Tuesday Poster Session
Category: Functional Bowel Disease
P5079 - Clinical Symptom Burden and Overlapping Disorders of Gut–Brain Interaction in Gastroparesis vs Functional Dyspepsia: A Propensity-Matched Cohort Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
.jpg)
Sameer Rao, MBBS
Rutgers New Jersey Medical School
Newark, NJ
Presenting Author(s)
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1
1Rutgers New Jersey Medical School, Newark, NJ; 2Allegheny Health Network, Pittsburgh, PA; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Gastroparesis (GP) and functional dyspepsia (FD) are chronic gastrointestinal (GI) disorders with overlapping symptoms. GP typically presents with nausea, vomiting, and early satiety, while FD is more often linked to epigastric pain. Whether they are distinct conditions, or a spectrum remains debated. We looked at population-level comparison of symptom profiles and co-existing gut–brain interaction disorders.
Methods: We conducted a retrospective cohort study using the TriNetX database, identifying attributes using ICD-10, CPT, and RxNorm codes. Patients with structural gastric or small bowel abnormalities were excluded. GP was defined by diagnosis within 3 months of a gastric emptying study and typical symptoms 3–12 months prior. FD required a diagnosis with prior upper endoscopy (1–12 months) and symptoms 6–12 months before diagnosis. Patients with overlapping GP/FD diagnoses were excluded. Primary outcomes were clinical symptoms; secondary outcomes included co-existing gut–brain interaction disorders. Propensity score matching (1:1) adjusted for demographics and comorbidities. Relative risks (RRs) and 95% CIs were calculated, with P< .05 considered significant.
Results: Our study included 7,329 patients with GP (mean age 47.1±17.6 years; 72.7% female) and 3,950 with FD (mean age 44.7±20.3 years; 69.2% female). After 1:1 propensity score matching, 3,420 patients per group were followed for 5 years. Compared to FD, GP patients had greater burden of nausea (RR 1.4, 95% CI 1.28–1.51, P-value< .0001), vomiting (RR 1.9, 95% CI 1.66–2.18, P-value< .0001), anorexia (RR 1.3, 95% CI 1.03–1.67, P-value=.03), early satiety (RR 1.3, 95% CI 1.03–1.66, P-value=.03), abdominal distension (RR 1.3, 95% CI 1.13–1.37, P-value< .0001), malnutrition (RR 2.8, 95% CI 2.23–3.42, P-value< .0001), and weight loss (RR 1.3, 95% CI 1.15–1.53, P-value< .0001). Epigastric pain was less common in GP (RR 0.6, 95% CI 0.54–0.63, P-value< .0001). GP was also linked to higher rates of chronic idiopathic constipation (RR 1.7, 95% CI 1.30–2.10, P-value< .0001) and slow transit constipation (RR 1.5, 95% CI 1.17–1.87, P-value=.0011), but lower rates of IBS (RR 0.7, 95% CI 0.64–0.77, P-value< .0001).
Discussion: In this large-scale database study comparing GP and FD, substantial symptom overlap was observed; however, GP was more strongly associated with motility-related symptoms, nutritional complications, and constipation, while FD more commonly with epigastric pain and IBS.
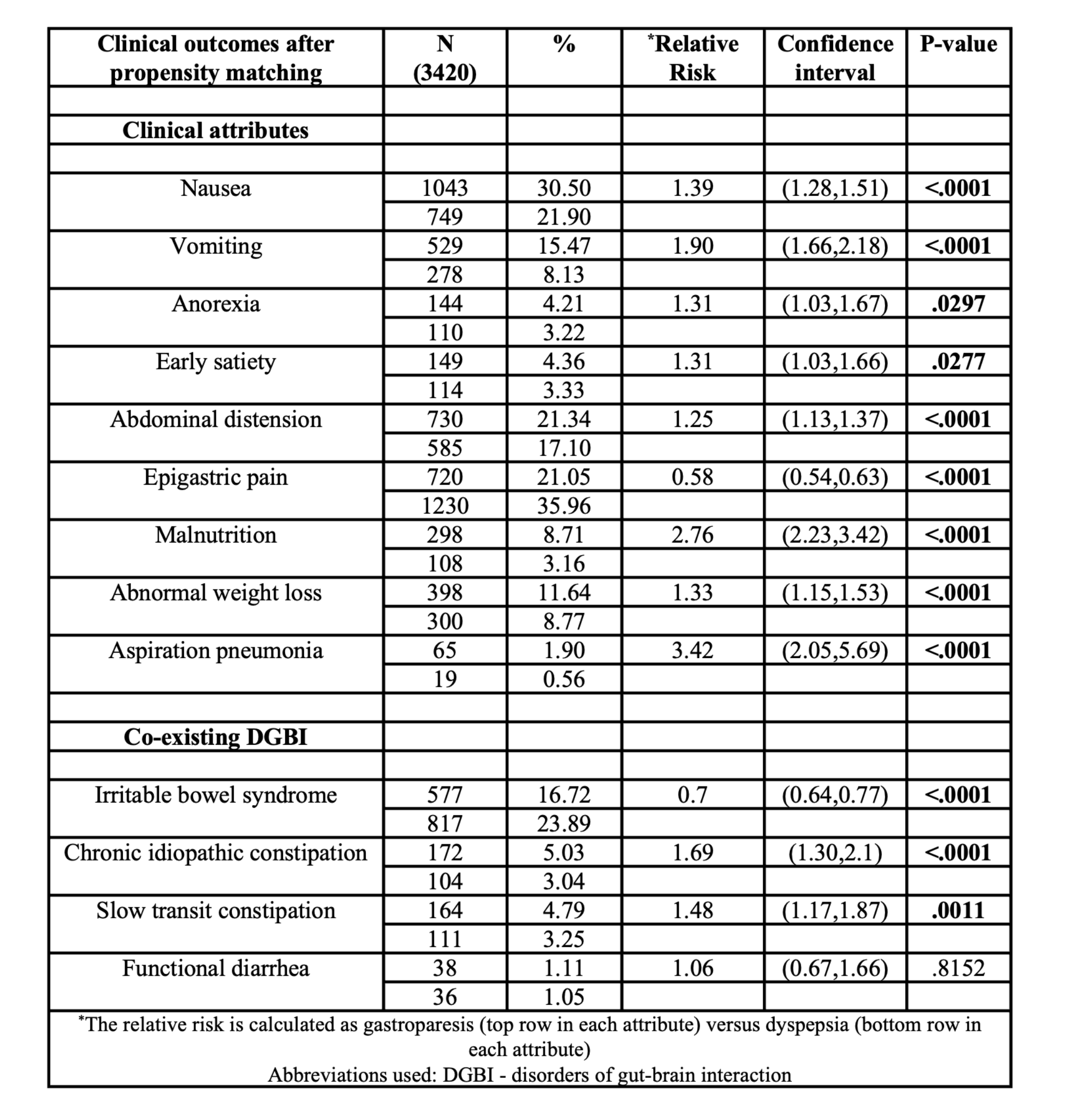
