Tuesday Poster Session
Category: General Endoscopy
P5167 - The Double Pylorus Illusion: A Rare Case of Lumen-to-Lumen Perforation From a Gastric Ulcer
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Sant K. Yadav, MBBS (he/him/his)
Corewell Health William Beaumont University Hospital
Royal Oak, MI
Presenting Author(s)
Sant K. Yadav, MBBS, Samiksha Pandey, MD, Pitambar Khanal, MBBS, Wael Dahhan, MD
Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Peptic ulcer disease (PUD) is most commonly associated with Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs), typically affecting the gastric antrum or duodenal bulb. Rarely, ulcers form long, deep lesions that cross anatomical boundaries, complicating diagnosis and treatment. Such extensive ulcers may result in serious outcomes, including penetration into adjacent organs or fistula formation. We present a rare case of lumen-to-lumen perforation of a gastric ulcer mimicking a second pylorus.
Case Description/
Methods: A 74-year-old woman with a history of abdominal surgeries and ovarian cancer was transferred from an outside hospital (OSH) with presumed necrotizing pancreatitis. She had experienced one month of intermittent postprandial epigastric and left upper quadrant pain, along with nausea and recent vomiting. She denied NSAID or steroid use, alcohol, smoking, or gastrointestinal bleeding. An Esophagogastroduodenoscopy (EGD) performed a year ago was normal. At the OSH, lipase was 157 U/L, amylase 120 U/L. CT showed a 1.8 cm lesion near the pancreatic head and gallstones, without biliary dilation. On arrival, she was hemodynamically stable. Labs revealed hemoglobin 9.4 g/dL, WBC 8.8 × 10⁹/L, creatinine 0.66 mg/dL, lipase 10 U/L, AST 30 U/L, and ALT 11 U/L. MRCP showed a 2.5 × 1.5 cm deep posterior antral ulcer with inflammatory changes close to the gastroduodenal artery. EGD confirmed a single 3cm x 2.5cm clean-based posterior antral ulcer perforating into the duodenal bulb, forming a lumen-to-lumen connection that mimicked a double pylorus (Figure 1). Biopsies showed mild active gastritis and ulceration without H. pylori. She was started on a high-dose proton pump inhibitor (PPI).
Discussion: This case highlights a rare form of PUD presenting as a penetrating posterior antral ulcer creating a gastroduodenal fistula. Conservative PPI therapy with H. pylori gastritis treatment if positive is the standard management. Surgery is indicated if uncontrolled bleeding, perforation, or later complication of severe scarred gastric outlet obstruction. The endoscopic finding of large inter-luminal gastro-duodenal fistulizing ulcers is rare, mimicking a double pylorus impression during endoscopic examination and adding another variant description of peptic ulcer disease pathology. Repeat EGD with biopsies in 12 weeks is advised to rule out malignancy.
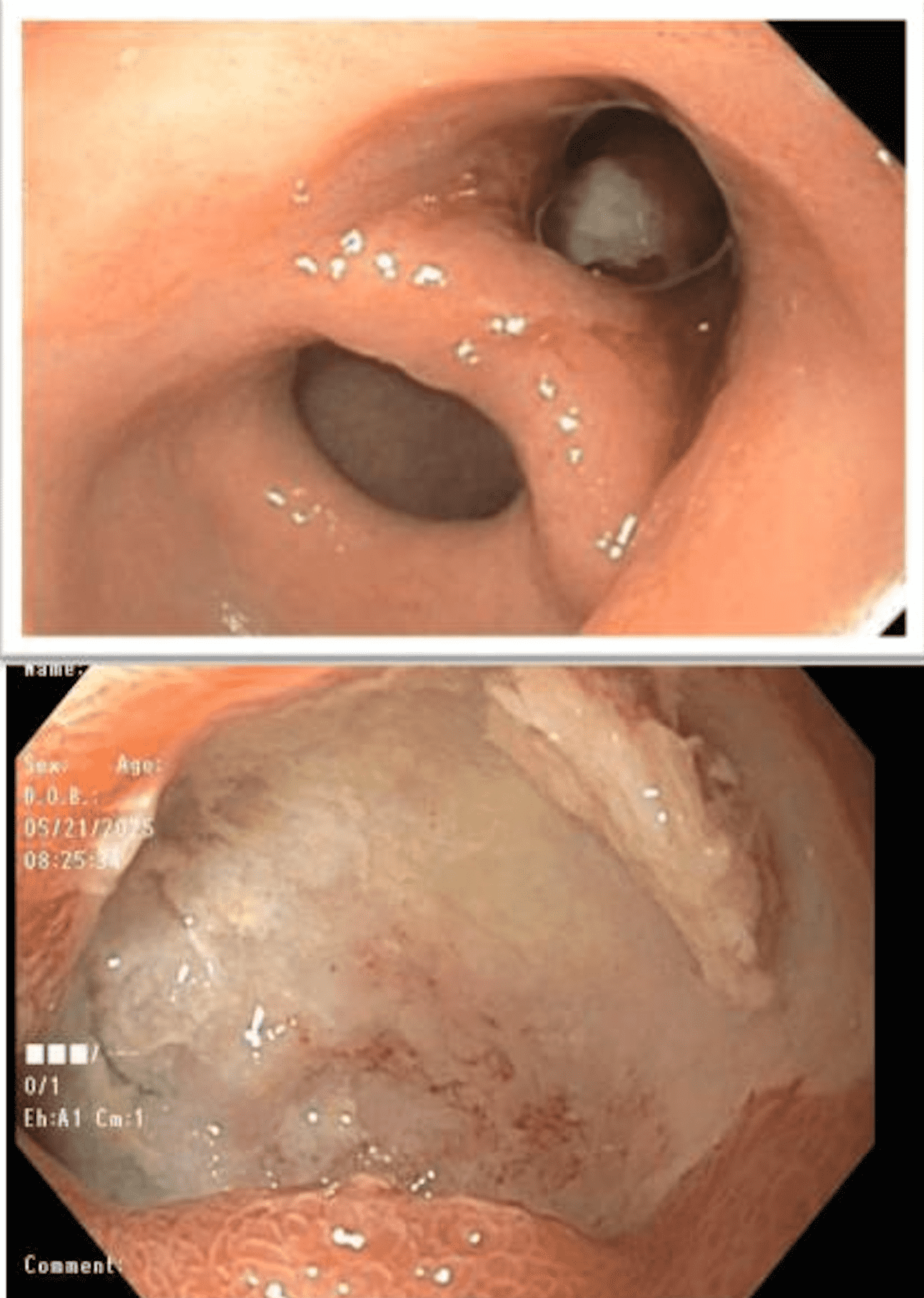
Figure: Endoscopic image of a gastric ulcer perforated to the duodenal bulb, causing a lumen-to-lumen perforation. (a) Gastric Antral Ulcer (b) Duodenal Bulb Ulcer
