Tuesday Poster Session
Category: GI Bleeding
P5205 - Gastrointestinal Bleeding in the Very Elderly: A Retrospective Cohort of Patients Aged 90 and Older
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Mustafa Sadek, MD
NCH Healthcare System
Naples, FL
Presenting Author(s)
Award: ACG Presidential Poster Award
Mustafa Sadek, MD, Paul Wasuwanich, MD, Mark Rasnake, MD, William Provance, DO
NCH Healthcare System, Naples, FL
Introduction: Gastrointestinal (GI) bleeding in the very elderly poses unique clinical challenges. As the population of adults aged ≥90 grows, GI breed-related hospitalizations are expected to rise, though data are limited. This study aimed to characterize the presentation, management, and outcomes of GI bleeding in this vulnerable population.
Methods: We conducted a retrospective cohort study of patients aged ≥90 admitted for GI bleed to the NCH Health Care System from January 2022 to April 2025. Of 150 identified via ICD-9/10 codes, 28 were excluded for incomplete data or trauma-related bleeding, leaving 122 for analysis. Data on demographics, labs, and endoscopic findings were collected. Primary outcomes were 28-day mortality, rebleeding, ICU admission, blood transfusion, and length of stay. Multivariable logistic regression was used.
Results: A total of 122 patients aged ≥90 with GI bleed were analyzed (median age 92, range 90–100); 37.7% were female. Most were White (98.4%). Presenting symptoms included melena (59.8%), hematochezia (40.2%), hematemesis (6.6%). Prior GI bleed occurred in 29.5%. Aspirin (35.2%) and direct oral anticoagulants (DOACs) (28.7%) were common home medications. Endoscopy was performed in 73.8%, showing diverticulosis (35.2%), gastritis (32.8%), and duodenal ulcers (13.1%). Interventions included coagulation (18.9%), hemostatic clipping (14.8%), epinephrine (3.3%), and embolization (2.5%). Median hospital stay was 4 days (IQR 3–5), median RBC transfusion was 1 unit (IQR 0–3). Rebleeding occurred in 16.4%, ICU admission in 5.7%, and 28-day mortality in 8.2%. Rebleeding was linked to elevated BUN (OR 1.02, p=0.021); lower risk with gastritis (OR 0.23, p=0.028). Elevated BUN also correlated with ICU admission (OR 1.03, p=0.026). Female sex was associated with a lower 28-day mortality (OR 0.17, p=0.039).
Discussion: In this retrospective study of patients aged ≥90 with GI bleed, elevated BUN was linked to rebleeding and ICU admission, supporting its role as a risk marker. Female sex appeared protective against 28-day mortality, consistent with known sex-based differences in older adults, though interpretation is limited by the smaller female cohort. Gastritis was associated with reduced rebleeding, while duodenal ulcers and low albumin trended toward worse outcomes. While hypotension and elevated INR were associated with higher odds of adverse events, they were not statistically significant. Findings may support early risk stratification in this vulnerable group.
