Tuesday Poster Session
Category: General Endoscopy
P5179 - Dysphagia Disguised - A Rare Case of Primary Esophageal Melanoma
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Abrahim Mahmood, DO (he/him/his)
NewYork-Presbyterian/Queens
Greenlawn, NY
Presenting Author(s)
Gagan Verma, DO, MPH, Abrahim Mahmood, DO, Syed Hussain, MD, Sang Kim, MD
NewYork-Presbyterian/Queens, Flushing, NY
Introduction: Primary melanoma of the esophagus is an unusual subtype of mucosal melanoma (MM). MM constitute about 1% of all melanomas, the majority of which are cutaneous melanomas (CM). MM develop from abnormal proliferation of melanocytes in areas protected from ultraviolet light, including oropharyngeal, anorectal, genitourinary and vulvovaginal regions. MM are more aggressive and less receptive to targeted therapies, with poor rates of five-year survival, around 10-20%, compared to 90% for CM. We present a case of dysphagia due to primary esophageal melanoma.
Case Description/
Methods: A 69-year-old man presented to our emergency room with dysphagia. In the ED, CT imaging revealed a large (3 x 5 x 6 cm) mass in the esophagus, confirmed by EGD (Fig 1a-b). A diagnosis of primary esophageal melanoma was made after biopsies showed spindle and epithelioid cells with black granules, which stained negative for iron or fungal organisms. Skin exam was normal. PET-CT did not demonstrate metastatic disease. The patient opted for neoadjuvant immunotherapy over operative intervention. Four months later, he presented with vomiting and inability to tolerate oral secretions. Repeat PET-CT imaging showed widespread metastatic disease. Repeat EGD showed a completely obstructing tumor in mid-esophagus (Figure 1c). Two overlapping, partially-covered esophageal stents were placed for palliation. (Figure 1d). He was discharged with outpatient chemotherapy. He was re-admitted several weeks later with respiratory failure and found to have a large malignant pleural effusion. He suffered a cardiac arrest during the admission and expired, six months after initial diagnosis.
Discussion: Primary melanoma of the esophagus is exceedingly rare and, like other MM, often has an aggressive clinical course. Pathology is crucial to establish the final diagnosis and to provide treatment targets. There is no clear consensus on treatment options for mucosal melanoma. Surgery was previously the only option, but recently immunotherapy has been used due to its efficacy in CM. In this case, the patient opted for neoadjuvant immunotherapy instead of surgical resection; unfortunately, the patient’s disease progressed despite immunotherapy, and he developed complete esophageal obstruction and widespread metastatic disease. This case offers additional perspective on the use of neoadjuvant immunotherapy versus curative resection. Further research into early detection and additional treatment options for these aggressive tumors is needed.
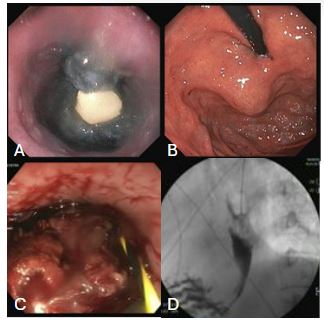
Figure: Figure 1: a) endoscopic view of black tumor b) extrinsic compression c) repeat endoscopy showing obstructing tumor d) fluoroscopy noting esophageal obstruction
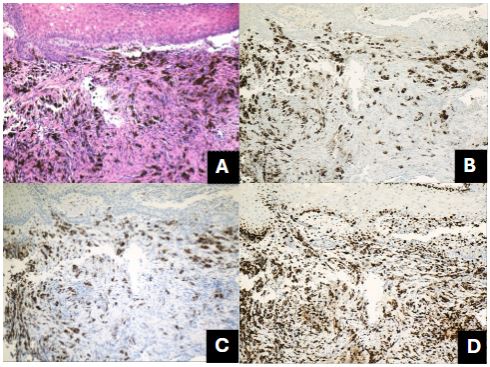
Figure: Figure 2: A) subepithelial malignant melanocytes with melanin granules, H&E stain x 10. (B) scattered tumor cells expressing HMB45 (C) tumor cells expressing S100 marker (D) tumor cells with increased proliferative index of ki67
Disclosures:
Gagan Verma indicated no relevant financial relationships.
Abrahim Mahmood indicated no relevant financial relationships.
Syed Hussain indicated no relevant financial relationships.
Sang Kim indicated no relevant financial relationships.
