Tuesday Poster Session
Category: Functional Bowel Disease
P5067 - Rates of IBS Are Higher in Gender Minority Patients Than Cisgender Patients, Especially Those Taking Gender Affirming Hormone Therapy
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Holly Greenwald, MD (she/her/hers)
Temple University Hospital
Philadelphia, PA
Presenting Author(s)
Tess Petersen, MD1, Michael Behanan, MD2, Manasa Devi. Vallabhaneni, MD3, Aaron Balinski, MD3, Zachary Wilmer Reichenbach, MD, PhD3, Brenda Horwitz, MD3, Adam C.. Ehrlich, MD, MPH3, Holly Greenwald, MD3
1Temple Univeristy hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3Temple University Hospital, Philadelphia, PA
Introduction: Gender minority patients (GMP) are considered a health disparity population by the National Institute on Minority Health and Health Disparities. GMP, including transgender, nonbinary, and genderqueer patients, are grossly underrepresented in gastrointestinal research. Our urban, tertiary care, academic center is a national leader in GMP care. This study aimed to compare the incidence of irritable bowel syndrome (IBS) and gastro-esophageal reflux disease (GERD) in GMP and cis gender patients (CGP), and to explore the association of gender affirming hormone therapy on rates of IBS and GERD in GMP.
Methods: All patients who were seen at any outpatient practice at our institution between 09/2018-09/2022 and had gender identity information in the electronic health record were included in this retrospective cohort study. Patients with incomplete gender identity demographic information were excluded. GMP were defined as those whose sex assigned at birth or legal sex was different from gender identity. CGP were defined as those whose sex assigned at birth or legal sex was the same as gender identity. Patients with IBS were determined by ICD-10 code. Patients with GERD were determined by ICD-10 code or if patients were prescribed proton pump inhibitors or Histamine-2 receptor blockers.
