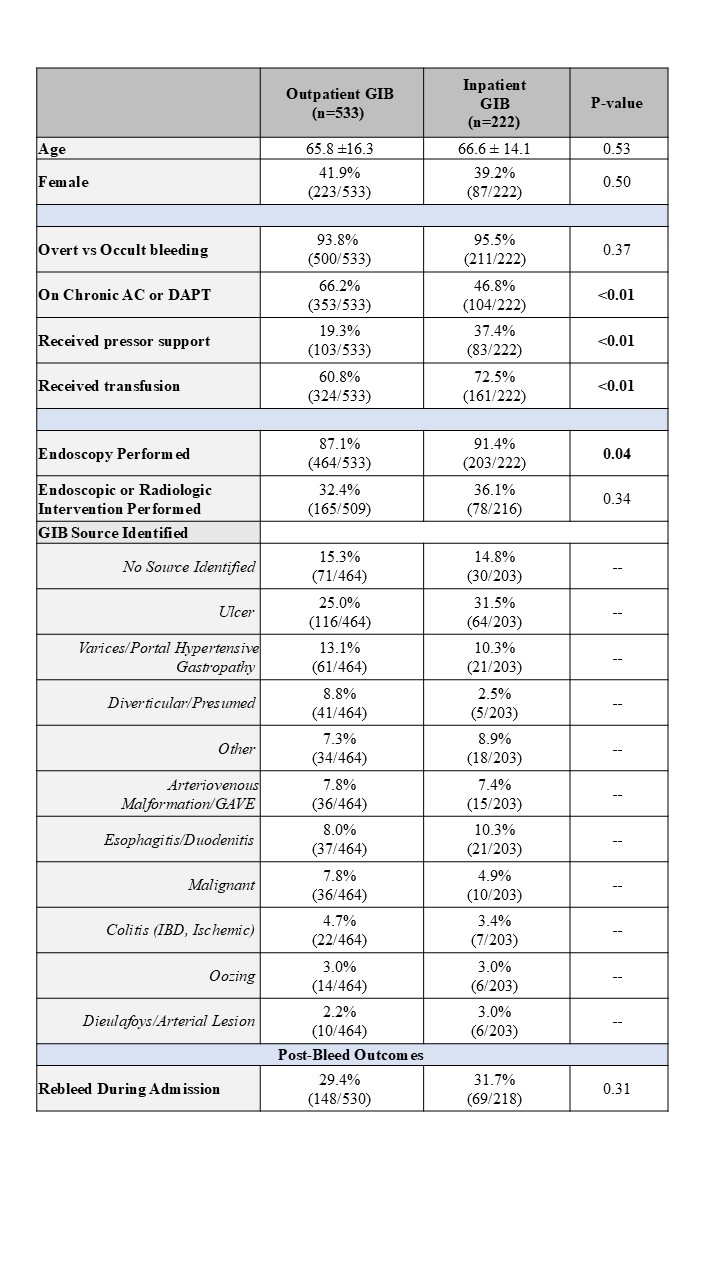
Figure: Table 1. Comparison of patients and bleed characteristics between those who presented with a GIB (outpatient GIB) and those who developed GIB during admission (inpatient GIB). Significance was determined using Chi-squared test. AC: anticoagulation. DAPT: dual antiplatelet therapy. GAVE: gastric antral vascular ectasia. IBD: inflammatory bowel disease.

Figure: Figure 1. Kaplan Meier Survival Curve over 90 days post GIB comparing patients who had GIB on hospital presentation (OP) versus developed GIB during admission (IP) (p < 0.01)
Disclosures:
Miyabi Saito indicated no relevant financial relationships.
Margaret Koester indicated no relevant financial relationships.
James M. Richter indicated no relevant financial relationships.
Sonali Palchaudhuri indicated no relevant financial relationships.
Miyabi Saito, MD1, Margaret Koester, MD, MPH2, James M. Richter, MD, MA3, Sonali Palchaudhuri, MD, MHCI2. P5212 - Patients With a Gastrointestinal Bleed During Hospitalization Have Higher 90-Day Mortality Than Those With GI Bleeding on Hospital Presentation, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