Disclosures:
Sant Yadav indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Pitambar Khanal indicated no relevant financial relationships.
Wael Dahhan indicated no relevant financial relationships.
Sant K. Yadav, MBBS, Samiksha Pandey, MD, Pitambar Khanal, MBBS, Wael Dahhan, MD. P5167 - The Double Pylorus Illusion: A Rare Case of Lumen-to-Lumen Perforation From a Gastric Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Corewell Health William Beaumont University Hospital, Royal Oak, MI
Introduction: Peptic ulcer disease (PUD) is most commonly associated with Helicobacter pylori infection and the use of nonsteroidal anti-inflammatory drugs (NSAIDs), typically affecting the gastric antrum or duodenal bulb. Rarely, ulcers form long, deep lesions that cross anatomical boundaries, complicating diagnosis and treatment. Such extensive ulcers may result in serious outcomes, including penetration into adjacent organs or fistula formation. We present a rare case of lumen-to-lumen perforation of a gastric ulcer mimicking a second pylorus.
Case Description/
Methods: A 74-year-old woman with a history of abdominal surgeries and ovarian cancer was transferred from an outside hospital (OSH) with presumed necrotizing pancreatitis. She had experienced one month of intermittent postprandial epigastric and left upper quadrant pain, along with nausea and recent vomiting. She denied NSAID or steroid use, alcohol, smoking, or gastrointestinal bleeding. An Esophagogastroduodenoscopy (EGD) performed a year ago was normal. At the OSH, lipase was 157 U/L, amylase 120 U/L. CT showed a 1.8 cm lesion near the pancreatic head and gallstones, without biliary dilation. On arrival, she was hemodynamically stable. Labs revealed hemoglobin 9.4 g/dL, WBC 8.8 × 10⁹/L, creatinine 0.66 mg/dL, lipase 10 U/L, AST 30 U/L, and ALT 11 U/L. MRCP showed a 2.5 × 1.5 cm deep posterior antral ulcer with inflammatory changes close to the gastroduodenal artery. EGD confirmed a single 3cm x 2.5cm clean-based posterior antral ulcer perforating into the duodenal bulb, forming a lumen-to-lumen connection that mimicked a double pylorus (Figure 1). Biopsies showed mild active gastritis and ulceration without H. pylori. She was started on a high-dose proton pump inhibitor (PPI).
Discussion: This case highlights a rare form of PUD presenting as a penetrating posterior antral ulcer creating a gastroduodenal fistula. Conservative PPI therapy with H. pylori gastritis treatment if positive is the standard management. Surgery is indicated if uncontrolled bleeding, perforation, or later complication of severe scarred gastric outlet obstruction. The endoscopic finding of large inter-luminal gastro-duodenal fistulizing ulcers is rare, mimicking a double pylorus impression during endoscopic examination and adding another variant description of peptic ulcer disease pathology. Repeat EGD with biopsies in 12 weeks is advised to rule out malignancy.
