Tuesday Poster Session
Category: General Endoscopy
P5162 - Beyond the Bladder: Metastatic Urothelial Carcinoma in the Major Papilla
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Katharine H. Cook, DO (she/her/hers)
University of Kentucky
Lexington, KY
Presenting Author(s)
Katharine H. Cook, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Kshitij Thakur, MD1
1University of Kentucky, Lexington, KY; 2College of Medicine, University of Kentucky, Lexington, KY
Introduction: Urothelial Carcinoma (UC) is a commonly diagnosed bladder tumor. The plasmacytoid variant of urothelial carcinoma tends to have an aggressive clinical course with nontraditional metastasis along peritoneal surfaces, tissue planes and the lymphatic system. Presented here is a rare case of plasmacytoid UC with isolated metastasis to the major papilla and duodenum following radical cystectomy.
Case Description/
Methods: The patient is a 70 y.o. female who presented with 2-months of dysuria and hematuria. She underwent transurethral resection of an identified mass in the bladder with pathology demonstrating UC, high grade plasmacytoid variant. Shortly after diagnosis she presented with obstructive AKI and bilateral hydronephrosis requiring placement of bilateral percutaneous nephrostomy tubes. After discussion with urology, she elected to undergo radical cystectomy with ileal conduit and end colostomy creation. Two weeks later, she re-presented to the ED due to abdominal pain, bilious emesis, and inability to tolerate oral intake. She had an NG tube placed for decompression due to concern for post-op ileus and was started on TPN. A follow up CT scan was obtained which revealed an obstructing polypoid mass in the duodenum. Gastroenterology was consulted and preformed upper endoscopy showing a non-traversable solitary mass at the major papilla and duodenum. Biopsies were positive for metastatic plasmacytoid UC. After multidisciplinary discussion the patient ultimately elected for palliative PEG tube placement and was sent home under the care of hospice services.
Discussion: UC accounts for approximately 90% of all bladder neoplasms with Plasmacytoid UC accounting for only 1-3% of invasive phenotypes. The estimated rate of incidence in females is four times higher than males with females presenting at higher clinical stages. Similar to this case, most patients with invasive UC undergo radical cystectomy. In those with plasmacytoid variant, it has been suggested that 33% have intraperitoneal spread and 20% have subsequent metastasis involving other serosal surfaces.
Plasmacytoid UC is an aggressive variant with nontraditional, but characteristic metastatic patterns. Our patient demonstrated a rare presentation of isolated metastasis to the major papilla in the duodenum with only 3 similar cases reported in the literature. Further research must be done to determine plasmacytoid UC’s propensity for metastasis to the duodenum and its surrounding structures given the rarity of its occurrence.
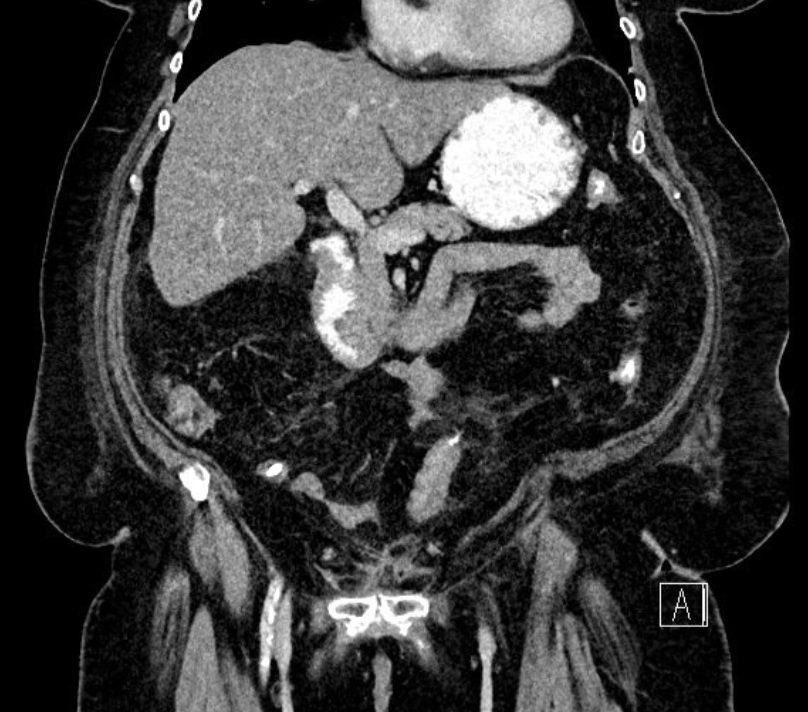
