Tuesday Poster Session
Category: General Endoscopy
P5152 - Unmasking a Duodenal Ulcer: A Rare Culprit Behind Mass Effect and Obstructive Jaundice
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Ayah Obeid, MD (she/her/hers)
St. Luke's University Health Network
Bethlehem, PA
Presenting Author(s)
Ayah Obeid, MD1, Frank Lin, DO1, Anuraag Bandi, MD2, Nishit Patel, MD1, Chatargy Kaza, MD1
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Easton, PA
Introduction: Obstructive jaundice is commonly caused by biliary stones or malignancy. However, duodenal ulcers causing external compression of the ampulla are rare and may mimic pancreaticobiliary tumors. We present a case of obstructive jaundice caused by a bleeding duodenal ulcer compressing the ampulla, initially concerning for malignancy, that resolved with endoscopic and medical management.
Case Description/
Methods: A 79-year-old male with no significant past medical history presented with right lower quadrant abdominal pain for 5 days and was diagnosed with acute sigmoid diverticulitis, managed with antibiotics. Incidentally, he was found to have elevated liver enzymes and bilirubin (Table 1). CT revealed eccentric thickening of the descending duodenum. MRCP demonstrated an abrupt cutoff of the common bile duct with intra- and extrahepatic biliary dilatation, raising concern for a duodenal or pancreatic mass (Figure 1A & 1B). EGD revealed a large, deep duodenal ulcer with active oozing compressing the ampulla (Figure 1C). The ulcer was treated with epinephrine injection, Hemoclip placement, and cauterization. The ampulla appeared edematous but intact. ERCP was deferred due to high perforation risk. Following endoscopic therapy, liver enzymes and bilirubin normalized. He completed antibiotics and was discharged on Pantoprazole twice daily. Repeat EGD at 2 months showed a healed ulcer with scarring and a normal-appearing ampulla (Figure 1D). Biopsies revealed chronic duodenitis without dysplasia or malignancy.
Discussion: Obstructive jaundice is commonly due to stones or malignancy, but external compression from a duodenal ulcer is a rare and often an overlooked cause. In our case, a large posterior duodenal ulcer caused direct ampullary compression, leading to biliary obstruction with imaging findings concerning for malignancy. The presence of active bleeding, elevated liver enzymes, and an abrupt biliary cutoff posed a significant diagnostic challenge. Resolution of jaundice and normalization of liver enzymes after ulcer treatment confirmed a benign etiology. This case emphasizes the importance of including peptic ulcer disease in the differential diagnosis of obstructive jaundice and shows that conservative therapy may be both safe and effective when malignancy is excluded.
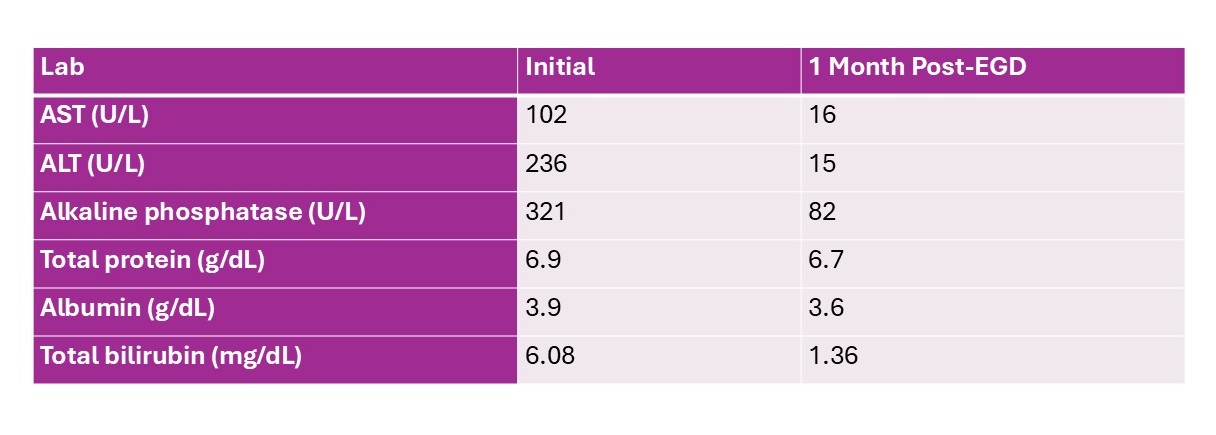
Figure: Table 1: Hepatic labs before and after treating Duodenal ulcer.
