Tuesday Poster Session
Category: General Endoscopy
P5171 - Biliary Peritonitis Without Luminal Perforation After Pan-Endoscopy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Elona Poltiyelova, DO
Westchester Medical Center
Valhalla, NY
Presenting Author(s)
Elona Poltiyelova, DO1, Naveena Sunkara, MD1, Jordan Kirsch, DO1, Matthew Bronstein, MD1, Virendra Tewari, MBBS, MD, DM, FACG2
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
Introduction: Acute abdomen following endoscopic procedures is most commonly due to luminal perforation. The incidence of perforation ranges from 0.005% to 0.085% for colonoscopy and from 0.01% to 0.03% for esophagogastroduodenoscopy (EGD). Extraluminal injuries, by contrast, are extremely rare, with an estimated incidence of only 0.0005% to 0.033% following colonoscopy. We present a rare case of acute abdomen secondary to biliary peritonitis following a combined EGD and colonoscopy procedure.
Case Description/
Methods: An 82 yo M with PMH of CAD, HTN, DM, atrial fibrillation (on long term Eliquis), and open cholecystectomy, was admitted with palpitations and anemia (hemoglobin 7.6). There was no h/o overt GI bleed. His last colonoscopy was 6 years ago and was normal. After cardiac stabilization, a colonoscopy and EGD with small bowel pill cam placement were performed. The EGD showed mild esophagitis and colonoscopy showed moderate diverticulosis, with no signs of bleeding. A few hours post-procedure, the patient developed abdominal pain and distension with leukocytosis and elevated lactic acid of 3.5, though hemoglobin was unchanged. Two abdominal CT scans over the next 24 hours were unrevealing. He then underwent diagnostic laparoscopy which was converted into exploratory laparotomy after bilious fluid was noted in the upper abdomen anterior to the stomach, as well as in the right upper quadrant (RUQ), with significant adhesions noted in the RUQ. Adhesions were lysed and two drainage tubes were placed. The entire bowel was examined thoroughly including an intraoperative EGD with air insufflation. No perforation or mucosal trauma was noted. HIDA scan noted active bile leak from the right side of liver. The patient did well after surgery and is currently post op day 3.
Discussion: Our case highlights an extremely rare extraluminal complication of diagnostic endoscopies requiring surgical management. The precise mechanism and exact site of bile leak was not clear despite thorough surgical exploration. We hypothesize that a few adhesions from his previous gallbladder pathology and open cholecystectomy were disrupted during colonoscopy maneuvering, exposing some minor bile duct from the undersurface of the liver. Prompt surgical intervention was crucial, despite negative imaging, in managing this rare complication.
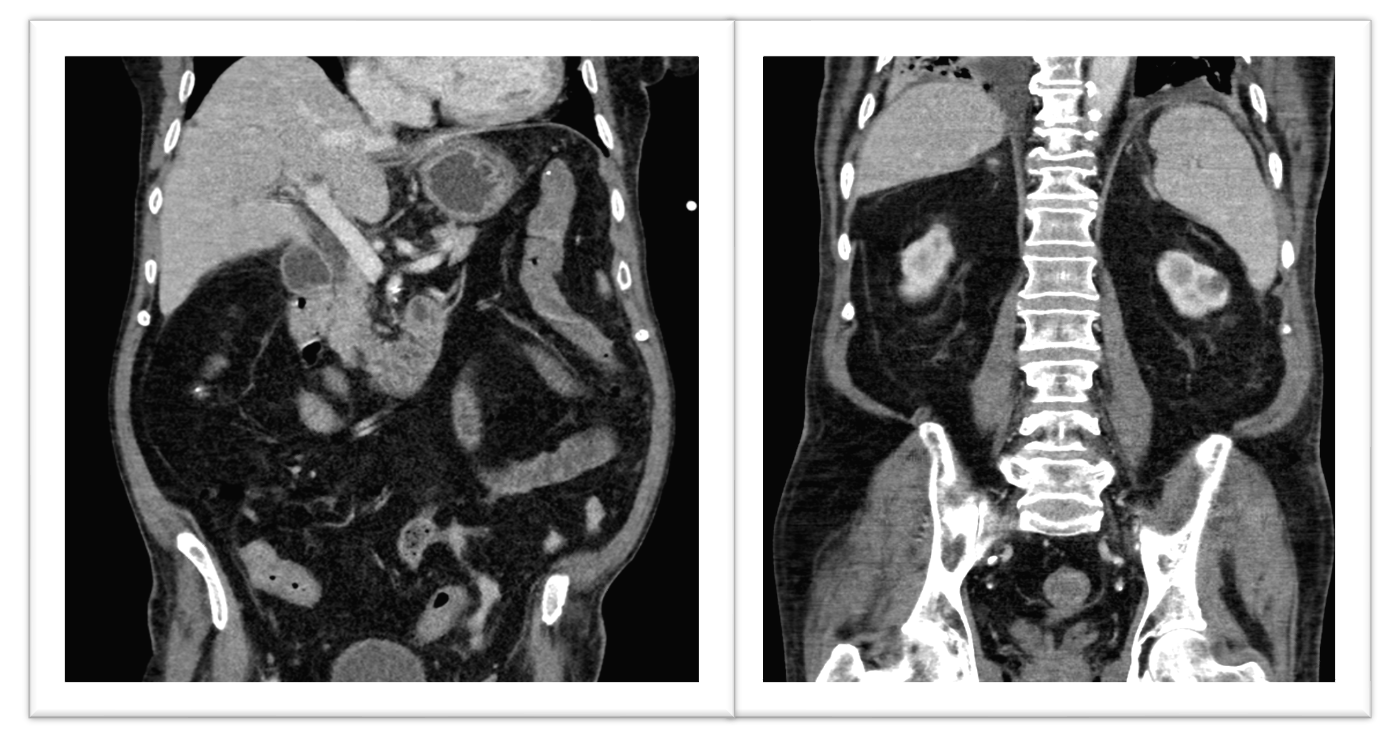
Figure: Image A: CT showing normal liver and spleen.

Figure: Image B: CT showing gaseous distension, no free air.