Figure: CT Abdomen and Pelvis: Surgical changes following radical cystectomy and questionable polypoid mass in the descending duodenum near the inferior flexure debris measuring approximately 2.5 cm
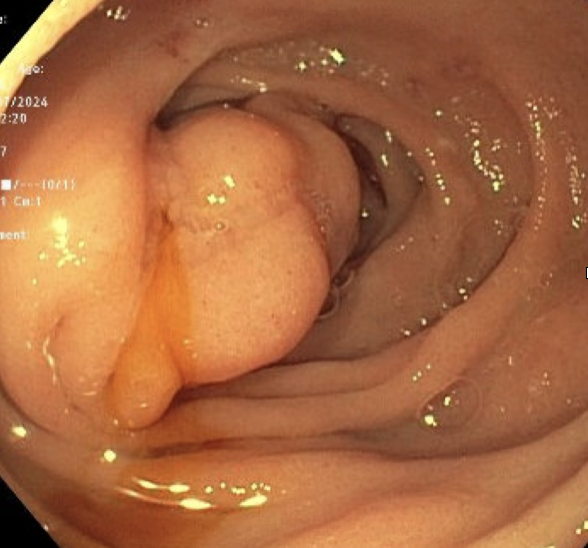
Figure: Endoscopy report:
Single mass (not traversable) in the major papilla, covering three quarters of the circumference of duodenal lumen
Severe edematous mucosa in the duodenal bulb and 2nd part of the duodenum
Disclosures:
Katharine Cook indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Seth Richardson indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Katharine H. Cook, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Kshitij Thakur, MD1. P5162 - Beyond the Bladder: Metastatic Urothelial Carcinoma in the Major Papilla, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Kentucky, Lexington, KY; 2College of Medicine, University of Kentucky, Lexington, KY
Introduction: Urothelial Carcinoma (UC) is a commonly diagnosed bladder tumor. The plasmacytoid variant of urothelial carcinoma tends to have an aggressive clinical course with nontraditional metastasis along peritoneal surfaces, tissue planes and the lymphatic system. Presented here is a rare case of plasmacytoid UC with isolated metastasis to the major papilla and duodenum following radical cystectomy.
Case Description/
Methods: The patient is a 70 y.o. female who presented with 2-months of dysuria and hematuria. She underwent transurethral resection of an identified mass in the bladder with pathology demonstrating UC, high grade plasmacytoid variant. Shortly after diagnosis she presented with obstructive AKI and bilateral hydronephrosis requiring placement of bilateral percutaneous nephrostomy tubes. After discussion with urology, she elected to undergo radical cystectomy with ileal conduit and end colostomy creation. Two weeks later, she re-presented to the ED due to abdominal pain, bilious emesis, and inability to tolerate oral intake. She had an NG tube placed for decompression due to concern for post-op ileus and was started on TPN. A follow up CT scan was obtained which revealed an obstructing polypoid mass in the duodenum. Gastroenterology was consulted and preformed upper endoscopy showing a non-traversable solitary mass at the major papilla and duodenum. Biopsies were positive for metastatic plasmacytoid UC. After multidisciplinary discussion the patient ultimately elected for palliative PEG tube placement and was sent home under the care of hospice services.
Discussion: UC accounts for approximately 90% of all bladder neoplasms with Plasmacytoid UC accounting for only 1-3% of invasive phenotypes. The estimated rate of incidence in females is four times higher than males with females presenting at higher clinical stages. Similar to this case, most patients with invasive UC undergo radical cystectomy. In those with plasmacytoid variant, it has been suggested that 33% have intraperitoneal spread and 20% have subsequent metastasis involving other serosal surfaces.