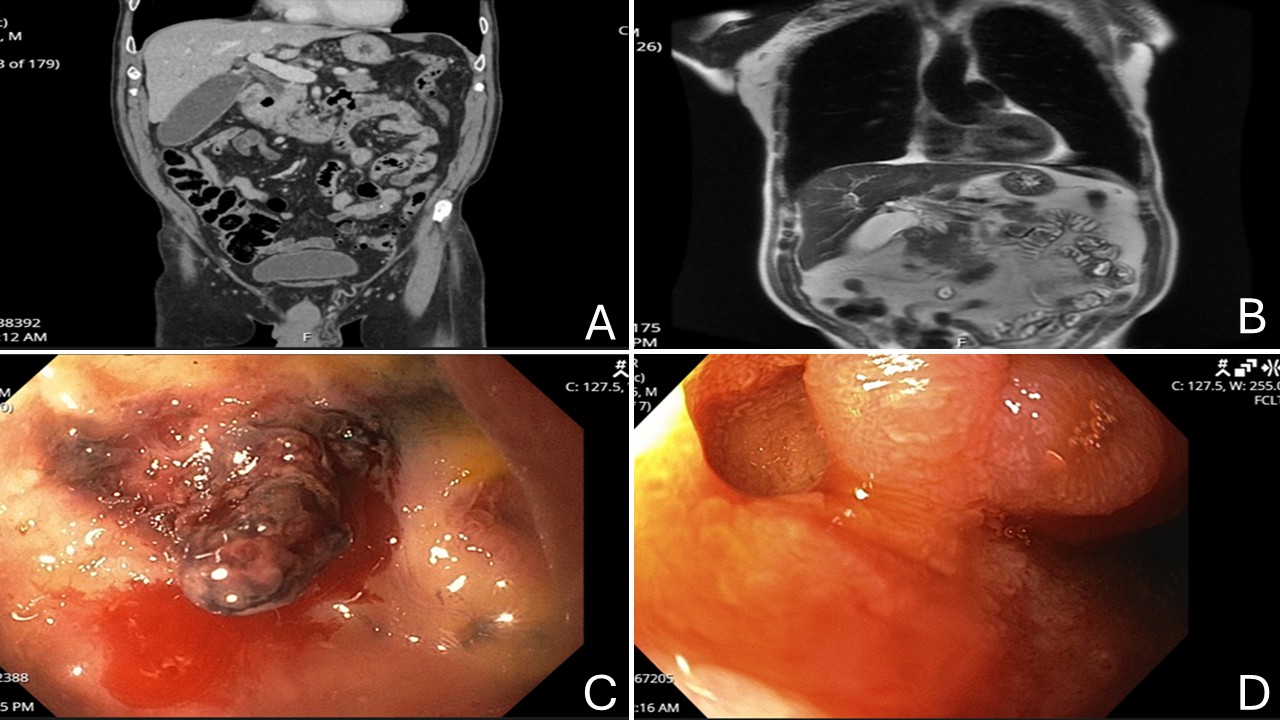
Figure: Figure 1: A: CT scan: The gallbladder is distended. Eccentric wall thickening of the descending duodenum. B: MRCP: Mild intra and extrahepatic biliary ductal dilatation, with abrupt cut off of the common bile duct as it enters the pancreatic head. C: Duodenum-large deep fresh ulcer was noted along the duodenal sweep with a visible vessel and active oozing. D: Duodenum-well-healed ulcer with scarring and some mildly inflamed mucosa around was noted in the postbulbar area.
Disclosures:
Ayah Obeid indicated no relevant financial relationships.
Frank Lin indicated no relevant financial relationships.
Anuraag Bandi indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Chatargy Kaza indicated no relevant financial relationships.