Disclosures:
Elona Poltiyelova indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Jordan Kirsch indicated no relevant financial relationships.
Matthew Bronstein indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Elona Poltiyelova, DO1, Naveena Sunkara, MD1, Jordan Kirsch, DO1, Matthew Bronstein, MD1, Virendra Tewari, MBBS, MD, DM, FACG2. P5171 - Biliary Peritonitis Without Luminal Perforation After Pan-Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Westchester Medical Center, Valhalla, NY; 2New York Medical College, Valhalla, NY
Introduction: Acute abdomen following endoscopic procedures is most commonly due to luminal perforation. The incidence of perforation ranges from 0.005% to 0.085% for colonoscopy and from 0.01% to 0.03% for esophagogastroduodenoscopy (EGD). Extraluminal injuries, by contrast, are extremely rare, with an estimated incidence of only 0.0005% to 0.033% following colonoscopy. We present a rare case of acute abdomen secondary to biliary peritonitis following a combined EGD and colonoscopy procedure.
Case Description/
Methods: An 82 yo M with PMH of CAD, HTN, DM, atrial fibrillation (on long term Eliquis), and open cholecystectomy, was admitted with palpitations and anemia (hemoglobin 7.6). There was no h/o overt GI bleed. His last colonoscopy was 6 years ago and was normal. After cardiac stabilization, a colonoscopy and EGD with small bowel pill cam placement were performed. The EGD showed mild esophagitis and colonoscopy showed moderate diverticulosis, with no signs of bleeding. A few hours post-procedure, the patient developed abdominal pain and distension with leukocytosis and elevated lactic acid of 3.5, though hemoglobin was unchanged. Two abdominal CT scans over the next 24 hours were unrevealing. He then underwent diagnostic laparoscopy which was converted into exploratory laparotomy after bilious fluid was noted in the upper abdomen anterior to the stomach, as well as in the right upper quadrant (RUQ), with significant adhesions noted in the RUQ. Adhesions were lysed and two drainage tubes were placed. The entire bowel was examined thoroughly including an intraoperative EGD with air insufflation. No perforation or mucosal trauma was noted. HIDA scan noted active bile leak from the right side of liver. The patient did well after surgery and is currently post op day 3.
Discussion: Our case highlights an extremely rare extraluminal complication of diagnostic endoscopies requiring surgical management. The precise mechanism and exact site of bile leak was not clear despite thorough surgical exploration. We hypothesize that a few adhesions from his previous gallbladder pathology and open cholecystectomy were disrupted during colonoscopy maneuvering, exposing some minor bile duct from the undersurface of the liver. Prompt surgical intervention was crucial, despite negative imaging, in managing this rare complication.
