Tuesday Poster Session
Category: Functional Bowel Disease
P5059 - Potential Utility of the Point of Care Bowel Sound Analysis for Asymptomatic Patients With and Without IBS: Pilot Study
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MB
Michael J. Barbarito
Endologic LLC
Fairfield, NJ
Presenting Author(s)
Michael J.. Barbarito, 1, Zamir S. Brelvi, MD, PhD2, Shiv D. Patel, BS3, Zahf Shaikh, DO4, Shawn Z. Brelvi, BSc5, Neel Godbole, 6, Julia Matalon, 7, Sourav Dutta, MD, MBA8, Sachin Mysore, BA9
1Endologic LLC, Fairfield, NJ; 2Hackensack Meridian Health/EndoLogic, Montville, NJ; 3Endologic LLC, Parsippany-Troy Hills, NJ; 4Hackensack Meridian Health, Randolph, NJ; 5Endologic LLC, Montville, NJ; 6Endologic LLC, Parsippany, NJ; 7Endologic, Montville, NJ; 8Endologic, Franklin Lakes, NJ; 9Endologic, Edison, NJ
Introduction: Irritable Bowel Syndrome (IBS) is often associated with small intestinal bacterial overgrowth (SIBO), related to altered bacterial density, motility, and enteric nervous system activity. However, SIBO-like symptoms can also arise from other conditions like infectious enteritis, IBD, celiac disease, and pancreatic insufficiency. The Gastrointestinal Symptom Rating Scale (GSRS) is a validated subjective tool for measuring IBS symptoms. This study explores the use of point-of-care bowel sound analysis (BSA) as a non-invasive, objective correlate to GSRS, building on prior work validating BSA in IBS and SIBO. We assess whether BSA can evaluate intestinal health in asymptomatic patients with and without IBS.
Methods: This cross-sectional diagnostic study enrolled asymptomatic males and females aged 18–80, with and without IBS (GSRS< 35). Excluded were those with abdominal surgery or IBD. Bowel sounds were recorded from 3 umbilical points (left, right, inferior) for 15 seconds each using electronic stethoscopes and a phone microphone. Audio files were analyzed using a proprietary algorithm referencing prior SIBO data to generate a BSA score. Scores < 5 were considered healthy, 6–25 borderline, and >25 unhealthy. Stool tests were used to evaluate correlations between BSA scores and fecal calprotectin levels ( >50 μg/g)
Results: 32 patients met criteria. Among non-IBS patients (n=14), 8 had BSA ≥5; 4 of these had abnormal stool tests. In the IBS group (n=18), 14 had BSA ≥5; 10 had normal stool tests. Non-IBS patients with BSA >5 had mean calprotectin of 93.04 μg/g vs. 10.2 μg/g for BSA < 5 (p=0.085). IBS patients with high BSA had a mean of 57.39 μg/g vs. 18.35 μg/g for low BSA (p=0.031), Fig. 1. Power simulation showed both trends could reach significance (p< 0.05) in future studies with ~30–40 patients per group. These results suggest BSA correlates with inflammation in patients deemed asymptomatic by GSRS. Fig. 2
Discussion: Point-of-care BSA may offer a non-invasive, objective measure of intestinal health in patients without overt symptoms. In non-IBS individuals, elevated BSA scores were associated with abnormal stool tests, suggesting potential for detecting occult pathology missed by subjective screening. In IBS patients, elevated BSA with normal stool tests aligns with literature positioning BSA as a marker of symptom severity. Larger studies are warranted to validate these findings and support the use of BSA as both a screening tool for non-IBS patients and a monitoring tool for IBS.
