Tuesday Poster Session
Category: General Endoscopy
P5178 - The Hidden Culprit: A Case of Appendicitis Camouflaged as Inflammatory Bowel Disease
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nakul Ganju, MD (he/him/his)
Department of Medicine, Howard University Hospital
Washington, DC
Presenting Author(s)
Nakul Ganju, MD1, Ahmed Mohamed Ebeid, MD2, Pinky Bai, MD2, Abay Gobezie, MD2, Lakshmi Chirumamilla, MD2, Juan C. Santiago-Gonzalez, MD, MSc2, Angesom Kibreab, MD2
1Department of Medicine, Howard University Hospital, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Appendicitis and inflammatory bowel disease (IBD) may present with overlapping clinical, radiologic, and histologic features, complicating diagnosis. Appendicitis usually causes acute right lower quadrant pain, nausea, and fever, while IBD more often presents with chronic abdominal pain, diarrhea, and weight loss. Cecal involvement may cause appendicitis to mimic IBD on imaging, with terminal ileal thickening and adjacent inflammation. Differentiating them is critical: appendicitis often needs urgent surgery, whereas IBD is treated medically. Misdiagnosis delays care and increases risk of complications.
Case Description/
Methods: A 24-year-old male with no significant history presented with three days of intermittent abdominal pain, nausea, non-bloody vomiting, fever, two weeks of diarrhea, poor intake, and dysuria. On admission, he was febrile and leukocytotic. CT abdomen/pelvis showed dilated bowel loops, pelvic free fluid, and terminal ileal thickening without a visible appendix—suggestive of terminal ileitis or IBD. He was given IV fluids, antibiotics, and empiric corticosteroids (stopped next day). Despite therapy, symptoms and inflammatory markers persisted. Repeat imaging showed a new pelvic abscess; drainage was deferred due to technical constraints. Colonoscopy to evaluate for IBD revealed erythema, edema, and bulging at the appendiceal orifice, raising concern for appendicitis. Follow-up imaging showed abscess shrinkage, and the patient improved clinically. He was discharged on oral antibiotics with elective appendectomy planned.
Discussion: This case highlights challenges in distinguishing appendicitis from IBD, especially with terminal ileitis and equivocal imaging. Early steroid use, common in IBD, can worsen infections or obscure surgical pathology. Though rarely used for appendicitis, colonoscopy provided the critical clue. A multidisciplinary approach—gastroenterology, surgery, radiology—was key to diagnosis. Clinicians must consider alternatives when presentations are atypical or unresponsive. This case underscores the value of diagnostic flexibility in overlapping abdominal syndromes.
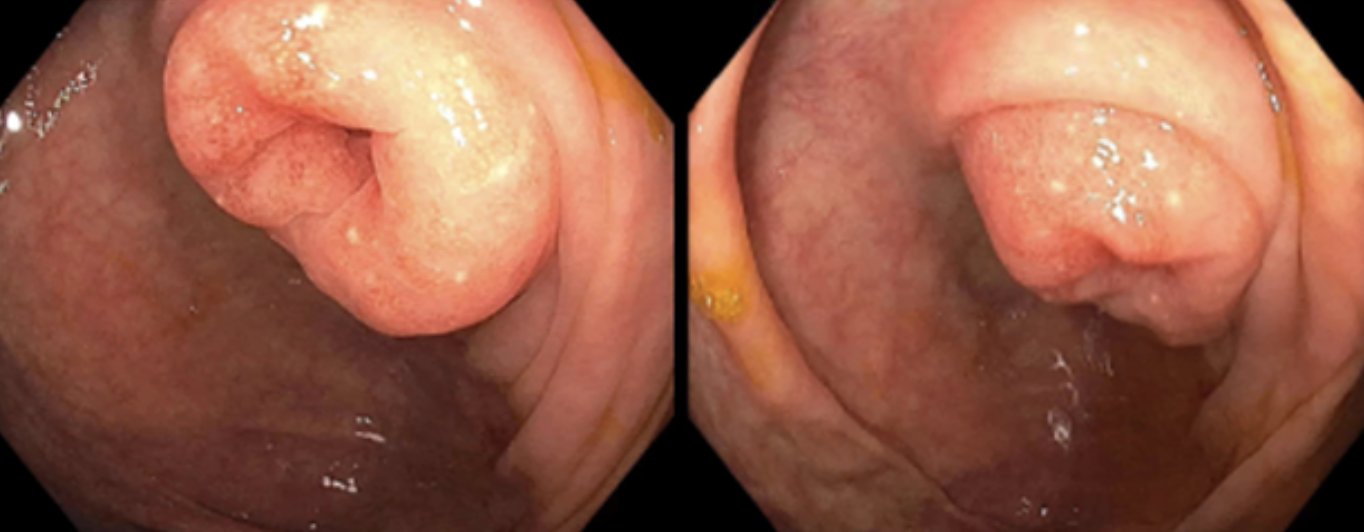
Figure: Figure 1. Edematous, erythematous appendiceal orifice concerning for appendicitis.
