Tuesday Poster Session
Category: Functional Bowel Disease
P5080 - Comparative Analysis of Medication Use and Healthcare Utilization in Gastroparesis and Functional Dyspepsia: A Propensity-Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sameer Rao, MBBS
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Allegheny Health Network, Pittsburgh, PA; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Gastroparesis (GP) and functional dyspepsia (FD) often have overlapping upper gastrointestinal symptoms; however may differ in therapeutic approaches and healthcare utilization. We aimed to compare medication usage and healthcare utilization between these two populations in a national cohort.
Methods: We conducted a retrospective cohort study using the TriNetX database, identifying attributes using ICD-10, CPT, and RxNorm codes. Patients with structural gastric or small bowel abnormalities were excluded. GP was defined by diagnosis within 3 months of a gastric emptying study and typical symptoms 3–12 months prior. FD required a diagnosis with prior upper endoscopy (1–12 months) and symptoms 6–12 months before diagnosis. Patients with overlapping GP/FD diagnoses were excluded. The primary outcome was medication use; secondary outcomes included healthcare utilization. Propensity score matching (1:1) adjusted for demographics and comorbidities. Relative risks (RRs) with 95% confidence intervals (CIs) were calculated, with P< .05 considered significant.
Results: We identified 7,329 patients with GP (mean age 47.1±17.6 years; 72.7% female) and 3,950 with FD (mean age 44.7±20.3 years; 69.2% female). After 1:1 matching, 3,420 patients per group were followed for 5 years. GP patients had significantly higher use of metoclopramide (RR 3.4, 95% CI 3.02–3.84, P-value< .0001), erythromycin (RR 2.7, 95% CI 2.24–2.92, P-value< .0001), and antiemetics including ondansetron, promethazine, prochlorperazine, and diphenhydramine (all P-value< .0001). In contrast, tricyclic antidepressants (TCAs) were used less frequently in GP (RR 0.7, 95% CI 0.66–0.82, P-value< .0001), with only a minimal difference in proton pump inhibitor (PPI) use (RR 0.95, 95% CI 0.91–0.99, P-value=.03). GP was also with higher rates of upper endoscopy (RR 1.2, 95% CI 1.07–1.30, P-value=.001), emergency department visits (RR 1.2, 95% CI 1.08–1.22, P-value< .0001), hospitalizations (RR 1.5, 95% CI 1.33–1.62, P-value< .0001), and all-cause mortality (RR 1.5, 95% CI 1.18–1.92, P-value=.001), but lower use of computed tomography scans of the abdomen (RR 0.7, 95% CI 0.55–0.93, P-value=.01).
Discussion: GP and FD patients show high overall use of gastrointestinal and psychotropic medications. GP is more often associated with reliance on prokinetics, antiemetics, and greater healthcare utilization, whereas FD is more commonly linked to tricyclic antidepressant use. These patterns reflect differing management and shared clinical complexity.