Results: This study included 4995 patients (688 GMP, 4307 CGP). Demographic characteristics are described in Table 1. In a univariate analysis GMP had higher prevalence of IBS (2.6%) than CGP patients (1.2%) [RR 2.2, 95% CI 1.3-3.8, P=0.004]. In a multivariate analysis controlled for age and race, GMP had significantly higher prevalence of IBS than CGP [RR 2.4, 95% CI 1.2-4.6, P= 0.010]. Conversely, when controlled for age and race, GMP had a lower prevalence of GERD than CGP [RR 0.54, 95% CI 0.18-0.29, P< 0.001]. Gender affirming hormone therapies in the GMP are described in Table 2. GMP taking gender affirming hormone therapy had significantly higher prevalence of IBS than GMP not on hormone therapy [RR 5.5, 95% CI 1.3-24, P= 0.024]. When controlling for age and race, gender affirming hormone therapy did not increase risk of GERD [95% CI 0.8-2.3, P=0.192].
Discussion: In summary, GMP were found to have higher prevalence of IBS, especially when using gender affirming hormone therapy, but lower rates of GERD than CGP after controlling for age and race. These data may be explained by the minority stress model which hypothesizes that GMP experience higher rates of social stress.
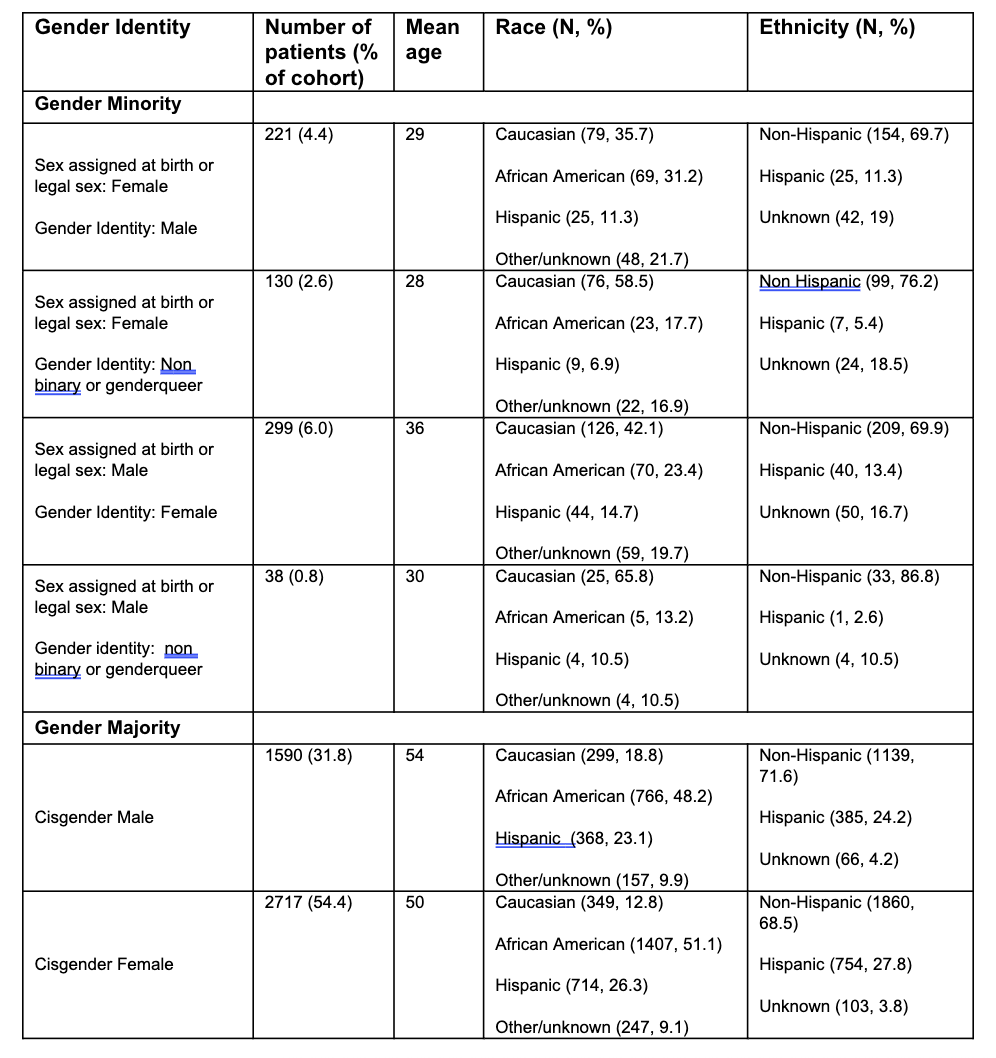
Figure: Table 1. Patient demographics
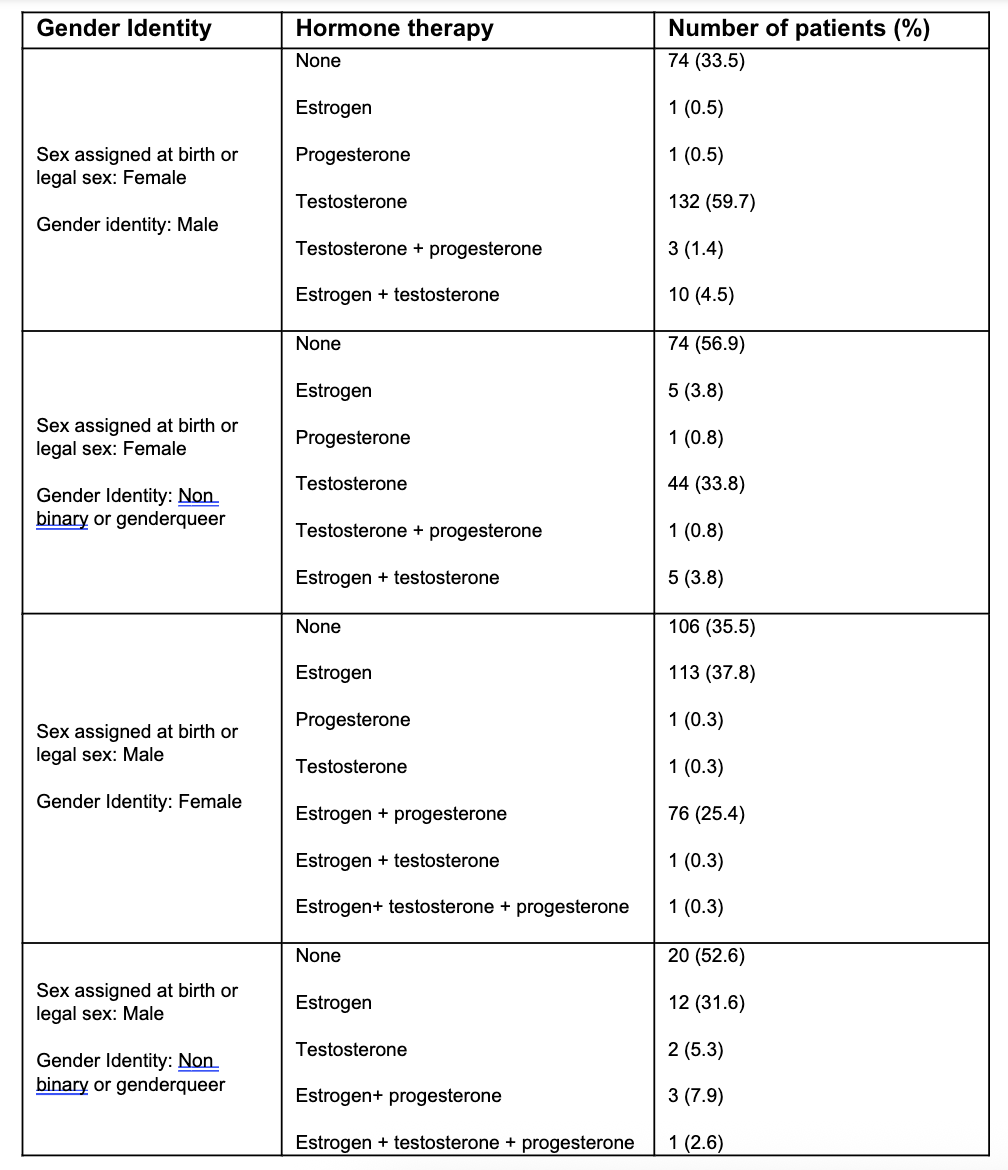
Figure: Table 2. Gender affirming hormone medications in gender minority patients
Disclosures:
Tess Petersen indicated no relevant financial relationships.
Michael Behanan indicated no relevant financial relationships.
Manasa Vallabhaneni indicated no relevant financial relationships.
Aaron Balinski indicated no relevant financial relationships.
Zachary Wilmer Reichenbach indicated no relevant financial relationships.
Brenda Horwitz indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Consultant, Speakers Bureau. Bristol Meyers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Guardant – Advisory Committee/Board Member. J&J – Consultant.
Holly Greenwald indicated no relevant financial relationships.
Tess Petersen, MD1, Michael Behanan, MD2, Manasa Devi. Vallabhaneni, MD3, Aaron Balinski, MD3, Zachary Wilmer Reichenbach, MD, PhD3, Brenda Horwitz, MD3, Adam C.. Ehrlich, MD, MPH3, Holly Greenwald, MD3. P5067 - Rates of IBS Are Higher in Gender Minority Patients Than Cisgender Patients, Especially Those Taking Gender Affirming Hormone Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Temple Univeristy hospital, Philadelphia, PA; 2Lewis Katz School of Medicine at Temple University, Philadelphia, PA; 3Temple University Hospital, Philadelphia, PA