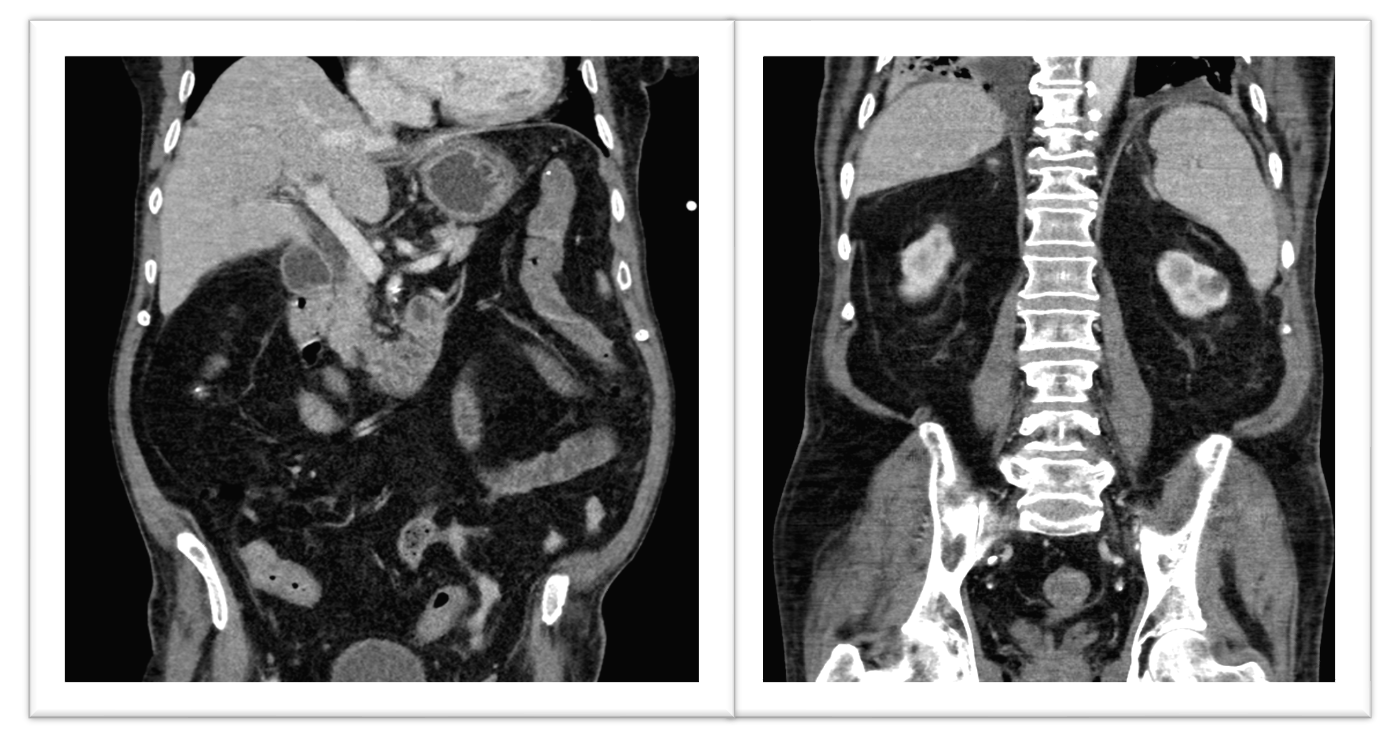
Figure: Image A: CT showing normal liver and spleen.

Figure: Image B: CT showing gaseous distension, no free air.
Disclosures:
Elona Poltiyelova indicated no relevant financial relationships.
Naveena Sunkara indicated no relevant financial relationships.
Jordan Kirsch indicated no relevant financial relationships.
Matthew Bronstein indicated no relevant financial relationships.
Virendra Tewari indicated no relevant financial relationships.
Elona Poltiyelova, DO1, Naveena Sunkara, MD1, Jordan Kirsch, DO1, Matthew Bronstein, MD1, Virendra Tewari, MBBS, MD, DM, FACG2. P5171 - Biliary Peritonitis Without Luminal Perforation After Pan-Endoscopy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