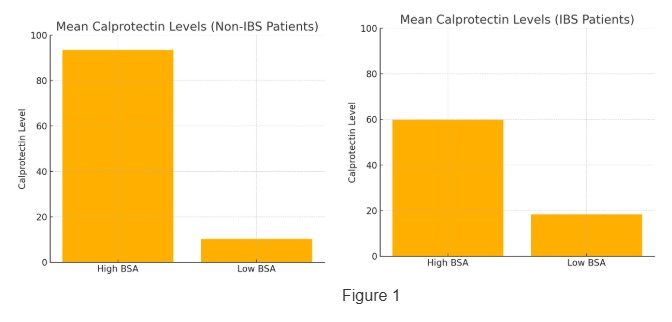
Figure: Mean Calprotectin Level in Low vs High BSA for Non-IBS and IBS Patients
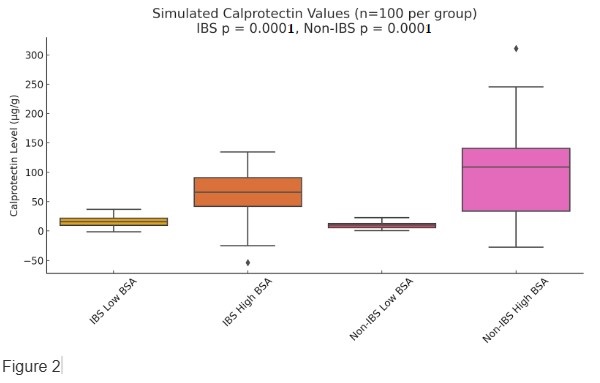
Figure: Projected Mean Calprotectin Level in Low vs High BSA for Non-IBS and IBS Patients
Disclosures:
Michael Barbarito indicated no relevant financial relationships.
Zamir Brelvi indicated no relevant financial relationships.
Shiv Patel indicated no relevant financial relationships.
Zahf Shaikh indicated no relevant financial relationships.
Shawn Brelvi indicated no relevant financial relationships.
Neel Godbole indicated no relevant financial relationships.
Julia Matalon indicated no relevant financial relationships.
Sourav Dutta indicated no relevant financial relationships.
Sachin Mysore indicated no relevant financial relationships.
Michael J.. Barbarito, 1, Zamir S. Brelvi, MD, PhD2, Shiv D. Patel, BS3, Zahf Shaikh, DO4, Shawn Z. Brelvi, BSc5, Neel Godbole, 6, Julia Matalon, 7, Sourav Dutta, MD, MBA8, Sachin Mysore, BA9. P5059 - Potential Utility of the Point of Care Bowel Sound Analysis for Asymptomatic Patients With and Without IBS: Pilot Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Endologic LLC, Fairfield, NJ; 2Hackensack Meridian Health/EndoLogic, Montville, NJ; 3Endologic LLC, Parsippany-Troy Hills, NJ; 4Hackensack Meridian Health, Randolph, NJ; 5Endologic LLC, Montville, NJ; 6Endologic LLC, Parsippany, NJ; 7Endologic, Montville, NJ; 8Endologic, Franklin Lakes, NJ; 9Endologic, Edison, NJ
Introduction: Irritable Bowel Syndrome (IBS) is often associated with small intestinal bacterial overgrowth (SIBO), related to altered bacterial density, motility, and enteric nervous system activity. However, SIBO-like symptoms can also arise from other conditions like infectious enteritis, IBD, celiac disease, and pancreatic insufficiency. The Gastrointestinal Symptom Rating Scale (GSRS) is a validated subjective tool for measuring IBS symptoms. This study explores the use of point-of-care bowel sound analysis (BSA) as a non-invasive, objective correlate to GSRS, building on prior work validating BSA in IBS and SIBO. We assess whether BSA can evaluate intestinal health in asymptomatic patients with and without IBS.