Figure: Table – Comparison of symptomatology and co-existing disorders of gut–brain interaction between patients with gastroparesis and functional dyspepsia
Disclosures:
Sameer Rao indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Manas Gunani indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1. P5079 - Clinical Symptom Burden and Overlapping Disorders of Gut–Brain Interaction in Gastroparesis vs Functional Dyspepsia: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Rutgers New Jersey Medical School, Newark, NJ; 2Allegheny Health Network, Pittsburgh, PA; 3Texas Tech University Health Sciences Center, Odessa, TX; 4Lenox Hill Hospital, Northwell Health, New York, NY
Introduction: Gastroparesis (GP) and functional dyspepsia (FD) are chronic gastrointestinal (GI) disorders with overlapping symptoms. GP typically presents with nausea, vomiting, and early satiety, while FD is more often linked to epigastric pain. Whether they are distinct conditions, or a spectrum remains debated. We looked at population-level comparison of symptom profiles and co-existing gut–brain interaction disorders.
Methods: We conducted a retrospective cohort study using the TriNetX database, identifying attributes using ICD-10, CPT, and RxNorm codes. Patients with structural gastric or small bowel abnormalities were excluded. GP was defined by diagnosis within 3 months of a gastric emptying study and typical symptoms 3–12 months prior. FD required a diagnosis with prior upper endoscopy (1–12 months) and symptoms 6–12 months before diagnosis. Patients with overlapping GP/FD diagnoses were excluded. Primary outcomes were clinical symptoms; secondary outcomes included co-existing gut–brain interaction disorders. Propensity score matching (1:1) adjusted for demographics and comorbidities. Relative risks (RRs) and 95% CIs were calculated, with P< .05 considered significant.
Results: Our study included 7,329 patients with GP (mean age 47.1±17.6 years; 72.7% female) and 3,950 with FD (mean age 44.7±20.3 years; 69.2% female). After 1:1 propensity score matching, 3,420 patients per group were followed for 5 years. Compared to FD, GP patients had greater burden of nausea (RR 1.4, 95% CI 1.28–1.51, P-value< .0001), vomiting (RR 1.9, 95% CI 1.66–2.18, P-value< .0001), anorexia (RR 1.3, 95% CI 1.03–1.67, P-value=.03), early satiety (RR 1.3, 95% CI 1.03–1.66, P-value=.03), abdominal distension (RR 1.3, 95% CI 1.13–1.37, P-value< .0001), malnutrition (RR 2.8, 95% CI 2.23–3.42, P-value< .0001), and weight loss (RR 1.3, 95% CI 1.15–1.53, P-value< .0001). Epigastric pain was less common in GP (RR 0.6, 95% CI 0.54–0.63, P-value< .0001). GP was also linked to higher rates of chronic idiopathic constipation (RR 1.7, 95% CI 1.30–2.10, P-value< .0001) and slow transit constipation (RR 1.5, 95% CI 1.17–1.87, P-value=.0011), but lower rates of IBS (RR 0.7, 95% CI 0.64–0.77, P-value< .0001).
Discussion: In this large-scale database study comparing GP and FD, substantial symptom overlap was observed; however, GP was more strongly associated with motility-related symptoms, nutritional complications, and constipation, while FD more commonly with epigastric pain and IBS.
