Tuesday Poster Session
Category: General Endoscopy
P5166 - IR Guided Localization of a Pancreatico-Colonic Fistula
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Austin D. Gable, MD
Naval Medical Center San Diego
San Diego, CA
Presenting Author(s)
Austin D. Gable, MD, Scott Liu, MD
Naval Medical Center San Diego, San Diego, CA
Introduction: Fistula formation can be a complication of infected pancreatic necrosis, with high rates of mortality. It often requires surgical management but can also be treated endoscopically. One of the challenges of endoscopic management is locating the fistulas, as they can be small or obscured by inflammation/necrosis. We present a patient with a colonic fistula that was endoscopically located using interventional radiology assistance.
Case Description/
Methods: The patient is a 74-year-old man who was initially diagnosed with cholecystitis, which was managed with a laparoscopic subtotal cholecystectomy. During the operation, he had a superficial injury to the cystic duct, which led to a post-operative bile leak. ERCP and fully covered metal stent placement was performed to bridge the cystic duct. The patient developed severe post-ERCP pancreatitis. He remained symptomatic and repeat CT demonstrated a partially encapsulated, air containing, peripancreatic fluid collection without evidence of necrosis. He underwent IR guided drain placement and feculent fluid output was noted during the procedure. The pancreatic fluid collection grew ESBL E. coli, which was treated with a prolonged course of antibiotics. During an IR drain interrogation, a fistula between the pancreatic fluid collection and the colon at the hepatic flexure was seen. This was managed endoscopically with argon plasma coagulation and an over the scope clip. An additional fistula to the left colon was found on an IR drain interrogation about six weeks later. Gastroenterology performed a joint case with interventional radiology in which the drain was injected with contrast, which was visualized in the peritoneum and the descending colon. A wire was placed through the drain and the drain was removed. A 5 French catheter was then advanced over this wire by IR and the catheter was used to advance further and navigate the fistula tract into the descending colon. Contrast injection confirmed its position, and the catheter was removed, leaving the wire in place in the colon. A colonoscopy was then performed, finding the wire just distal to the splenic flexure. The site was marked with a tattoo and the mucosa surrounding the fistula was ablated with APC. Then an over the scope clip was attached to the scope, the fistula site was found, and the clip was applied, closing the fistula.
Discussion: We present here a case of novel technique using rendezvous procedure with IR to endoscopically close a pancreaticocolonic fistula.
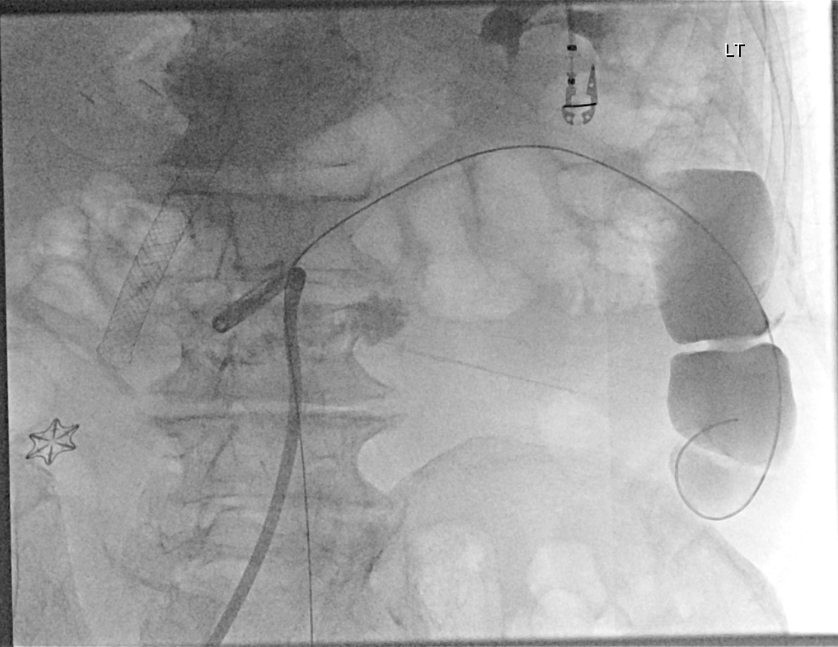
Figure: Fluoroscopic image of contrast pooling in the descending colon and the wire placed in the IR drain, advanced through the fistula and into the descending colon.
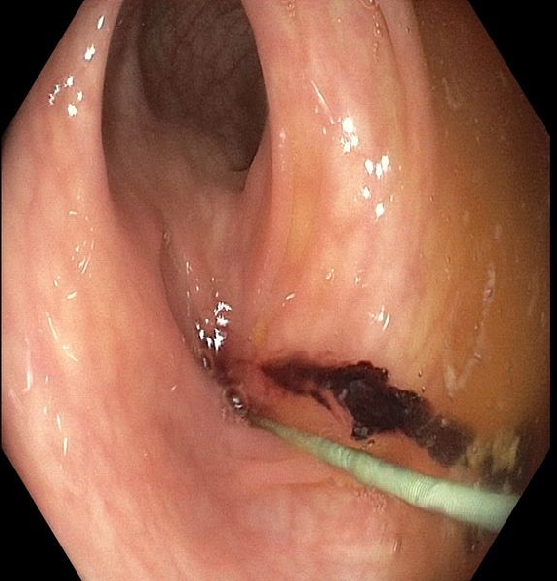
Figure: Endoscopic visualization of the wire tracking through the fistula into the descending colon.
Disclosures:
Austin Gable indicated no relevant financial relationships.
Scott Liu indicated no relevant financial relationships.