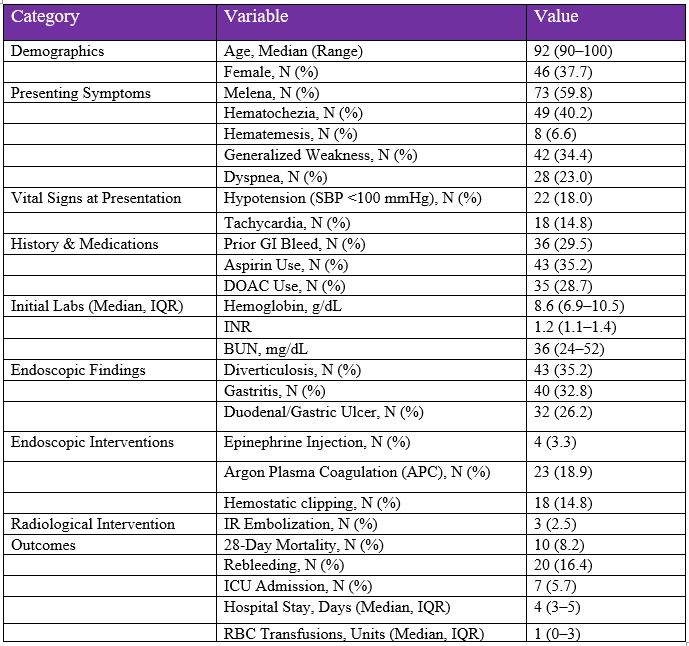
Figure: Table 1: Summary Characteristics of Elderly Patients (≥90 years) with GI Bleeding (N = 122)
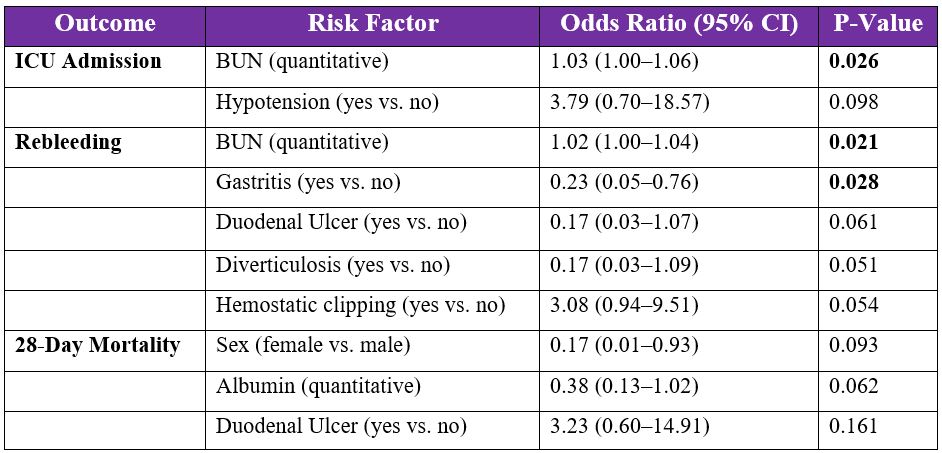
Figure: Table 2: Univariable Risk Factors for Adverse Outcomes in GI Bleeding Patients >90 Years Old
Disclosures:
Mustafa Sadek indicated no relevant financial relationships.
Paul Wasuwanich indicated no relevant financial relationships.
Mark Rasnake indicated no relevant financial relationships.
William Provance indicated no relevant financial relationships.
Mustafa Sadek, MD, Paul Wasuwanich, MD, Mark Rasnake, MD, William Provance, DO. P5205 - Gastrointestinal Bleeding in the Very Elderly: A Retrospective Cohort of Patients Aged 90 and Older, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mustafa Sadek, MD, Paul Wasuwanich, MD, Mark Rasnake, MD, William Provance, DO
NCH Healthcare System, Naples, FL
Introduction: Gastrointestinal (GI) bleeding in the very elderly poses unique clinical challenges. As the population of adults aged ≥90 grows, GI breed-related hospitalizations are expected to rise, though data are limited. This study aimed to characterize the presentation, management, and outcomes of GI bleeding in this vulnerable population.
Methods: We conducted a retrospective cohort study of patients aged ≥90 admitted for GI bleed to the NCH Health Care System from January 2022 to April 2025. Of 150 identified via ICD-9/10 codes, 28 were excluded for incomplete data or trauma-related bleeding, leaving 122 for analysis. Data on demographics, labs, and endoscopic findings were collected. Primary outcomes were 28-day mortality, rebleeding, ICU admission, blood transfusion, and length of stay. Multivariable logistic regression was used.
Results: A total of 122 patients aged ≥90 with GI bleed were analyzed (median age 92, range 90–100); 37.7% were female. Most were White (98.4%). Presenting symptoms included melena (59.8%), hematochezia (40.2%), hematemesis (6.6%). Prior GI bleed occurred in 29.5%. Aspirin (35.2%) and direct oral anticoagulants (DOACs) (28.7%) were common home medications. Endoscopy was performed in 73.8%, showing diverticulosis (35.2%), gastritis (32.8%), and duodenal ulcers (13.1%). Interventions included coagulation (18.9%), hemostatic clipping (14.8%), epinephrine (3.3%), and embolization (2.5%). Median hospital stay was 4 days (IQR 3–5), median RBC transfusion was 1 unit (IQR 0–3). Rebleeding occurred in 16.4%, ICU admission in 5.7%, and 28-day mortality in 8.2%. Rebleeding was linked to elevated BUN (OR 1.02, p=0.021); lower risk with gastritis (OR 0.23, p=0.028). Elevated BUN also correlated with ICU admission (OR 1.03, p=0.026). Female sex was associated with a lower 28-day mortality (OR 0.17, p=0.039).
