Tuesday Poster Session
Category: Functional Bowel Disease
P5088 - Increased Incidence of Female-Predominant Gastrointestinal Conditions in Male-to-Female Transgender Individuals on Estrogen Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- KJ
Kate E. Johnson, BA (she/her/hers)
Weill Cornell Medical College
New York, NY
Presenting Author(s)
Kate E. Johnson, BA, Reem Z.. Sharaiha, MD, MSc
Weill Cornell Medical College, New York, NY
Introduction: Limited data exist on gastrointestinal health outcomes in transgender populations. This study aimed to evaluate the incidence of various GI conditions in male-to-female (MTF) transgender individuals on estrogen therapy compared to cisgender male controls.
Methods: This retrospective cohort study utilized the TriNetX Research Network, encompassing 103 healthcare organizations. We identified MTF transgender individuals with a diagnosis of transsexualism (ICD-10: F64.0), current estradiol therapy, and absence of testosterone therapy. The control group consisted of cisgender males. Propensity score matching (nearest neighbor, 0.1 caliper) was performed on 13 characteristics, including demographics, comorbidities, and BMI. We analyzed 7 GI outcomes with sufficient case numbers ( >10 cases per arm), focusing on conditions known to have female predominance, using risk analysis with 95% confidence intervals.
Results: We identified 19,420 MTF transgender individuals and 7,219,401 cisgender male controls, with propensity score matching yielding final cohorts of 18,833 patients each. MTF transgender cohort (mean age 34.0±14.3 years) had significantly increased risk for multiple female-predominant GI conditions compared to cisgender male controls. The most striking findings were observed in functional GI disorders: constipation occurred in 9.6% vs 5.9% (Risk Ratio [RR]: 1.61, 95% CI: 1.50-1.73, p< 0.001), irritable bowel syndrome in 2.7% vs 1.8% (RR: 1.55, 95% CI: 1.35-1.78, p< 0.001), and gastroparesis in 0.4% vs 0.2% (RR: 1.84, 95% CI: 1.24-2.73, p=0.002). Generalized abdominal pain (4.2% vs 3.2%, RR: 1.30, 95% CI: 1.17-1.44, p< 0.001), celiac disease (0.5% vs 0.3%, RR: 1.75, 95% CI: 1.27-2.41, p=0.001), and acute pancreatitis were also more frequently observed (0.6% vs 0.4%, RR: 1.63, 95% CI: 1.21-2.18, p=0.001). Functional dyspepsia showed a trend toward increased risk (0.8% vs 0.7%, RR: 1.25, 95% CI: 0.99-1.57, p=0.064) (Figure 1).
Discussion: Male-to-female transgender individuals on estrogen therapy demonstrate significantly increased rates of female-predominant GI conditions, particularly functional disorders including IBS, constipation, and gastroparesis. This pattern suggests estrogen therapy may contribute to developing GI symptom profiles typically seen in cisgender females, likely through hormonal effects on GI motility and visceral hypersensitivity. Healthcare providers should be alert of these patterns and consider early gastroenterology referral.
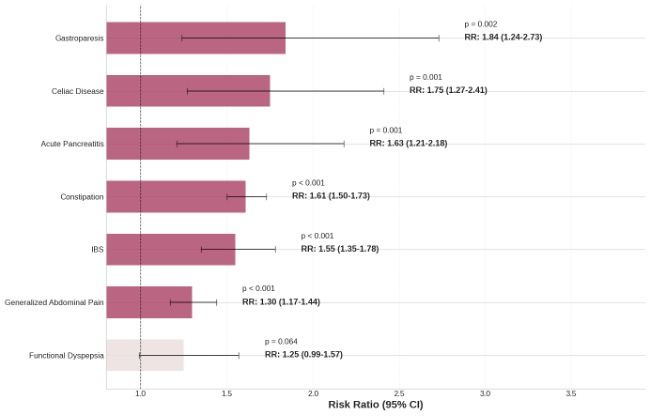
Figure: Figure 1. Risk of gastrointestinal conditions in male-to-female transgender individuals compared to cisgender male controls.
Disclosures:
Kate Johnson indicated no relevant financial relationships.
Reem Sharaiha: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus – Consultant. Surgical Intuitive – Consultant.