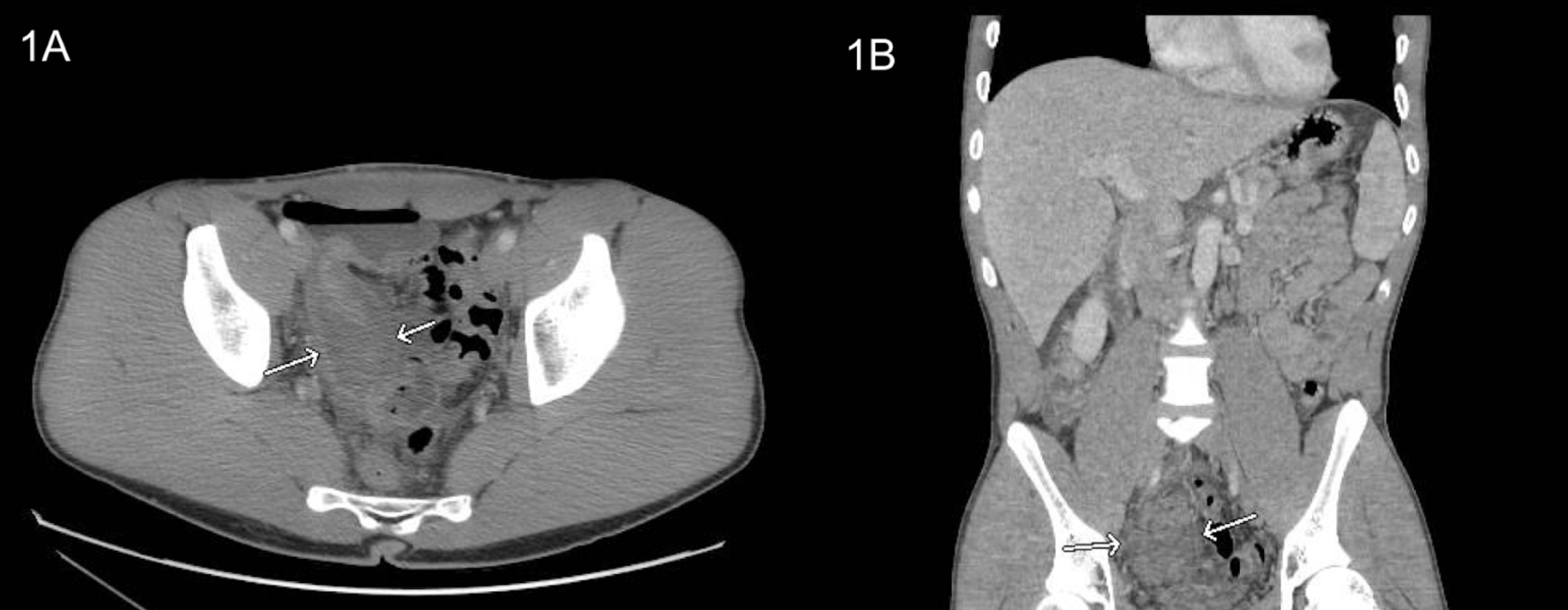
Figure: Figure 1. Initial CT Abdomen/Pelvis imaging revealed indeterminate fluid-containing structures in the right lower quadrant, displacing pelvic bowel loops to the left. These findings were initially suspected to represent a repeated segment of the terminal ileum or an inflammatory process. (A) Transverse image; (B) Coronal image.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Ahmed Mohamed Ebeid indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Abay Gobezie indicated no relevant financial relationships.