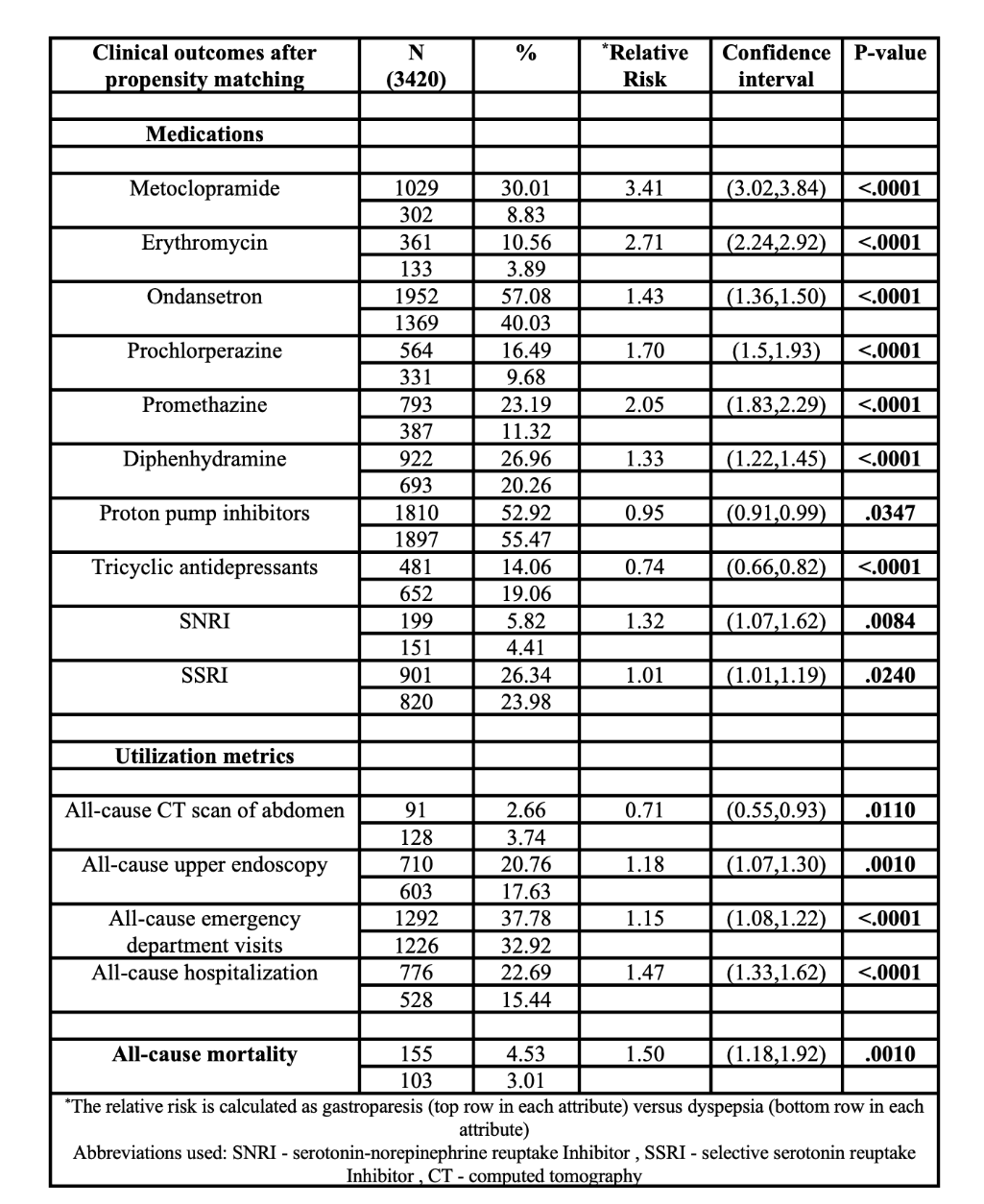
Figure: Table - Comparison of medication use, healthcare utilization, and mortality between gastroparesis and functional dyspepsia
Disclosures:
Sameer Rao indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Manas Gunani indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1. P5080 - Comparative Analysis of Medication Use and Healthcare Utilization in Gastroparesis and Functional Dyspepsia: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Allegheny Health Network, Pittsburgh, PA; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Gastroparesis (GP) and functional dyspepsia (FD) often have overlapping upper gastrointestinal symptoms; however may differ in therapeutic approaches and healthcare utilization. We aimed to compare medication usage and healthcare utilization between these two populations in a national cohort.
Methods: We conducted a retrospective cohort study using the TriNetX database, identifying attributes using ICD-10, CPT, and RxNorm codes. Patients with structural gastric or small bowel abnormalities were excluded. GP was defined by diagnosis within 3 months of a gastric emptying study and typical symptoms 3–12 months prior. FD required a diagnosis with prior upper endoscopy (1–12 months) and symptoms 6–12 months before diagnosis. Patients with overlapping GP/FD diagnoses were excluded. The primary outcome was medication use; secondary outcomes included healthcare utilization. Propensity score matching (1:1) adjusted for demographics and comorbidities. Relative risks (RRs) with 95% confidence intervals (CIs) were calculated, with P< .05 considered significant.
Results: We identified 7,329 patients with GP (mean age 47.1±17.6 years; 72.7% female) and 3,950 with FD (mean age 44.7±20.3 years; 69.2% female). After 1:1 matching, 3,420 patients per group were followed for 5 years. GP patients had significantly higher use of metoclopramide (RR 3.4, 95% CI 3.02–3.84, P-value< .0001), erythromycin (RR 2.7, 95% CI 2.24–2.92, P-value< .0001), and antiemetics including ondansetron, promethazine, prochlorperazine, and diphenhydramine (all P-value< .0001). In contrast, tricyclic antidepressants (TCAs) were used less frequently in GP (RR 0.7, 95% CI 0.66–0.82, P-value< .0001), with only a minimal difference in proton pump inhibitor (PPI) use (RR 0.95, 95% CI 0.91–0.99, P-value=.03). GP was also with higher rates of upper endoscopy (RR 1.2, 95% CI 1.07–1.30, P-value=.001), emergency department visits (RR 1.2, 95% CI 1.08–1.22, P-value< .0001), hospitalizations (RR 1.5, 95% CI 1.33–1.62, P-value< .0001), and all-cause mortality (RR 1.5, 95% CI 1.18–1.92, P-value=.001), but lower use of computed tomography scans of the abdomen (RR 0.7, 95% CI 0.55–0.93, P-value=.01).