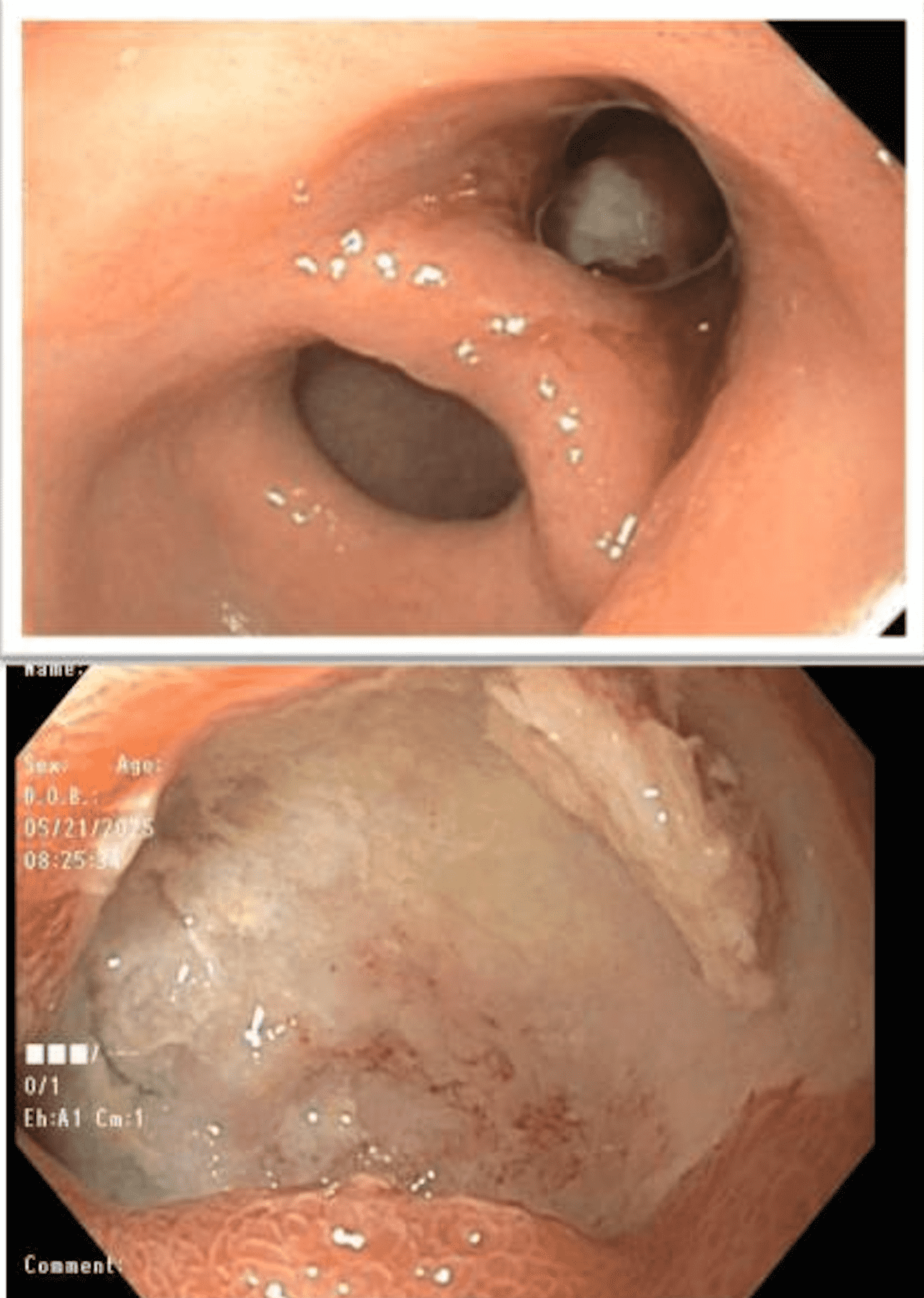
Figure: Endoscopic image of a gastric ulcer perforated to the duodenal bulb, causing a lumen-to-lumen perforation. (a) Gastric Antral Ulcer (b) Duodenal Bulb Ulcer
Disclosures:
Sant Yadav indicated no relevant financial relationships.
Samiksha Pandey indicated no relevant financial relationships.
Pitambar Khanal indicated no relevant financial relationships.
Wael Dahhan indicated no relevant financial relationships.
Sant K. Yadav, MBBS, Samiksha Pandey, MD, Pitambar Khanal, MBBS, Wael Dahhan, MD. P5167 - The Double Pylorus Illusion: A Rare Case of Lumen-to-Lumen Perforation From a Gastric Ulcer, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