Introduction: Gender minority patients (GMP) are considered a health disparity population by the National Institute on Minority Health and Health Disparities. GMP, including transgender, nonbinary, and genderqueer patients, are grossly underrepresented in gastrointestinal research. Our urban, tertiary care, academic center is a national leader in GMP care. This study aimed to compare the incidence of irritable bowel syndrome (IBS) and gastro-esophageal reflux disease (GERD) in GMP and cis gender patients (CGP), and to explore the association of gender affirming hormone therapy on rates of IBS and GERD in GMP.
Methods: All patients who were seen at any outpatient practice at our institution between 09/2018-09/2022 and had gender identity information in the electronic health record were included in this retrospective cohort study. Patients with incomplete gender identity demographic information were excluded. GMP were defined as those whose sex assigned at birth or legal sex was different from gender identity. CGP were defined as those whose sex assigned at birth or legal sex was the same as gender identity. Patients with IBS were determined by ICD-10 code. Patients with GERD were determined by ICD-10 code or if patients were prescribed proton pump inhibitors or Histamine-2 receptor blockers.
Results: This study included 4995 patients (688 GMP, 4307 CGP). Demographic characteristics are described in Table 1. In a univariate analysis GMP had higher prevalence of IBS (2.6%) than CGP patients (1.2%) [RR 2.2, 95% CI 1.3-3.8, P=0.004]. In a multivariate analysis controlled for age and race, GMP had significantly higher prevalence of IBS than CGP [RR 2.4, 95% CI 1.2-4.6, P= 0.010]. Conversely, when controlled for age and race, GMP had a lower prevalence of GERD than CGP [RR 0.54, 95% CI 0.18-0.29, P< 0.001]. Gender affirming hormone therapies in the GMP are described in Table 2. GMP taking gender affirming hormone therapy had significantly higher prevalence of IBS than GMP not on hormone therapy [RR 5.5, 95% CI 1.3-24, P= 0.024]. When controlling for age and race, gender affirming hormone therapy did not increase risk of GERD [95% CI 0.8-2.3, P=0.192].