Austin D. Gable, MD, Scott Liu, MD. P5166 - IR Guided Localization of a Pancreatico-Colonic Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Naval Medical Center San Diego, San Diego, CA
Introduction: Fistula formation can be a complication of infected pancreatic necrosis, with high rates of mortality. It often requires surgical management but can also be treated endoscopically. One of the challenges of endoscopic management is locating the fistulas, as they can be small or obscured by inflammation/necrosis. We present a patient with a colonic fistula that was endoscopically located using interventional radiology assistance.
Case Description/
Methods: The patient is a 74-year-old man who was initially diagnosed with cholecystitis, which was managed with a laparoscopic subtotal cholecystectomy. During the operation, he had a superficial injury to the cystic duct, which led to a post-operative bile leak. ERCP and fully covered metal stent placement was performed to bridge the cystic duct. The patient developed severe post-ERCP pancreatitis. He remained symptomatic and repeat CT demonstrated a partially encapsulated, air containing, peripancreatic fluid collection without evidence of necrosis. He underwent IR guided drain placement and feculent fluid output was noted during the procedure. The pancreatic fluid collection grew ESBL E. coli, which was treated with a prolonged course of antibiotics. During an IR drain interrogation, a fistula between the pancreatic fluid collection and the colon at the hepatic flexure was seen. This was managed endoscopically with argon plasma coagulation and an over the scope clip. An additional fistula to the left colon was found on an IR drain interrogation about six weeks later. Gastroenterology performed a joint case with interventional radiology in which the drain was injected with contrast, which was visualized in the peritoneum and the descending colon. A wire was placed through the drain and the drain was removed. A 5 French catheter was then advanced over this wire by IR and the catheter was used to advance further and navigate the fistula tract into the descending colon. Contrast injection confirmed its position, and the catheter was removed, leaving the wire in place in the colon. A colonoscopy was then performed, finding the wire just distal to the splenic flexure. The site was marked with a tattoo and the mucosa surrounding the fistula was ablated with APC. Then an over the scope clip was attached to the scope, the fistula site was found, and the clip was applied, closing the fistula.
Discussion: We present here a case of novel technique using rendezvous procedure with IR to endoscopically close a pancreaticocolonic fistula.
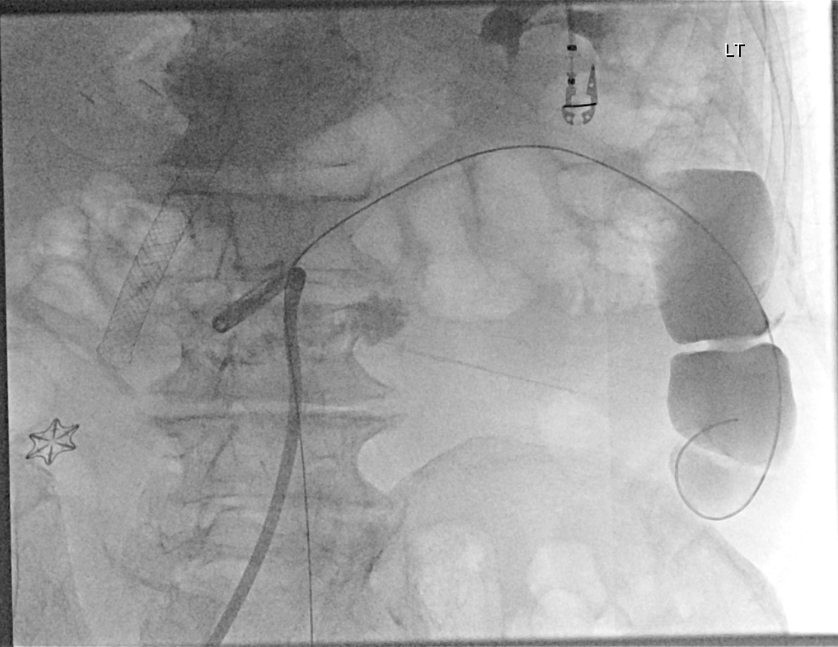
Figure: Fluoroscopic image of contrast pooling in the descending colon and the wire placed in the IR drain, advanced through the fistula and into the descending colon.
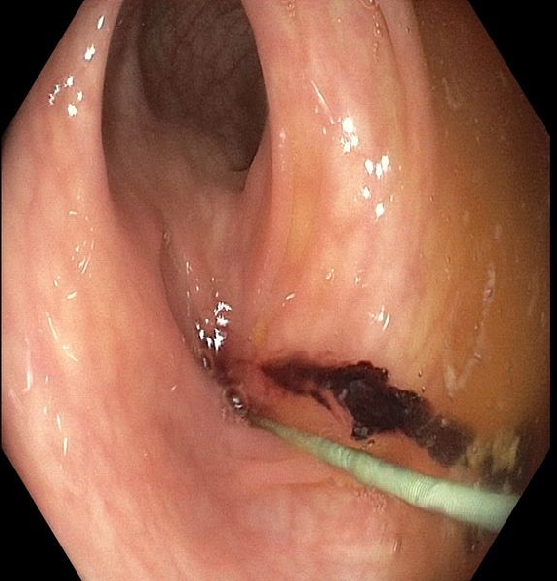
Figure: Endoscopic visualization of the wire tracking through the fistula into the descending colon.
Disclosures:
Austin Gable indicated no relevant financial relationships.
Scott Liu indicated no relevant financial relationships.
Austin D. Gable, MD, Scott Liu, MD. P5166 - IR Guided Localization of a Pancreatico-Colonic Fistula, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