Ayah Obeid, MD1, Frank Lin, DO1, Anuraag Bandi, MD2, Nishit Patel, MD1, Chatargy Kaza, MD1. P5152 - Unmasking a Duodenal Ulcer: A Rare Culprit Behind Mass Effect and Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1St. Luke's University Health Network, Bethlehem, PA; 2St. Luke's University Health Network, Easton, PA
Introduction: Obstructive jaundice is commonly caused by biliary stones or malignancy. However, duodenal ulcers causing external compression of the ampulla are rare and may mimic pancreaticobiliary tumors. We present a case of obstructive jaundice caused by a bleeding duodenal ulcer compressing the ampulla, initially concerning for malignancy, that resolved with endoscopic and medical management.
Case Description/
Methods: A 79-year-old male with no significant past medical history presented with right lower quadrant abdominal pain for 5 days and was diagnosed with acute sigmoid diverticulitis, managed with antibiotics. Incidentally, he was found to have elevated liver enzymes and bilirubin (Table 1). CT revealed eccentric thickening of the descending duodenum. MRCP demonstrated an abrupt cutoff of the common bile duct with intra- and extrahepatic biliary dilatation, raising concern for a duodenal or pancreatic mass (Figure 1A & 1B). EGD revealed a large, deep duodenal ulcer with active oozing compressing the ampulla (Figure 1C). The ulcer was treated with epinephrine injection, Hemoclip placement, and cauterization. The ampulla appeared edematous but intact. ERCP was deferred due to high perforation risk. Following endoscopic therapy, liver enzymes and bilirubin normalized. He completed antibiotics and was discharged on Pantoprazole twice daily. Repeat EGD at 2 months showed a healed ulcer with scarring and a normal-appearing ampulla (Figure 1D). Biopsies revealed chronic duodenitis without dysplasia or malignancy.
Discussion: Obstructive jaundice is commonly due to stones or malignancy, but external compression from a duodenal ulcer is a rare and often an overlooked cause. In our case, a large posterior duodenal ulcer caused direct ampullary compression, leading to biliary obstruction with imaging findings concerning for malignancy. The presence of active bleeding, elevated liver enzymes, and an abrupt biliary cutoff posed a significant diagnostic challenge. Resolution of jaundice and normalization of liver enzymes after ulcer treatment confirmed a benign etiology. This case emphasizes the importance of including peptic ulcer disease in the differential diagnosis of obstructive jaundice and shows that conservative therapy may be both safe and effective when malignancy is excluded.
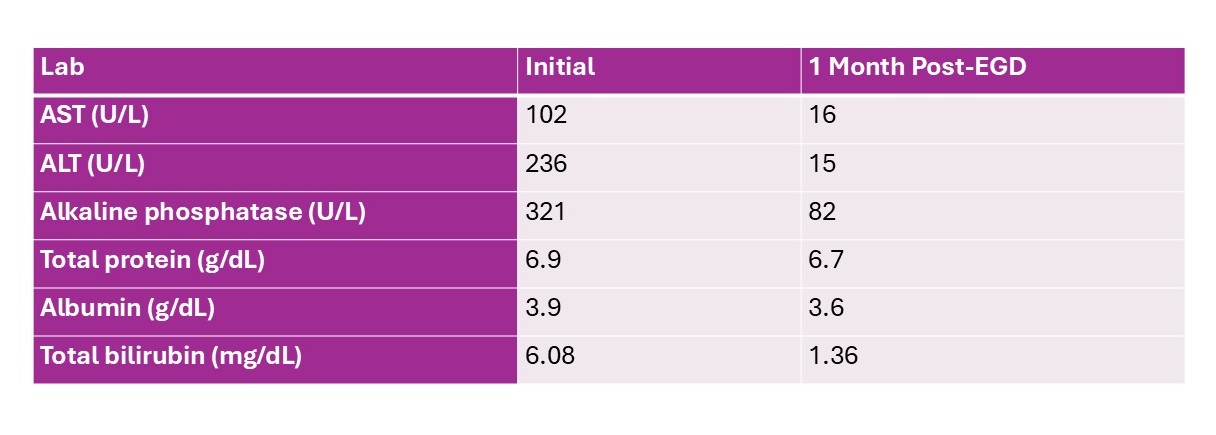
Figure: Table 1: Hepatic labs before and after treating Duodenal ulcer.
