Tuesday Poster Session
Category: General Endoscopy
P5134 - Accuracy of Virtual Scale Endoscopy in Colorectal Polyp Size Measurement: Pairwise and Network Meta-Analysis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Islam Rajab, MD
St. Joseph's University Medical Center
Paterson, NJ
Presenting Author(s)
Award: ACG Presidential Poster Award
Mohamed S. Elgendy, MBBCh1, Islam Rajab, MD2, Mohamed Rifai, 3, Amira M. Taha, 4, Abdulrahman Maged, 5, Hosam I. Taha, MBBCh1, Mohamed A. Elgamasy, 5, Mohamed Abuelazm, 5, Mina Fransawy Alkomos, MD2, Walid Baddoura, MD2
1Tanta University, Tanta, Al Gharbiyah, Egypt; 2St. Joseph's University Medical Center, Paterson, NJ; 3Faculty of Medicine, Menoufia university,Shebin El Kom,Egypt, Menoufia, Al Minufiyah, Egypt; 4Fayoum University, Faculty of Medicine, Fayoum, Al Fayyum, Egypt; 5Faculty of Medicine, Tanta University, Tanta, Egypt, Tanta, Al Gharbiyah, Egypt
Introduction: Colorectal cancer (CRC) is a leading cause of cancer death. Accurate in vivo polyp measurement is key for management, but visual assessment (VA) is often unreliable, correctly sizing only half and misclassifying up to one-third. Traditional tools like forceps and snares offer limited precision. Virtual Scale Endoscopy (VSE), a laser-calibrated overlay that adjusts for distance in real-time, shows promise for improving measurement accuracy without compromising efficiency
Methods: A pairwise meta-analysis comparing VSE to VA and a frequentist network meta-analysis (NMA) comparing VSE to VA, snare, and forceps were conducted from PubMed, Cochrane, WoS, Embase, and Scopus. Risk ratios (RR) were calculated for categorical outcomes and mean differences (MD) for continuous outcomes, each with a 95% confidence interval (CI). Intervention rankings were estimated with NMA by the Surface Under the Cumulative Ranking curve (SUCRA).
Results: Twelve studies were included, comprising 1,608 polyps from both clinical and preclinical trials, including 2,866 patients from seven clinical studies. In pairwise analysis, relative accuracy significantly improved with VSE compared to VA in both preclinical (MD 14.14, 95% CI: 6.54–21.74) and clinical settings (MD 14.86, 95% CI: 10.45–19.26). Correct size estimation also improved with VSE (RR 1.96, 95% CI: 1.64–2.33).
In the NMA, VSE reduced misclassification for polyps >5 mm (RR 3.51 vs. VA, 95% CI: 1.88–6.55; RR 3.26 vs. snare, 95% CI: 1.66–6.39), >10 mm (RR 2.08 vs. VA, 95% CI: 1.14–3.81), and >20 mm (RR 2.40 vs. VA, 95% CI: 1.30–4.46; RR 8.00 vs. forceps, 95% CI: 1.17–54.5). No significant differences were observed at size thresholds >3 mm, ≤5 mm, or ≤10 mm. Snare ranked highest for overestimation (SUCRA 69%), followed by VSE (63%), but differences were insignificant. Underestimation was lowest with VSE (SUCRA 80%), though differences from VA, snare, or forceps were insignificant. No significant differences were found for total misclassification (P= 0.438), overestimation (P= 0.617), or underestimation (P= 0.592).
Discussion: VSE significantly improved colorectal polyp size measurement accuracy compared to traditional VA. VSE also reduced measurement variability and misclassification compared to VA, snare, and forceps at clinically critical size thresholds. This can improve decision-making in polypectomy and surveillance, especially for diminutive and small polyps. However, larger multicenter randomized trials are needed to confirm these benefits.