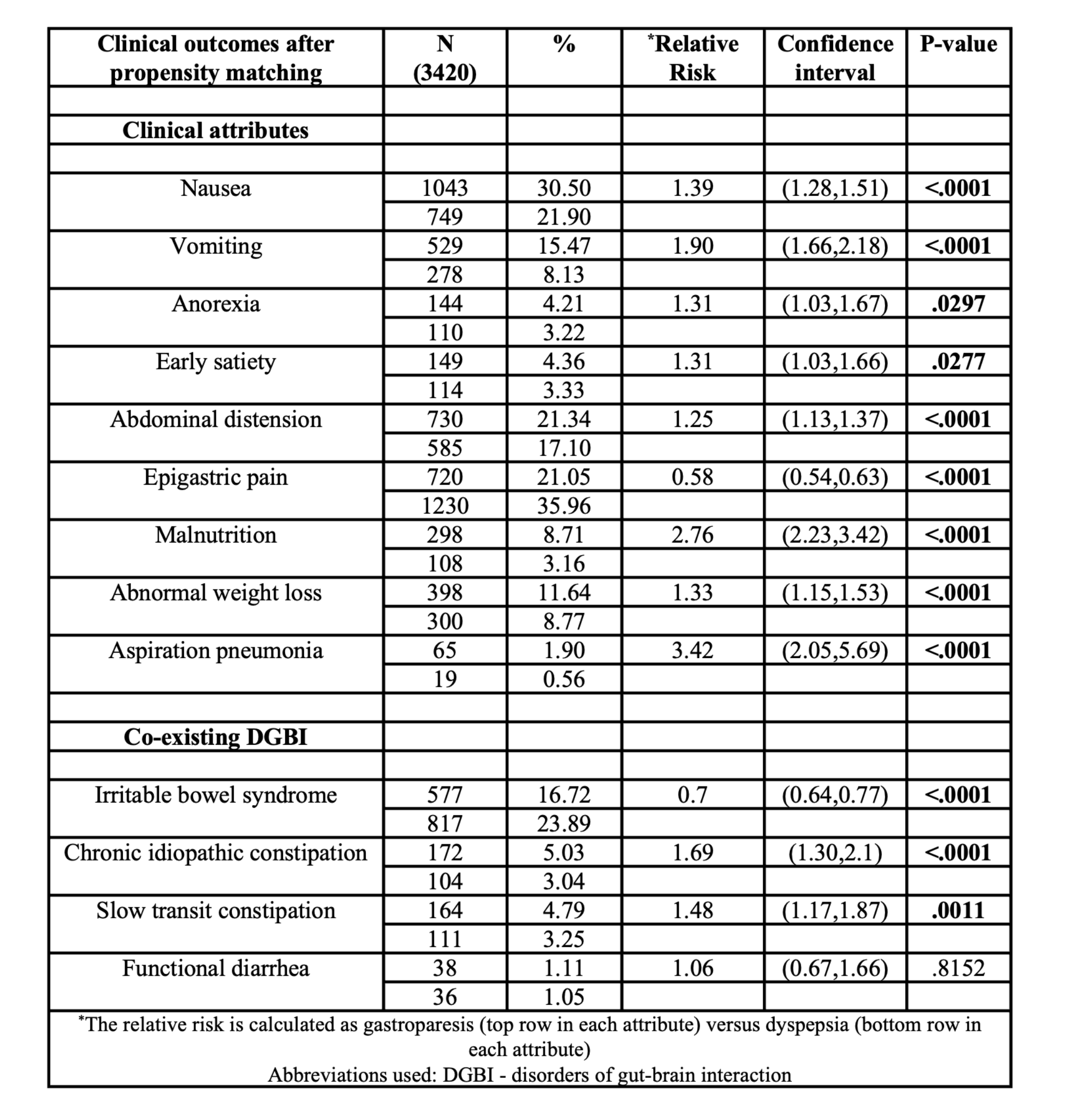
Figure: Table – Comparison of symptomatology and co-existing disorders of gut–brain interaction between patients with gastroparesis and functional dyspepsia
Disclosures:
Sameer Rao indicated no relevant financial relationships.
Ritik M. Goyal indicated no relevant financial relationships.
Manas Gunani indicated no relevant financial relationships.
Anjul Verma indicated no relevant financial relationships.
Rohan Karkra indicated no relevant financial relationships.
Menna-Allah Elaskandrany indicated no relevant financial relationships.
Amanda Rupert indicated no relevant financial relationships.
Ahmed Al-Khazraji indicated no relevant financial relationships.
Sameer Rao, MBBS1, Ritik M. Goyal, MBBS1, Manas Gunani, MBBS2, Anjul Verma, MD3, Rohan Karkra, MBBS1, Menna-Allah Elaskandrany, DO4, Amanda A. Rupert, MD1, Ahmed Al-Khazraji, MD1. P5079 - Clinical Symptom Burden and Overlapping Disorders of Gut–Brain Interaction in Gastroparesis vs Functional Dyspepsia: A Propensity-Matched Cohort Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