Gagan Verma, DO, MPH, Abrahim Mahmood, DO, Syed Hussain, MD, Sang Kim, MD. P5179 - Dysphagia Disguised - A Rare Case of Primary Esophageal Melanoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NewYork-Presbyterian/Queens, Flushing, NY
Introduction: Primary melanoma of the esophagus is an unusual subtype of mucosal melanoma (MM). MM constitute about 1% of all melanomas, the majority of which are cutaneous melanomas (CM). MM develop from abnormal proliferation of melanocytes in areas protected from ultraviolet light, including oropharyngeal, anorectal, genitourinary and vulvovaginal regions. MM are more aggressive and less receptive to targeted therapies, with poor rates of five-year survival, around 10-20%, compared to 90% for CM. We present a case of dysphagia due to primary esophageal melanoma.
Case Description/
Methods: A 69-year-old man presented to our emergency room with dysphagia. In the ED, CT imaging revealed a large (3 x 5 x 6 cm) mass in the esophagus, confirmed by EGD (Fig 1a-b). A diagnosis of primary esophageal melanoma was made after biopsies showed spindle and epithelioid cells with black granules, which stained negative for iron or fungal organisms. Skin exam was normal. PET-CT did not demonstrate metastatic disease. The patient opted for neoadjuvant immunotherapy over operative intervention. Four months later, he presented with vomiting and inability to tolerate oral secretions. Repeat PET-CT imaging showed widespread metastatic disease. Repeat EGD showed a completely obstructing tumor in mid-esophagus (Figure 1c). Two overlapping, partially-covered esophageal stents were placed for palliation. (Figure 1d). He was discharged with outpatient chemotherapy. He was re-admitted several weeks later with respiratory failure and found to have a large malignant pleural effusion. He suffered a cardiac arrest during the admission and expired, six months after initial diagnosis.
Discussion: Primary melanoma of the esophagus is exceedingly rare and, like other MM, often has an aggressive clinical course. Pathology is crucial to establish the final diagnosis and to provide treatment targets. There is no clear consensus on treatment options for mucosal melanoma. Surgery was previously the only option, but recently immunotherapy has been used due to its efficacy in CM. In this case, the patient opted for neoadjuvant immunotherapy instead of surgical resection; unfortunately, the patient’s disease progressed despite immunotherapy, and he developed complete esophageal obstruction and widespread metastatic disease. This case offers additional perspective on the use of neoadjuvant immunotherapy versus curative resection. Further research into early detection and additional treatment options for these aggressive tumors is needed.
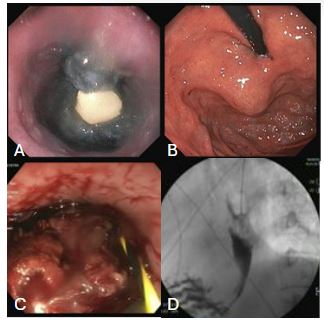
Figure: Figure 1: a) endoscopic view of black tumor b) extrinsic compression c) repeat endoscopy showing obstructing tumor d) fluoroscopy noting esophageal obstruction
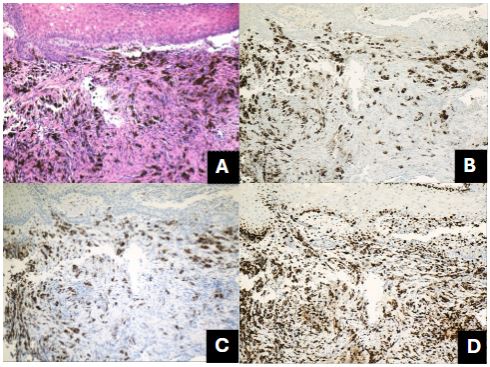
Figure: Figure 2: A) subepithelial malignant melanocytes with melanin granules, H&E stain x 10. (B) scattered tumor cells expressing HMB45 (C) tumor cells expressing S100 marker (D) tumor cells with increased proliferative index of ki67
Disclosures:
Gagan Verma indicated no relevant financial relationships.
Abrahim Mahmood indicated no relevant financial relationships.
Syed Hussain indicated no relevant financial relationships.
Sang Kim indicated no relevant financial relationships.
Gagan Verma, DO, MPH, Abrahim Mahmood, DO, Syed Hussain, MD, Sang Kim, MD. P5179 - Dysphagia Disguised - A Rare Case of Primary Esophageal Melanoma, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