Discussion: In this retrospective study of patients aged ≥90 with GI bleed, elevated BUN was linked to rebleeding and ICU admission, supporting its role as a risk marker. Female sex appeared protective against 28-day mortality, consistent with known sex-based differences in older adults, though interpretation is limited by the smaller female cohort. Gastritis was associated with reduced rebleeding, while duodenal ulcers and low albumin trended toward worse outcomes. While hypotension and elevated INR were associated with higher odds of adverse events, they were not statistically significant. Findings may support early risk stratification in this vulnerable group.
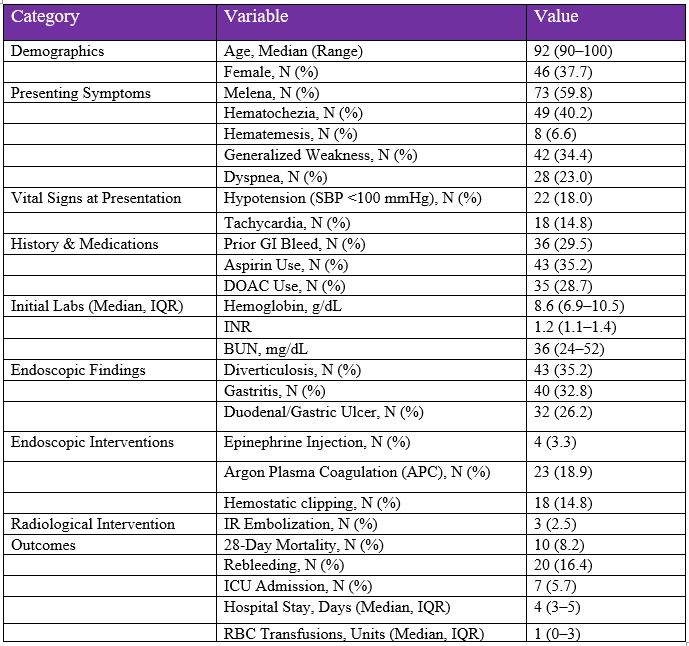
Figure: Table 1: Summary Characteristics of Elderly Patients (≥90 years) with GI Bleeding (N = 122)
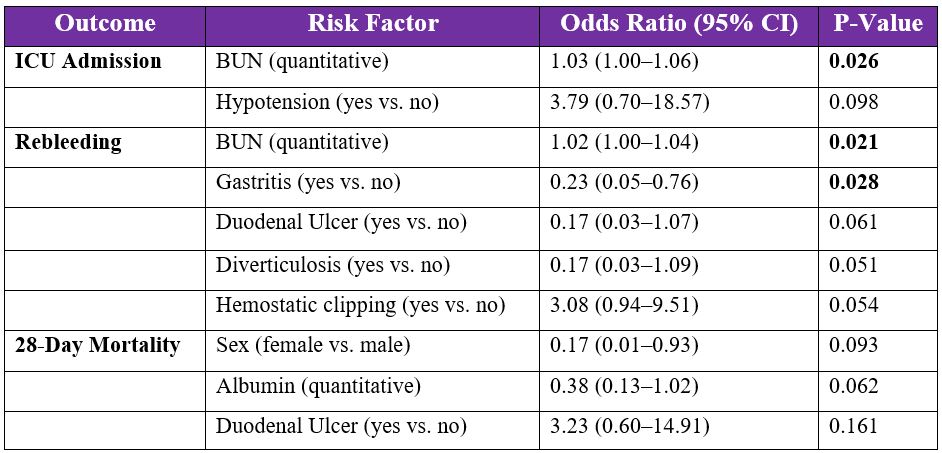
Figure: Table 2: Univariable Risk Factors for Adverse Outcomes in GI Bleeding Patients >90 Years Old
Disclosures:
Mustafa Sadek indicated no relevant financial relationships.
Paul Wasuwanich indicated no relevant financial relationships.
Mark Rasnake indicated no relevant financial relationships.
William Provance indicated no relevant financial relationships.
Mustafa Sadek, MD, Paul Wasuwanich, MD, Mark Rasnake, MD, William Provance, DO. P5205 - Gastrointestinal Bleeding in the Very Elderly: A Retrospective Cohort of Patients Aged 90 and Older, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