Kate E. Johnson, BA, Reem Z.. Sharaiha, MD, MSc. P5088 - Increased Incidence of Female-Predominant Gastrointestinal Conditions in Male-to-Female Transgender Individuals on Estrogen Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Weill Cornell Medical College, New York, NY
Introduction: Limited data exist on gastrointestinal health outcomes in transgender populations. This study aimed to evaluate the incidence of various GI conditions in male-to-female (MTF) transgender individuals on estrogen therapy compared to cisgender male controls.
Methods: This retrospective cohort study utilized the TriNetX Research Network, encompassing 103 healthcare organizations. We identified MTF transgender individuals with a diagnosis of transsexualism (ICD-10: F64.0), current estradiol therapy, and absence of testosterone therapy. The control group consisted of cisgender males. Propensity score matching (nearest neighbor, 0.1 caliper) was performed on 13 characteristics, including demographics, comorbidities, and BMI. We analyzed 7 GI outcomes with sufficient case numbers ( >10 cases per arm), focusing on conditions known to have female predominance, using risk analysis with 95% confidence intervals.
Results: We identified 19,420 MTF transgender individuals and 7,219,401 cisgender male controls, with propensity score matching yielding final cohorts of 18,833 patients each. MTF transgender cohort (mean age 34.0±14.3 years) had significantly increased risk for multiple female-predominant GI conditions compared to cisgender male controls. The most striking findings were observed in functional GI disorders: constipation occurred in 9.6% vs 5.9% (Risk Ratio [RR]: 1.61, 95% CI: 1.50-1.73, p< 0.001), irritable bowel syndrome in 2.7% vs 1.8% (RR: 1.55, 95% CI: 1.35-1.78, p< 0.001), and gastroparesis in 0.4% vs 0.2% (RR: 1.84, 95% CI: 1.24-2.73, p=0.002). Generalized abdominal pain (4.2% vs 3.2%, RR: 1.30, 95% CI: 1.17-1.44, p< 0.001), celiac disease (0.5% vs 0.3%, RR: 1.75, 95% CI: 1.27-2.41, p=0.001), and acute pancreatitis were also more frequently observed (0.6% vs 0.4%, RR: 1.63, 95% CI: 1.21-2.18, p=0.001). Functional dyspepsia showed a trend toward increased risk (0.8% vs 0.7%, RR: 1.25, 95% CI: 0.99-1.57, p=0.064) (Figure 1).
Discussion: Male-to-female transgender individuals on estrogen therapy demonstrate significantly increased rates of female-predominant GI conditions, particularly functional disorders including IBS, constipation, and gastroparesis. This pattern suggests estrogen therapy may contribute to developing GI symptom profiles typically seen in cisgender females, likely through hormonal effects on GI motility and visceral hypersensitivity. Healthcare providers should be alert of these patterns and consider early gastroenterology referral.
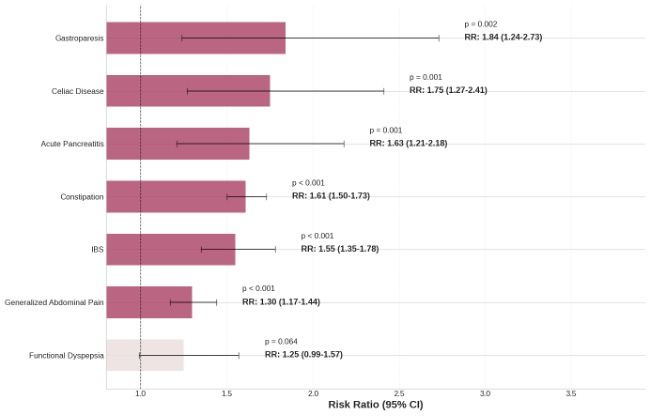
Figure: Figure 1. Risk of gastrointestinal conditions in male-to-female transgender individuals compared to cisgender male controls.
Disclosures:
Kate Johnson indicated no relevant financial relationships.
Reem Sharaiha: Boston Scientific – Consultant. Cook Medical – Consultant. Olympus – Consultant. Surgical Intuitive – Consultant.
Kate E. Johnson, BA, Reem Z.. Sharaiha, MD, MSc. P5088 - Increased Incidence of Female-Predominant Gastrointestinal Conditions in Male-to-Female Transgender Individuals on Estrogen Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.