Discussion: In summary, GMP were found to have higher prevalence of IBS, especially when using gender affirming hormone therapy, but lower rates of GERD than CGP after controlling for age and race. These data may be explained by the minority stress model which hypothesizes that GMP experience higher rates of social stress.
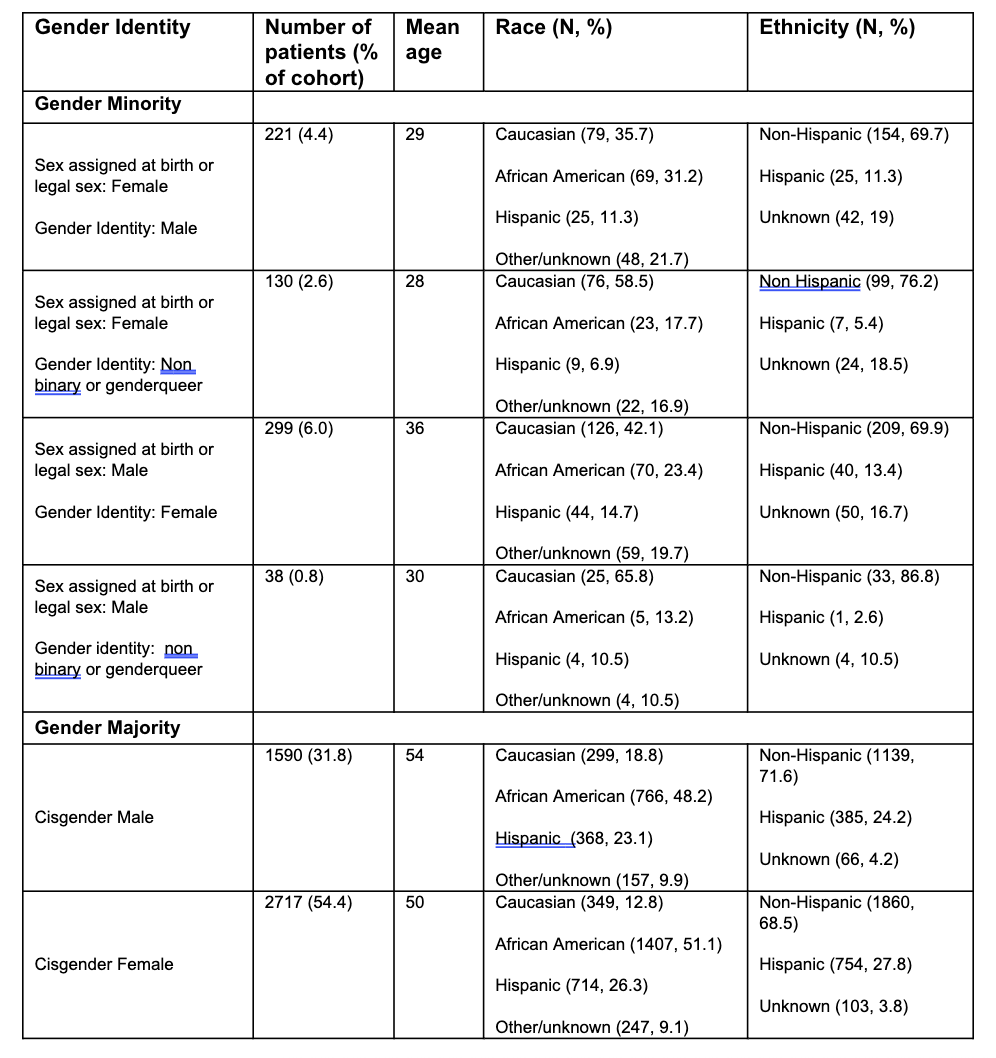
Figure: Table 1. Patient demographics
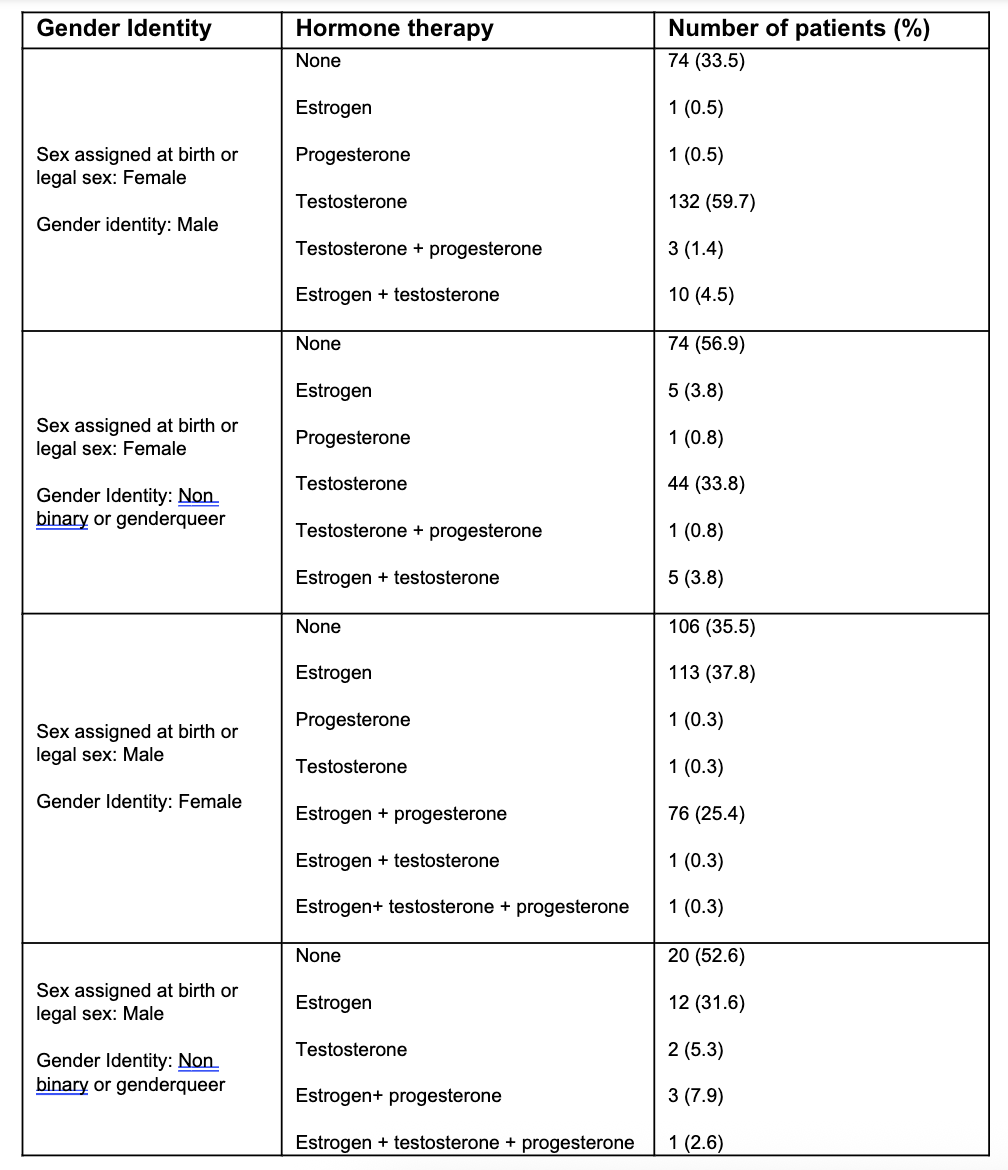
Figure: Table 2. Gender affirming hormone medications in gender minority patients
Disclosures:
Tess Petersen indicated no relevant financial relationships.
Michael Behanan indicated no relevant financial relationships.
Manasa Vallabhaneni indicated no relevant financial relationships.
Aaron Balinski indicated no relevant financial relationships.
Zachary Wilmer Reichenbach indicated no relevant financial relationships.
Brenda Horwitz indicated no relevant financial relationships.
Adam Ehrlich: Abbvie – Consultant, Speakers Bureau. Bristol Meyers Squibb – Advisory Committee/Board Member, Speakers Bureau. Eli Lilly – Advisory Committee/Board Member, Speakers Bureau. Guardant – Advisory Committee/Board Member. J&J – Consultant.
Holly Greenwald indicated no relevant financial relationships.
Tess Petersen, MD1, Michael Behanan, MD2, Manasa Devi. Vallabhaneni, MD3, Aaron Balinski, MD3, Zachary Wilmer Reichenbach, MD, PhD3, Brenda Horwitz, MD3, Adam C.. Ehrlich, MD, MPH3, Holly Greenwald, MD3. P5067 - Rates of IBS Are Higher in Gender Minority Patients Than Cisgender Patients, Especially Those Taking Gender Affirming Hormone Therapy, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