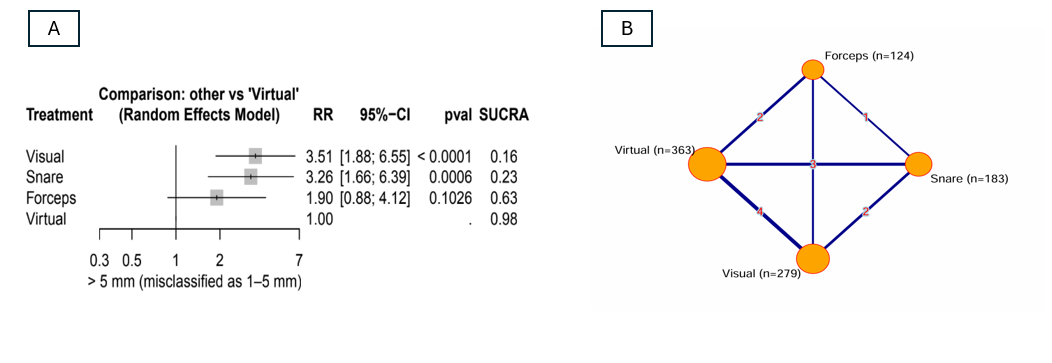
Figure: Figure 1 Shows (A) Laser-based sizing mechanism of Virtual Scale Endoscopy (VSE); (B) forest plots of total relative accuracy; and (C) forest plots of correct polyp size estimation comparing VSE to visual assessment in clinical and preclinical studies
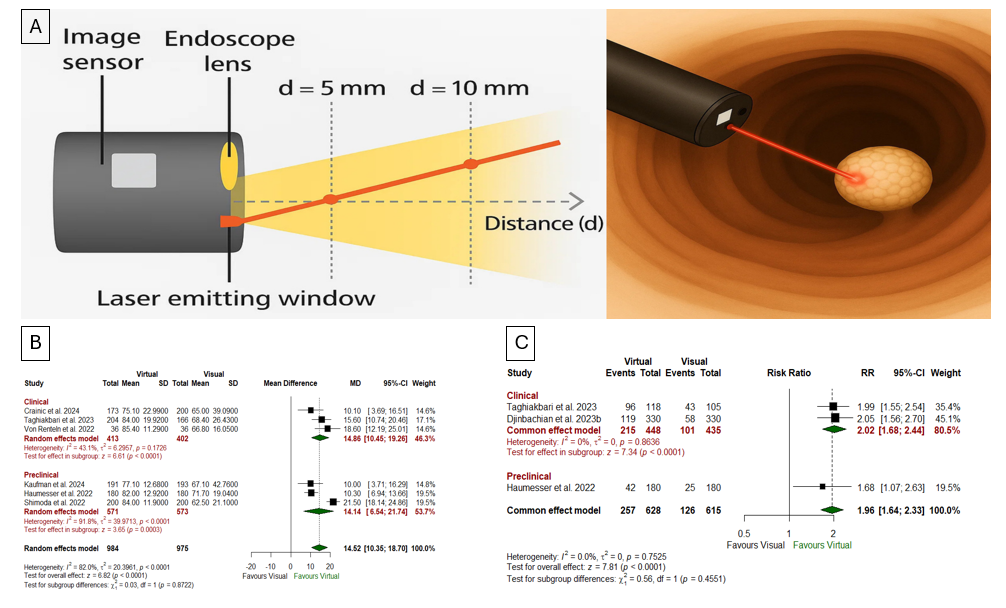
Figure: Figure 2. (A) Forest plot from the network meta-analysis showing the relative risk of underestimating polyp size >5 mm misclassified as 1–5 mm, with significantly higher misclassification observed in comparison to virtual assessment; (B) Network plot illustrating direct and indirect comparisons between virtual, visual, snare, and forceps modalities for polyps misclassified by size
Disclosures:
Mohamed S. Elgendy indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Mohamed Rifai indicated no relevant financial relationships.
Amira M. Taha indicated no relevant financial relationships.
Abdulrahman Maged indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Mohamed A. Elgamasy indicated no relevant financial relationships.
Mohamed Abuelazm indicated no relevant financial relationships.