Lakshmi Chirumamilla indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Nakul Ganju, MD1, Ahmed Mohamed Ebeid, MD2, Pinky Bai, MD2, Abay Gobezie, MD2, Lakshmi Chirumamilla, MD2, Juan C. Santiago-Gonzalez, MD, MSc2, Angesom Kibreab, MD2. P5178 - The Hidden Culprit: A Case of Appendicitis Camouflaged as Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Medicine, Howard University Hospital, Washington, DC; 2Howard University Hospital, Washington, DC
Introduction: Appendicitis and inflammatory bowel disease (IBD) may present with overlapping clinical, radiologic, and histologic features, complicating diagnosis. Appendicitis usually causes acute right lower quadrant pain, nausea, and fever, while IBD more often presents with chronic abdominal pain, diarrhea, and weight loss. Cecal involvement may cause appendicitis to mimic IBD on imaging, with terminal ileal thickening and adjacent inflammation. Differentiating them is critical: appendicitis often needs urgent surgery, whereas IBD is treated medically. Misdiagnosis delays care and increases risk of complications.
Case Description/
Methods: A 24-year-old male with no significant history presented with three days of intermittent abdominal pain, nausea, non-bloody vomiting, fever, two weeks of diarrhea, poor intake, and dysuria. On admission, he was febrile and leukocytotic. CT abdomen/pelvis showed dilated bowel loops, pelvic free fluid, and terminal ileal thickening without a visible appendix—suggestive of terminal ileitis or IBD. He was given IV fluids, antibiotics, and empiric corticosteroids (stopped next day). Despite therapy, symptoms and inflammatory markers persisted. Repeat imaging showed a new pelvic abscess; drainage was deferred due to technical constraints. Colonoscopy to evaluate for IBD revealed erythema, edema, and bulging at the appendiceal orifice, raising concern for appendicitis. Follow-up imaging showed abscess shrinkage, and the patient improved clinically. He was discharged on oral antibiotics with elective appendectomy planned.
Discussion: This case highlights challenges in distinguishing appendicitis from IBD, especially with terminal ileitis and equivocal imaging. Early steroid use, common in IBD, can worsen infections or obscure surgical pathology. Though rarely used for appendicitis, colonoscopy provided the critical clue. A multidisciplinary approach—gastroenterology, surgery, radiology—was key to diagnosis. Clinicians must consider alternatives when presentations are atypical or unresponsive. This case underscores the value of diagnostic flexibility in overlapping abdominal syndromes.
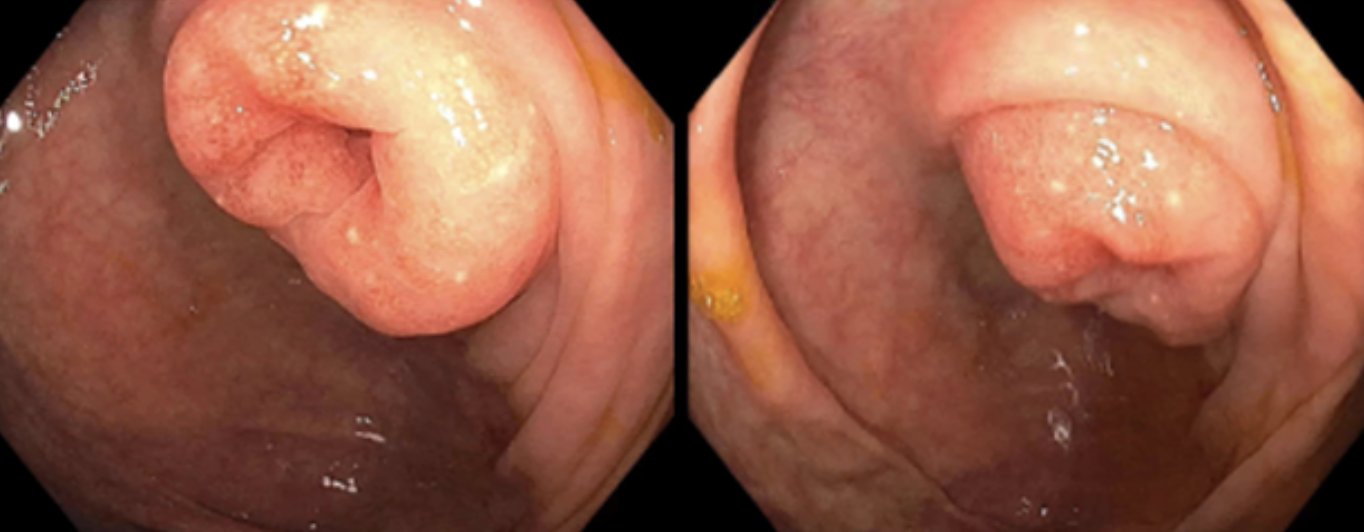
Figure: Figure 1. Edematous, erythematous appendiceal orifice concerning for appendicitis.