Plasmacytoid UC is an aggressive variant with nontraditional, but characteristic metastatic patterns. Our patient demonstrated a rare presentation of isolated metastasis to the major papilla in the duodenum with only 3 similar cases reported in the literature. Further research must be done to determine plasmacytoid UC’s propensity for metastasis to the duodenum and its surrounding structures given the rarity of its occurrence.
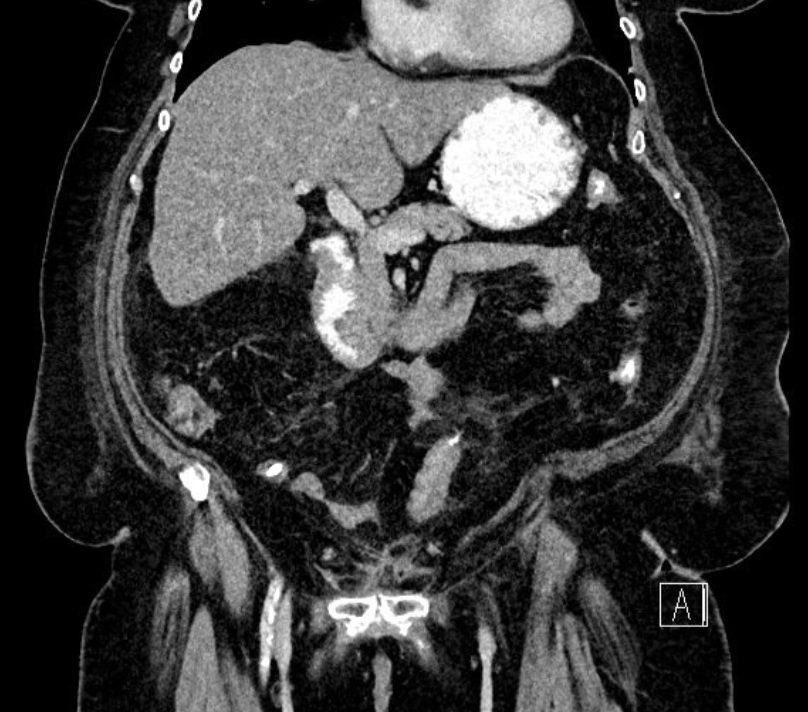
Figure: CT Abdomen and Pelvis: Surgical changes following radical cystectomy and questionable polypoid mass in the descending duodenum near the inferior flexure debris measuring approximately 2.5 cm
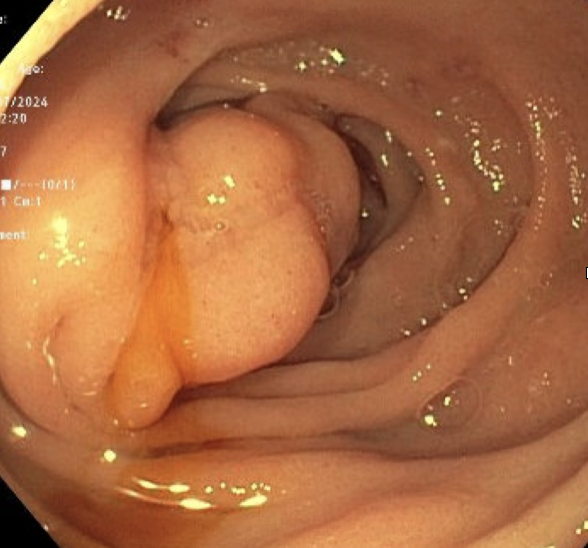
Figure: Endoscopy report:
Single mass (not traversable) in the major papilla, covering three quarters of the circumference of duodenal lumen
Severe edematous mucosa in the duodenal bulb and 2nd part of the duodenum
Disclosures:
Katharine Cook indicated no relevant financial relationships.
Ren Bryant indicated no relevant financial relationships.
Seth Richardson indicated no relevant financial relationships.
Kshitij Thakur indicated no relevant financial relationships.
Katharine H. Cook, DO1, Ren Bryant, DO2, Seth Richardson, MD1, Kshitij Thakur, MD1. P5162 - Beyond the Bladder: Metastatic Urothelial Carcinoma in the Major Papilla, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