Mina Fransawy Alkomos indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Mohamed S. Elgendy, MBBCh1, Islam Rajab, MD2, Mohamed Rifai, 3, Amira M. Taha, 4, Abdulrahman Maged, 5, Hosam I. Taha, MBBCh1, Mohamed A. Elgamasy, 5, Mohamed Abuelazm, 5, Mina Fransawy Alkomos, MD2, Walid Baddoura, MD2. P5134 - Accuracy of Virtual Scale Endoscopy in Colorectal Polyp Size Measurement: Pairwise and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Mohamed S. Elgendy, MBBCh1, Islam Rajab, MD2, Mohamed Rifai, 3, Amira M. Taha, 4, Abdulrahman Maged, 5, Hosam I. Taha, MBBCh1, Mohamed A. Elgamasy, 5, Mohamed Abuelazm, 5, Mina Fransawy Alkomos, MD2, Walid Baddoura, MD2
1Tanta University, Tanta, Al Gharbiyah, Egypt; 2St. Joseph's University Medical Center, Paterson, NJ; 3Faculty of Medicine, Menoufia university,Shebin El Kom,Egypt, Menoufia, Al Minufiyah, Egypt; 4Fayoum University, Faculty of Medicine, Fayoum, Al Fayyum, Egypt; 5Faculty of Medicine, Tanta University, Tanta, Egypt, Tanta, Al Gharbiyah, Egypt
Introduction: Colorectal cancer (CRC) is a leading cause of cancer death. Accurate in vivo polyp measurement is key for management, but visual assessment (VA) is often unreliable, correctly sizing only half and misclassifying up to one-third. Traditional tools like forceps and snares offer limited precision. Virtual Scale Endoscopy (VSE), a laser-calibrated overlay that adjusts for distance in real-time, shows promise for improving measurement accuracy without compromising efficiency
Methods: A pairwise meta-analysis comparing VSE to VA and a frequentist network meta-analysis (NMA) comparing VSE to VA, snare, and forceps were conducted from PubMed, Cochrane, WoS, Embase, and Scopus. Risk ratios (RR) were calculated for categorical outcomes and mean differences (MD) for continuous outcomes, each with a 95% confidence interval (CI). Intervention rankings were estimated with NMA by the Surface Under the Cumulative Ranking curve (SUCRA).
Results: Twelve studies were included, comprising 1,608 polyps from both clinical and preclinical trials, including 2,866 patients from seven clinical studies. In pairwise analysis, relative accuracy significantly improved with VSE compared to VA in both preclinical (MD 14.14, 95% CI: 6.54–21.74) and clinical settings (MD 14.86, 95% CI: 10.45–19.26). Correct size estimation also improved with VSE (RR 1.96, 95% CI: 1.64–2.33).
In the NMA, VSE reduced misclassification for polyps >5 mm (RR 3.51 vs. VA, 95% CI: 1.88–6.55; RR 3.26 vs. snare, 95% CI: 1.66–6.39), >10 mm (RR 2.08 vs. VA, 95% CI: 1.14–3.81), and >20 mm (RR 2.40 vs. VA, 95% CI: 1.30–4.46; RR 8.00 vs. forceps, 95% CI: 1.17–54.5). No significant differences were observed at size thresholds >3 mm, ≤5 mm, or ≤10 mm. Snare ranked highest for overestimation (SUCRA 69%), followed by VSE (63%), but differences were insignificant. Underestimation was lowest with VSE (SUCRA 80%), though differences from VA, snare, or forceps were insignificant. No significant differences were found for total misclassification (P= 0.438), overestimation (P= 0.617), or underestimation (P= 0.592).
Discussion: VSE significantly improved colorectal polyp size measurement accuracy compared to traditional VA. VSE also reduced measurement variability and misclassification compared to VA, snare, and forceps at clinically critical size thresholds. This can improve decision-making in polypectomy and surveillance, especially for diminutive and small polyps. However, larger multicenter randomized trials are needed to confirm these benefits.