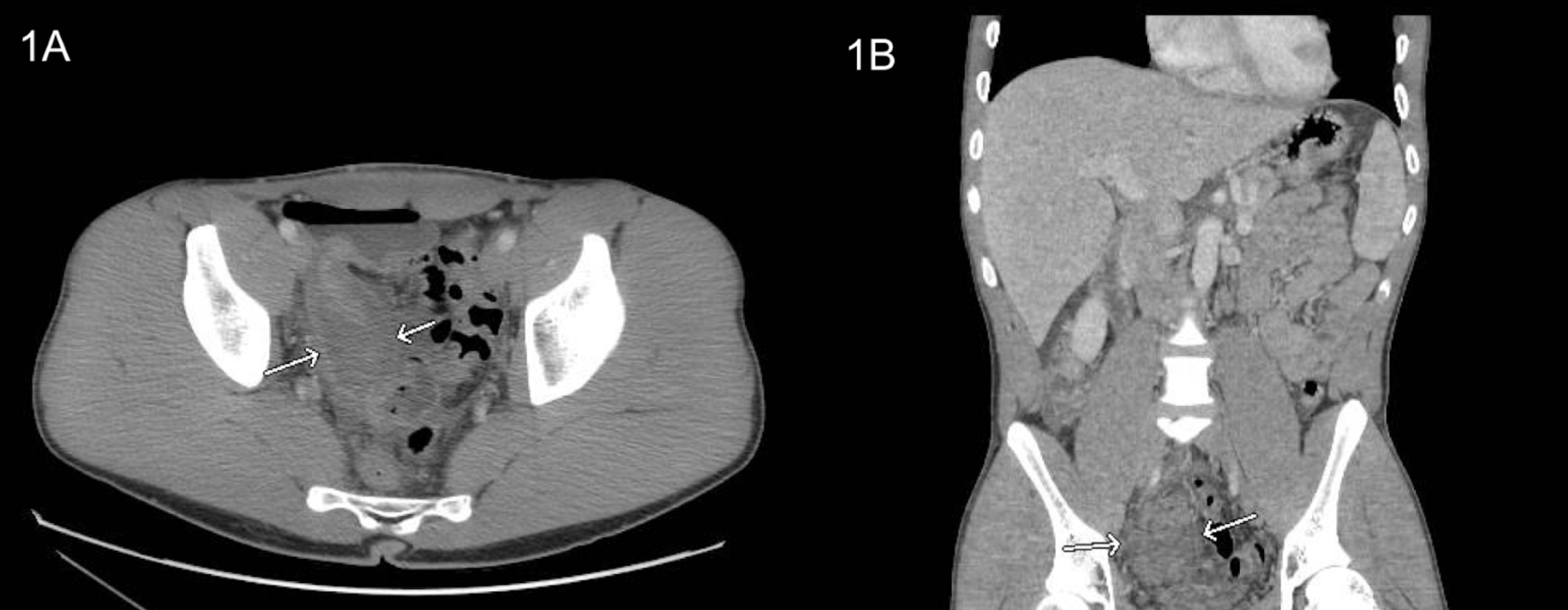
Figure: Figure 1. Initial CT Abdomen/Pelvis imaging revealed indeterminate fluid-containing structures in the right lower quadrant, displacing pelvic bowel loops to the left. These findings were initially suspected to represent a repeated segment of the terminal ileum or an inflammatory process. (A) Transverse image; (B) Coronal image.
Disclosures:
Nakul Ganju indicated no relevant financial relationships.
Ahmed Mohamed Ebeid indicated no relevant financial relationships.
Pinky Bai indicated no relevant financial relationships.
Abay Gobezie indicated no relevant financial relationships.
Lakshmi Chirumamilla indicated no relevant financial relationships.
Juan Santiago-Gonzalez indicated no relevant financial relationships.
Angesom Kibreab indicated no relevant financial relationships.
Nakul Ganju, MD1, Ahmed Mohamed Ebeid, MD2, Pinky Bai, MD2, Abay Gobezie, MD2, Lakshmi Chirumamilla, MD2, Juan C. Santiago-Gonzalez, MD, MSc2, Angesom Kibreab, MD2. P5178 - The Hidden Culprit: A Case of Appendicitis Camouflaged as Inflammatory Bowel Disease, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
