Tuesday Poster Session
Category: General Endoscopy
P5135 - Comparative Efficacy and Safety of Hybrid Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett’s Esophagus: A Systematic Review and Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Khyati Bidani, MD
Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School
New Brunswick, NJ
Presenting Author(s)
Khyati Bidani, MD1, Vishali Moond, MD2, Vikash Kumar, MD3, Louisa Recinos-Arenas, MD1, Andrew Korman, MD1, Sugirdhana Velpari, MD1, Arkady Broder, MD, FACG1
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Radiofrequency ablation (RFA) has long been the standard endoscopic therapy for dysplastic Barrett’s esophagus (BE). Recently, hybrid argon plasma coagulation (H-APC)—a technique combining submucosal fluid cushioning with APC—has emerged as a promising alternative with potentially improved safety and efficacy profiles. This study aims to systematically evaluate and compare the pooled clinical outcomes and safety of H-APC versus RFA in the treatment of Barrett’s esophagus.
Methods: A comprehensive literature search was conducted across Medline, Embase, PubMed, Cochrane Library, Web of Science, and major conference proceedings through May 2025. Studies reporting outcomes for H-APC or RFA in BE were included. The primary outcomes were histologic remission, complete eradication of intestinal metaplasia (CE-IM), and complete eradication of dysplasia (CE-D). Secondary outcomes included recurrence rates, overall adverse events, and stricture formation. Meta-analyses were performed using a random-effects model, and heterogeneity was assessed using I² statistics.
Results: A total of 16 studies were included in the analysis (H-APC: 8 studies; RFA: 8 studies). H-APC demonstrated higher rates of histologic remission (92.2% [95% CI: 86.1%–95.8%]; I² = 71%) compared to RFA (81.3% [74.9%–86.3%]; I² = 42%), though this difference was not statistically significant (p = 0.09). CE-IM was significantly higher with H-APC (91.6% [85.3%–95.4%]; I² = 73%) than with RFA (82.2% [77.9%–85.7%]; I² = 42%; p = 0.014). CE-D rates were also significantly greater with H-APC (99.5% [97.6%–99.9%]; I² = 0%) compared to RFA (91.1% [87.8%–94.7%]; I² = 56%; p = 0.01). Recurrence rates were comparable (H-APC: 9.3% vs. RFA: 8.0%; p = 0.79). However, H-APC had significantly fewer overall adverse events (4.9% vs. 20.9%; p = 0.04) and strictures (1.9% vs. 8.0%; p = 0.00). (table 1)
Discussion: Hybrid APC appears to be an effective and safer alternative to RFA for the management of Barrett’s esophagus, with superior rates of CE-IM and CE-D and significantly lower rates of adverse events and strictures. These findings support the expanding role of H-APC as a frontline therapy for BE, though prospective head-to-head trials are warranted to validate long-term comparative outcomes.
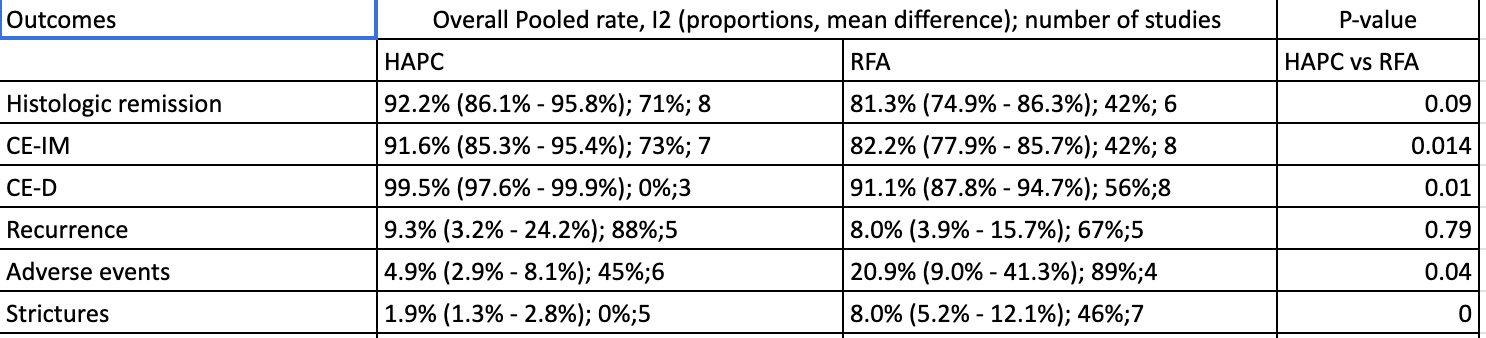
Figure: Table 1: Outcomes of HAPC vs RFA
Disclosures:
Khyati Bidani indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Louisa Recinos-Arenas indicated no relevant financial relationships.