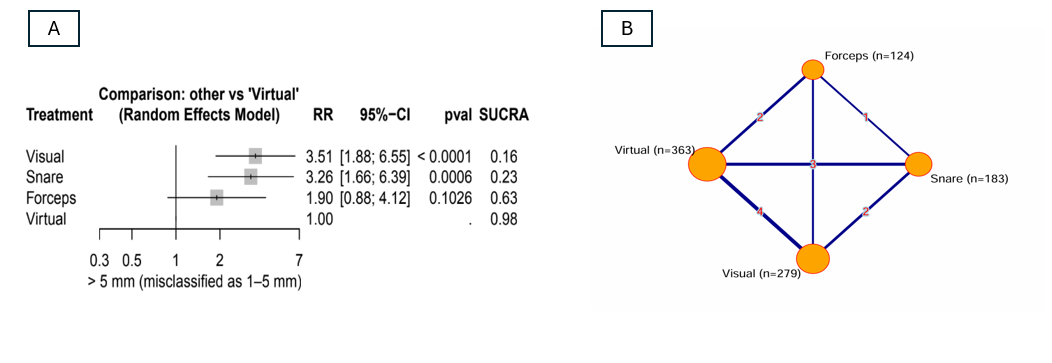
Figure: Figure 1 Shows (A) Laser-based sizing mechanism of Virtual Scale Endoscopy (VSE); (B) forest plots of total relative accuracy; and (C) forest plots of correct polyp size estimation comparing VSE to visual assessment in clinical and preclinical studies
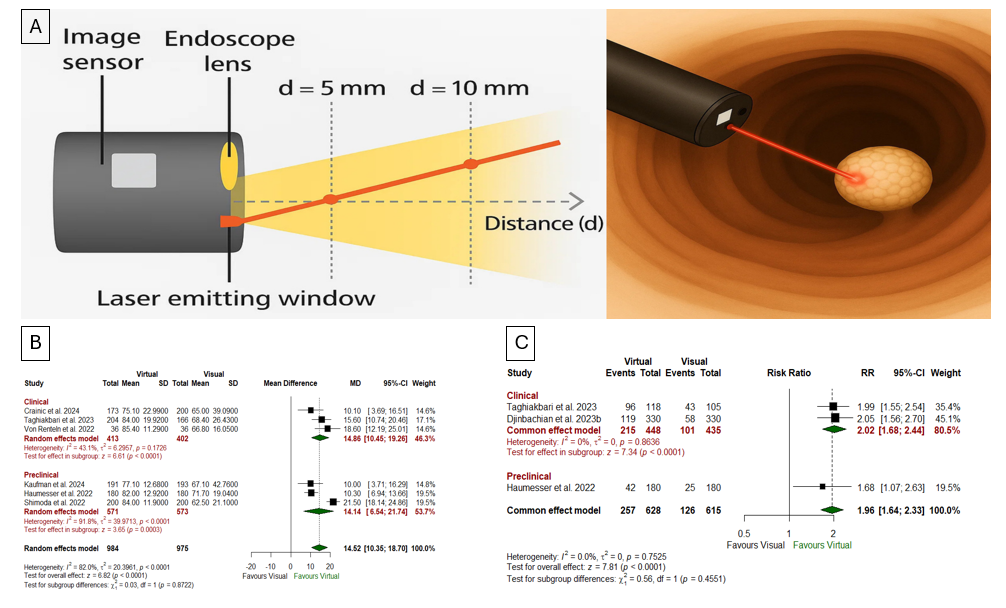
Figure: Figure 2. (A) Forest plot from the network meta-analysis showing the relative risk of underestimating polyp size >5 mm misclassified as 1–5 mm, with significantly higher misclassification observed in comparison to virtual assessment; (B) Network plot illustrating direct and indirect comparisons between virtual, visual, snare, and forceps modalities for polyps misclassified by size
Disclosures:
Mohamed S. Elgendy indicated no relevant financial relationships.
Islam Rajab indicated no relevant financial relationships.
Mohamed Rifai indicated no relevant financial relationships.
Amira M. Taha indicated no relevant financial relationships.
Abdulrahman Maged indicated no relevant financial relationships.
Hosam I. Taha indicated no relevant financial relationships.
Mohamed A. Elgamasy indicated no relevant financial relationships.
Mohamed Abuelazm indicated no relevant financial relationships.
Mina Fransawy Alkomos indicated no relevant financial relationships.
Walid Baddoura indicated no relevant financial relationships.
Mohamed S. Elgendy, MBBCh1, Islam Rajab, MD2, Mohamed Rifai, 3, Amira M. Taha, 4, Abdulrahman Maged, 5, Hosam I. Taha, MBBCh1, Mohamed A. Elgamasy, 5, Mohamed Abuelazm, 5, Mina Fransawy Alkomos, MD2, Walid Baddoura, MD2. P5134 - Accuracy of Virtual Scale Endoscopy in Colorectal Polyp Size Measurement: Pairwise and Network Meta-Analysis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