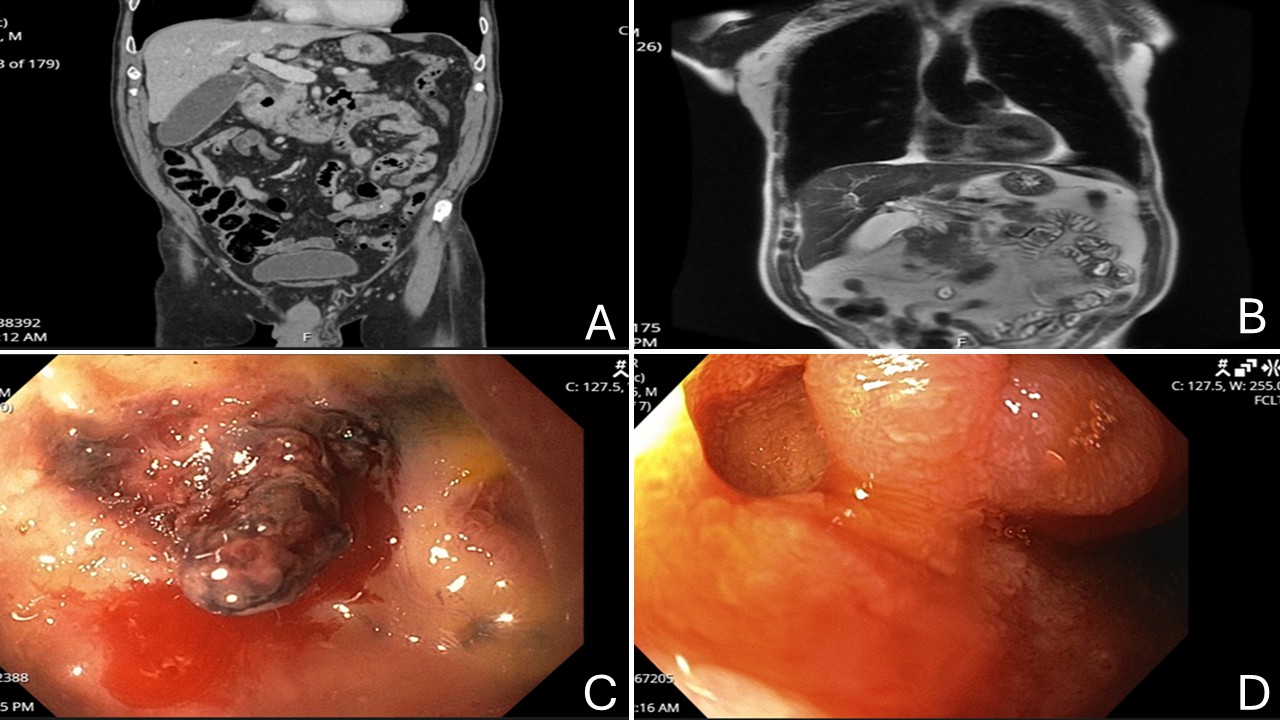
Figure: Figure 1: A: CT scan: The gallbladder is distended. Eccentric wall thickening of the descending duodenum. B: MRCP: Mild intra and extrahepatic biliary ductal dilatation, with abrupt cut off of the common bile duct as it enters the pancreatic head. C: Duodenum-large deep fresh ulcer was noted along the duodenal sweep with a visible vessel and active oozing. D: Duodenum-well-healed ulcer with scarring and some mildly inflamed mucosa around was noted in the postbulbar area.
Disclosures:
Ayah Obeid indicated no relevant financial relationships.
Frank Lin indicated no relevant financial relationships.
Anuraag Bandi indicated no relevant financial relationships.
Nishit Patel indicated no relevant financial relationships.
Chatargy Kaza indicated no relevant financial relationships.
Ayah Obeid, MD1, Frank Lin, DO1, Anuraag Bandi, MD2, Nishit Patel, MD1, Chatargy Kaza, MD1. P5152 - Unmasking a Duodenal Ulcer: A Rare Culprit Behind Mass Effect and Obstructive Jaundice, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