Andrew Korman indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Khyati Bidani, MD1, Vishali Moond, MD2, Vikash Kumar, MD3, Louisa Recinos-Arenas, MD1, Andrew Korman, MD1, Sugirdhana Velpari, MD1, Arkady Broder, MD, FACG1. P5135 - Comparative Efficacy and Safety of Hybrid Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett’s Esophagus: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Saint Peter's University Hospital / Rutgers Robert Wood Johnson Medical School, New Brunswick, NJ; 2Saint Peter's University Hospital/Robert Wood Johnson Medical School loc, New Brunswick, NJ; 3Creighton University School of Medicine, Phoenix, AZ
Introduction: Radiofrequency ablation (RFA) has long been the standard endoscopic therapy for dysplastic Barrett’s esophagus (BE). Recently, hybrid argon plasma coagulation (H-APC)—a technique combining submucosal fluid cushioning with APC—has emerged as a promising alternative with potentially improved safety and efficacy profiles. This study aims to systematically evaluate and compare the pooled clinical outcomes and safety of H-APC versus RFA in the treatment of Barrett’s esophagus.
Methods: A comprehensive literature search was conducted across Medline, Embase, PubMed, Cochrane Library, Web of Science, and major conference proceedings through May 2025. Studies reporting outcomes for H-APC or RFA in BE were included. The primary outcomes were histologic remission, complete eradication of intestinal metaplasia (CE-IM), and complete eradication of dysplasia (CE-D). Secondary outcomes included recurrence rates, overall adverse events, and stricture formation. Meta-analyses were performed using a random-effects model, and heterogeneity was assessed using I² statistics.
Results: A total of 16 studies were included in the analysis (H-APC: 8 studies; RFA: 8 studies). H-APC demonstrated higher rates of histologic remission (92.2% [95% CI: 86.1%–95.8%]; I² = 71%) compared to RFA (81.3% [74.9%–86.3%]; I² = 42%), though this difference was not statistically significant (p = 0.09). CE-IM was significantly higher with H-APC (91.6% [85.3%–95.4%]; I² = 73%) than with RFA (82.2% [77.9%–85.7%]; I² = 42%; p = 0.014). CE-D rates were also significantly greater with H-APC (99.5% [97.6%–99.9%]; I² = 0%) compared to RFA (91.1% [87.8%–94.7%]; I² = 56%; p = 0.01). Recurrence rates were comparable (H-APC: 9.3% vs. RFA: 8.0%; p = 0.79). However, H-APC had significantly fewer overall adverse events (4.9% vs. 20.9%; p = 0.04) and strictures (1.9% vs. 8.0%; p = 0.00). (table 1)
Discussion: Hybrid APC appears to be an effective and safer alternative to RFA for the management of Barrett’s esophagus, with superior rates of CE-IM and CE-D and significantly lower rates of adverse events and strictures. These findings support the expanding role of H-APC as a frontline therapy for BE, though prospective head-to-head trials are warranted to validate long-term comparative outcomes.
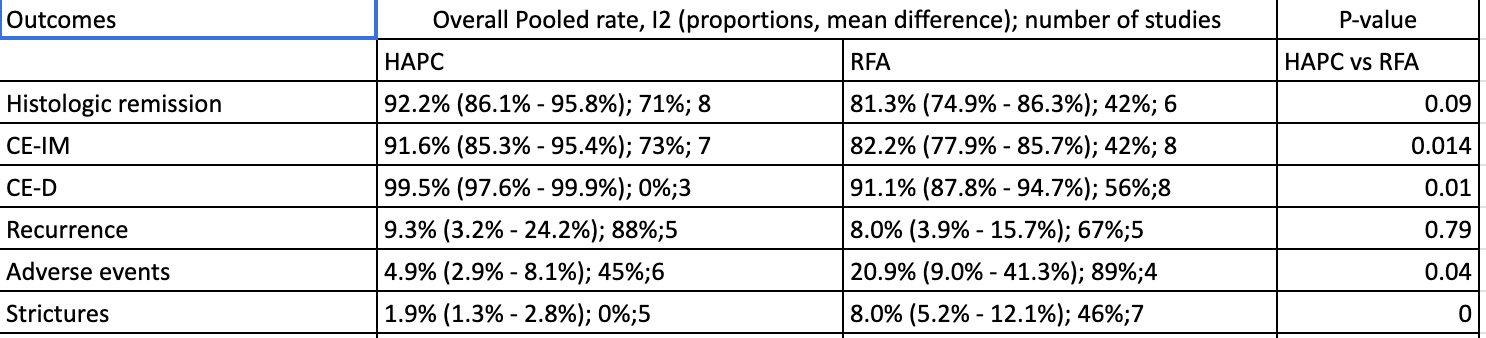
Figure: Table 1: Outcomes of HAPC vs RFA
Disclosures:
Khyati Bidani indicated no relevant financial relationships.
Vishali Moond indicated no relevant financial relationships.
Vikash Kumar indicated no relevant financial relationships.
Louisa Recinos-Arenas indicated no relevant financial relationships.
Andrew Korman indicated no relevant financial relationships.
Sugirdhana Velpari indicated no relevant financial relationships.
Arkady Broder indicated no relevant financial relationships.
Khyati Bidani, MD1, Vishali Moond, MD2, Vikash Kumar, MD3, Louisa Recinos-Arenas, MD1, Andrew Korman, MD1, Sugirdhana Velpari, MD1, Arkady Broder, MD, FACG1. P5135 - Comparative Efficacy and Safety of Hybrid Argon Plasma Coagulation vs Radiofrequency Ablation for Barrett’s Esophagus: A Systematic Review and Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
