Tuesday Poster Session
Category: General Endoscopy
P5132 - Association Between Preoperative Colonoscopy and Revision Risk in Primary Total Knee Arthroplasty: A Propensity-Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Suchapa Arayakarnkul, MD
University of Minnesota
Minneapolis, MN
Presenting Author(s)
Suchapa Arayakarnkul, MD1, Himsikhar Khataniar, MD2, Manal Asif, MD3, Rahul Karna, MD4, Mohammad Bilal, MD, FACG5
1University of Minnesota, Minneapolis, MN; 2Allegheny General Hospital, Pittsburgh, PA; 3Kabir Medical College, Peshawar, North-West Frontier, Pakistan; 4University of Minnesota Medical Center, Minneapolis, MN; 5University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Screening colonoscopy and total knee arthroplasty (TKA) are often performed in a similar age group. Colonoscopy can lead to transient bacteremia; and is hypothesized to seed prosthetic joints, leading to prosthetic joint infections (PJI). Prior literature is conflicting if colonoscopy-related transient bacteremia can lead to a significant risk of prosthesis failure. We aim to assess the relationship between preoperative colonoscopy, and the association with TKA outcomes.
Methods: A multi-institutional database TriNetX was utilized to assess patients undergoing TKA with a preceding colonoscopy from 2006 to 2025, using procedural terminology codes. Patients were categorized based on the number of days from colonoscopy to TKA with colonoscopy performed either < 1 or >1 year prior to TKA. Propensity-matched cohort analyses were performed after controlling for covariates including age, race, comorbidities, and risk factors for infection (diabetes, smoking, arthropathy, steroid use, HIV) to assess events including revision TKA, knee clean-out, PJI, osteomyelitis, cellulitis, sepsis, thromboembolic events, and mortality. Subgroup analysis was performed for patients with pre-operative colonoscopy within 3 months vs >1 year from TKA. Hazard ratio (HR) and 95% confidence intervals were reported; p-value< 0.05 were considered significant.
Results: We included a total of 12,892 patients who underwent colonoscopy < 1 year and 46,866 patients with colonoscopy >1 year prior to TKA. 12,881 patients were included in both groups after 1:1 propensity matching. There was no difference in revision TKA (HR 0.974 (0.901, 1.054), p=0.762) or knee clean-out (HR 0.706 (0.431, 1.156), p=0.611). Rates of infection (PJI (HR 1.178 (0.875, 1.586)), osteomyelitis (HR 0.771 (0.457, 1.302)), cellulitis (HR 1.018 (0.900, 1.151)), sepsis (HR 1.131 (0.920, 1.391)) were similar in both groups (all p >0.05). (Table 1) Additionally, there were no differences in rates of thromboembolic events or mortality. Subgroup analysis was performed for pre-operative colonoscopy within 3 months vs. >1 year. No significant differences in outcomes were observed. (Table 2)
Discussion: Preoperative colonoscopy prior to TKA was not associated with increased adverse outcomes including reoperation, infection, thromboembolic events, and mortality. Colonoscopy should not be withheld when clinically indicated.
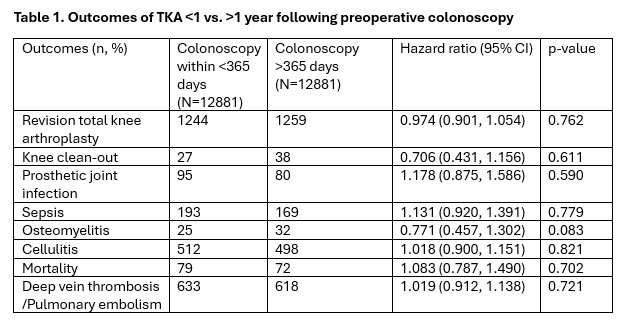
Figure: Table 1. Outcomes of TKA <1 vs. >1 year following preoperative colonoscopy
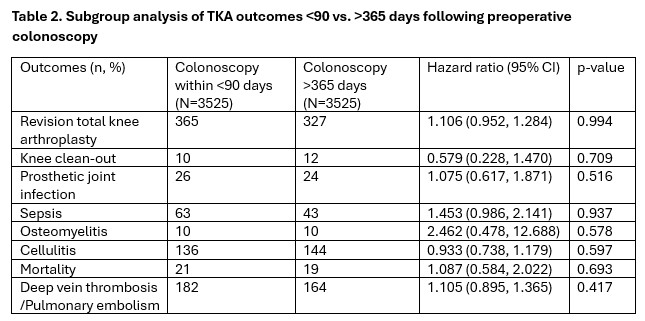
Figure: Table 2. Subgroup analysis of TKA outcomes <90 vs. >365 days following preoperative colonoscopy
Disclosures:
Suchapa Arayakarnkul indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Manal Asif indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Suchapa Arayakarnkul, MD1, Himsikhar Khataniar, MD2, Manal Asif, MD3, Rahul Karna, MD4, Mohammad Bilal, MD, FACG5. P5132 - Association Between Preoperative Colonoscopy and Revision Risk in Primary Total Knee Arthroplasty: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Minnesota, Minneapolis, MN; 2Allegheny General Hospital, Pittsburgh, PA; 3Kabir Medical College, Peshawar, North-West Frontier, Pakistan; 4University of Minnesota Medical Center, Minneapolis, MN; 5University of Colorado Anschutz Medical Campus, Denver, CO
Introduction: Screening colonoscopy and total knee arthroplasty (TKA) are often performed in a similar age group. Colonoscopy can lead to transient bacteremia; and is hypothesized to seed prosthetic joints, leading to prosthetic joint infections (PJI). Prior literature is conflicting if colonoscopy-related transient bacteremia can lead to a significant risk of prosthesis failure. We aim to assess the relationship between preoperative colonoscopy, and the association with TKA outcomes.