Methods: This cross-sectional diagnostic study enrolled asymptomatic males and females aged 18–80, with and without IBS (GSRS< 35). Excluded were those with abdominal surgery or IBD. Bowel sounds were recorded from 3 umbilical points (left, right, inferior) for 15 seconds each using electronic stethoscopes and a phone microphone. Audio files were analyzed using a proprietary algorithm referencing prior SIBO data to generate a BSA score. Scores < 5 were considered healthy, 6–25 borderline, and >25 unhealthy. Stool tests were used to evaluate correlations between BSA scores and fecal calprotectin levels ( >50 μg/g)
Results: 32 patients met criteria. Among non-IBS patients (n=14), 8 had BSA ≥5; 4 of these had abnormal stool tests. In the IBS group (n=18), 14 had BSA ≥5; 10 had normal stool tests. Non-IBS patients with BSA >5 had mean calprotectin of 93.04 μg/g vs. 10.2 μg/g for BSA < 5 (p=0.085). IBS patients with high BSA had a mean of 57.39 μg/g vs. 18.35 μg/g for low BSA (p=0.031), Fig. 1. Power simulation showed both trends could reach significance (p< 0.05) in future studies with ~30–40 patients per group. These results suggest BSA correlates with inflammation in patients deemed asymptomatic by GSRS. Fig. 2
Discussion: Point-of-care BSA may offer a non-invasive, objective measure of intestinal health in patients without overt symptoms. In non-IBS individuals, elevated BSA scores were associated with abnormal stool tests, suggesting potential for detecting occult pathology missed by subjective screening. In IBS patients, elevated BSA with normal stool tests aligns with literature positioning BSA as a marker of symptom severity. Larger studies are warranted to validate these findings and support the use of BSA as both a screening tool for non-IBS patients and a monitoring tool for IBS.
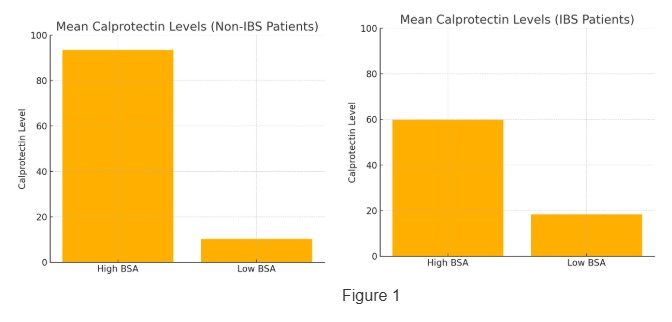
Figure: Mean Calprotectin Level in Low vs High BSA for Non-IBS and IBS Patients
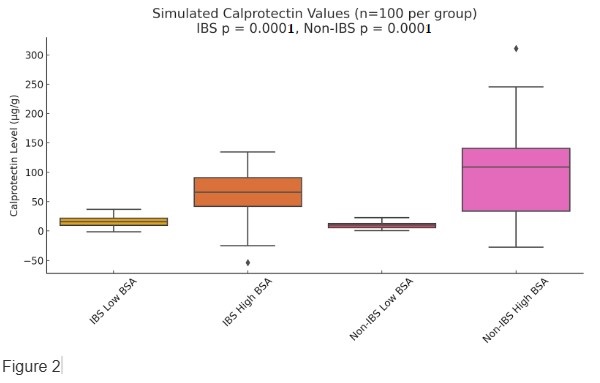
Figure: Projected Mean Calprotectin Level in Low vs High BSA for Non-IBS and IBS Patients
Disclosures:
Michael Barbarito indicated no relevant financial relationships.
Zamir Brelvi indicated no relevant financial relationships.
Shiv Patel indicated no relevant financial relationships.
Zahf Shaikh indicated no relevant financial relationships.
Shawn Brelvi indicated no relevant financial relationships.
Neel Godbole indicated no relevant financial relationships.
Julia Matalon indicated no relevant financial relationships.
Sourav Dutta indicated no relevant financial relationships.
Sachin Mysore indicated no relevant financial relationships.
Michael J.. Barbarito, 1, Zamir S. Brelvi, MD, PhD2, Shiv D. Patel, BS3, Zahf Shaikh, DO4, Shawn Z. Brelvi, BSc5, Neel Godbole, 6, Julia Matalon, 7, Sourav Dutta, MD, MBA8, Sachin Mysore, BA9. P5059 - Potential Utility of the Point of Care Bowel Sound Analysis for Asymptomatic Patients With and Without IBS: Pilot Study, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