Discussion: GP and FD patients show high overall use of gastrointestinal and psychotropic medications. GP is more often associated with reliance on prokinetics, antiemetics, and greater healthcare utilization, whereas FD is more commonly linked to tricyclic antidepressant use. These patterns reflect differing management and shared clinical complexity.
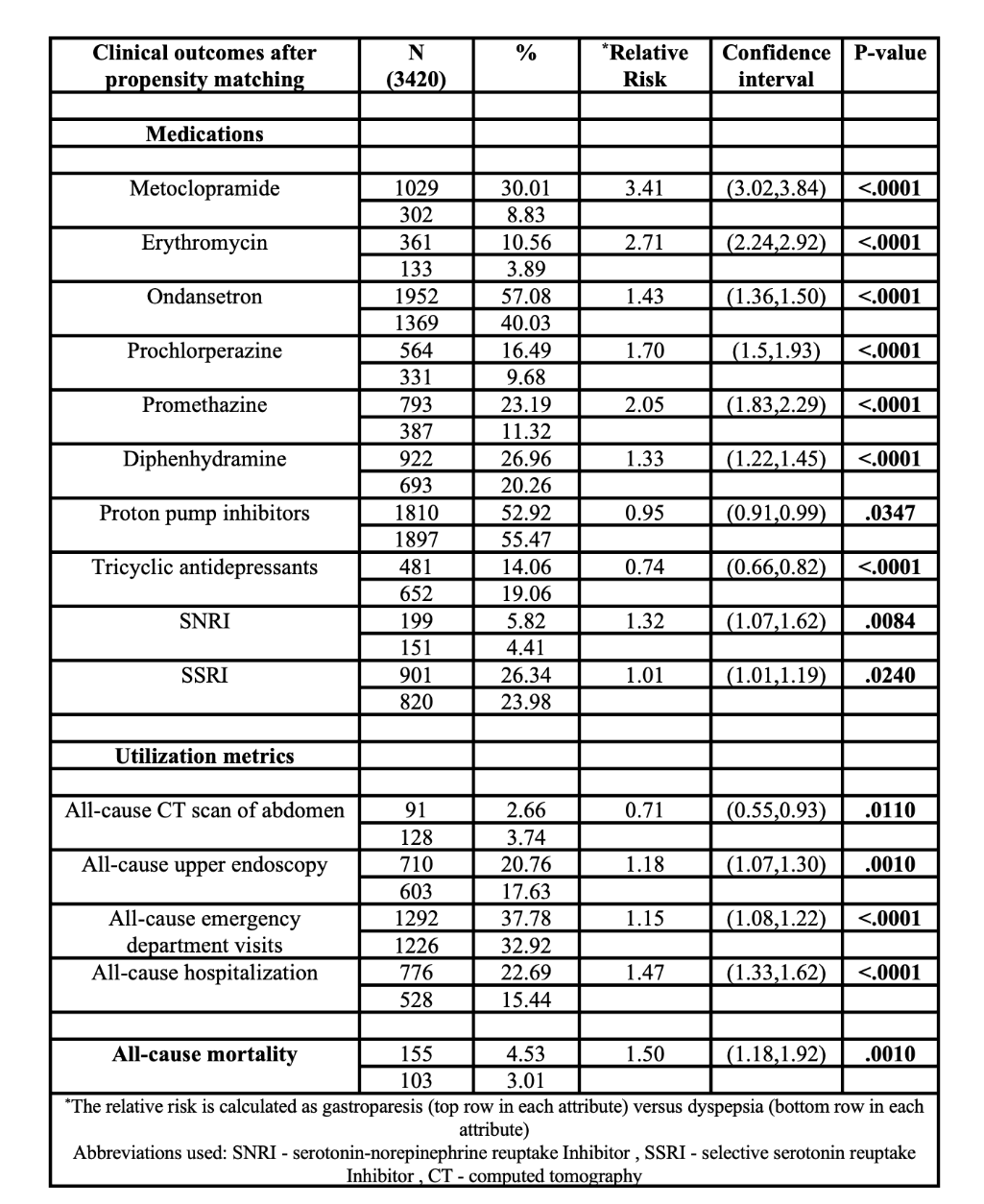
Figure: Table - Comparison of medication use, healthcare utilization, and mortality between gastroparesis and functional dyspepsia
Disclosures:
Sameer Rao indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Manas Gunani indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1. P5080 - Comparative Analysis of Medication Use and Healthcare Utilization in Gastroparesis and Functional Dyspepsia: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