Methods: A multi-institutional database TriNetX was utilized to assess patients undergoing TKA with a preceding colonoscopy from 2006 to 2025, using procedural terminology codes. Patients were categorized based on the number of days from colonoscopy to TKA with colonoscopy performed either < 1 or >1 year prior to TKA. Propensity-matched cohort analyses were performed after controlling for covariates including age, race, comorbidities, and risk factors for infection (diabetes, smoking, arthropathy, steroid use, HIV) to assess events including revision TKA, knee clean-out, PJI, osteomyelitis, cellulitis, sepsis, thromboembolic events, and mortality. Subgroup analysis was performed for patients with pre-operative colonoscopy within 3 months vs >1 year from TKA. Hazard ratio (HR) and 95% confidence intervals were reported; p-value< 0.05 were considered significant.
Results: We included a total of 12,892 patients who underwent colonoscopy < 1 year and 46,866 patients with colonoscopy >1 year prior to TKA. 12,881 patients were included in both groups after 1:1 propensity matching. There was no difference in revision TKA (HR 0.974 (0.901, 1.054), p=0.762) or knee clean-out (HR 0.706 (0.431, 1.156), p=0.611). Rates of infection (PJI (HR 1.178 (0.875, 1.586)), osteomyelitis (HR 0.771 (0.457, 1.302)), cellulitis (HR 1.018 (0.900, 1.151)), sepsis (HR 1.131 (0.920, 1.391)) were similar in both groups (all p >0.05). (Table 1) Additionally, there were no differences in rates of thromboembolic events or mortality. Subgroup analysis was performed for pre-operative colonoscopy within 3 months vs. >1 year. No significant differences in outcomes were observed. (Table 2)
Discussion: Preoperative colonoscopy prior to TKA was not associated with increased adverse outcomes including reoperation, infection, thromboembolic events, and mortality. Colonoscopy should not be withheld when clinically indicated.
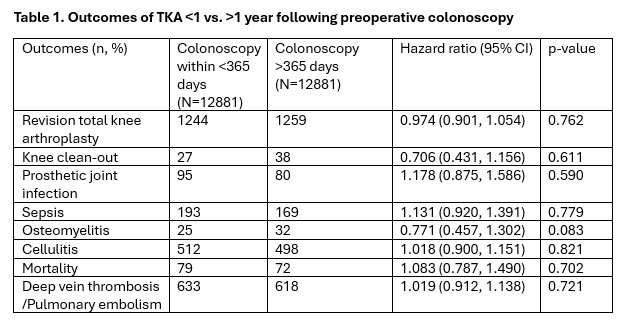
Figure: Table 1. Outcomes of TKA <1 vs. >1 year following preoperative colonoscopy
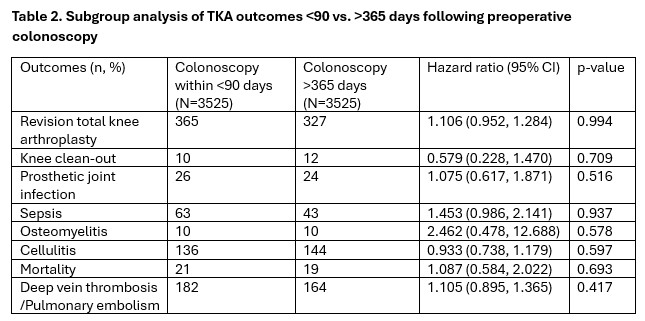
Figure: Table 2. Subgroup analysis of TKA outcomes <90 vs. >365 days following preoperative colonoscopy
Disclosures:
Suchapa Arayakarnkul indicated no relevant financial relationships.
Himsikhar Khataniar indicated no relevant financial relationships.
Manal Asif indicated no relevant financial relationships.
Rahul Karna indicated no relevant financial relationships.
Mohammad Bilal: Boston Scientific – Consultant. Cook endoscopy – Paid speaker. Steris Endoscopy – Consultant.
Suchapa Arayakarnkul, MD1, Himsikhar Khataniar, MD2, Manal Asif, MD3, Rahul Karna, MD4, Mohammad Bilal, MD, FACG5. P5132 - Association Between Preoperative Colonoscopy and Revision Risk in Primary Total Knee Arthroplasty: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

