Tuesday Poster Session
Category: Esophagus
P5057 - Unveiling a Rare Coexistence: Achalasia Associated with Distal Esophageal and Gastric Diverticula – A Case Series
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Swati Mahapatra, DO (she/her/hers)
Texas A&M
El Paso, TX
Presenting Author(s)
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD3, Richard McCallum, MD, FACG3
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Texas A&M, El Paso, TX; 3Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Achalasia is an esophageal motor disorder marked by incomplete lower esophageal sphincter relaxation and impaired peristalsis, leading to esophageal dilation. Gastroesophageal conditions coexist in 3%–7% of cases and may mimic achalasia (pseudoachalasia), be unrelated (e.g., hiatal hernia, gastric volvulus), or related (e.g., esophageal diverticulum). Distal esophageal diverticulum (ED) is often linked to motility disorders, with achalasia present in over 60% of cases. In contrast, gastric diverticula (GD) are rare, with an incidence of 0.03%–0.3%, and their coexistence with achalasia is undocumented. We present two rare cases of achalasia with concurrent ED and GD.
Case Description/
Methods: Case 1: A 49-year-old male with a history of GERD presented with one year of progressive dysphagia to solids and liquids. High-resolution esophageal manometry and barium swallow confirmed type I achalasia with complete aperistalsis. Esophagogastroduodenoscopy (EGD) with functional lumen imaging probe (FLIP) demonstrated a markedly dilated esophagus and a medium-sized GD located in the gastric fundus. The patient underwent successful 30 mm balloon dilation of the gastroesophageal junction (GEJ) under fluoroscopic guidance. Post-dilation FLIP showed improved GEJ distensibility with a maximum diameter of 16 mm. The patient was discharged with scheduled outpatient follow-up.
Case 2: A 90-year-old female with Sjögren’s syndrome and hypertension presented with a 10-week history of dysphagia to solids and liquids. Manometry and barium swallow confirmed type I achalasia with aperistalsis. EGD with FLIP evaluation identified a mid-esophageal diverticulum along with two distal esophageal diverticula. The patient underwent 30 mm balloon dilation of the GEJ under fluoroscopic guidance. Post-procedure FLIP revealed enhanced distensibility with a maximal diameter of 30 mm. She was discharged with outpatient gastroenterology follow-up.
Discussion: This case series reports two rare cases of achalasia coexisting with esophageal and gastric diverticula, a previously undocumented association. Advanced diagnostics, including FLIP, and targeted interventions like balloon dilation, proved effective in managing these complex presentations. These findings highlight the importance of recognizing atypical anatomical anomalies in achalasia for optimal patient care.
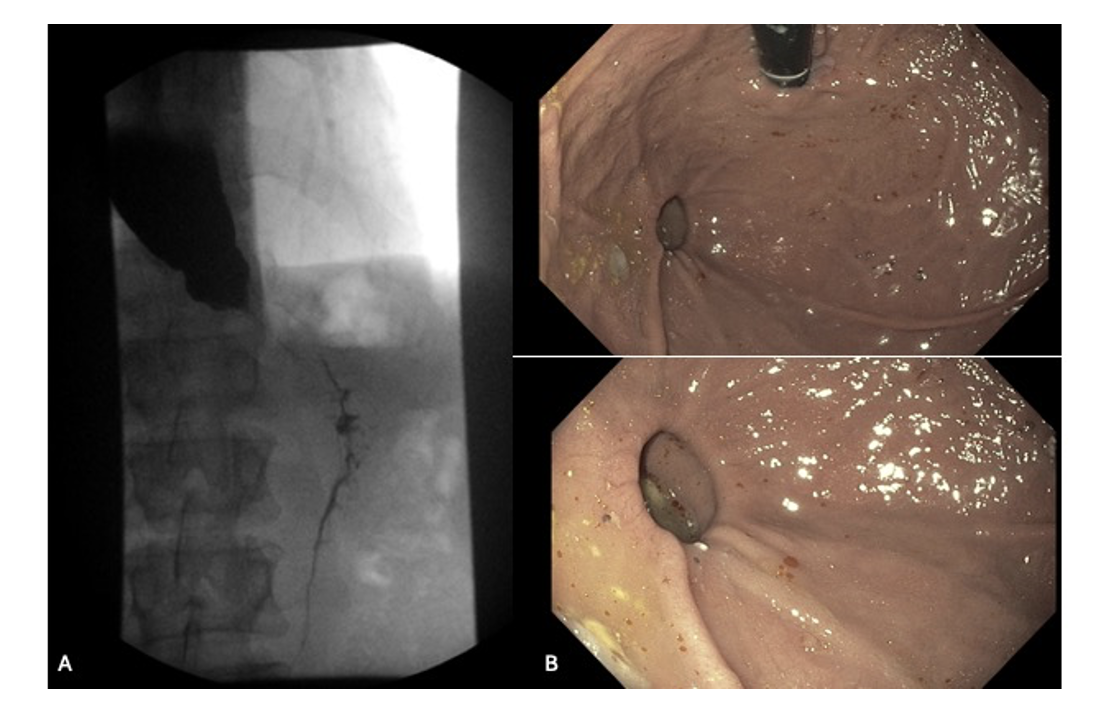
Figure: Figure 1A. Barium swallow showing mildly dilated esophagus with decreased esophageal motility, confirming achalasia type 1. Figure 1B. EGD findings showing medium-sized gastric diverticulum in the gastric fundus for case 1.
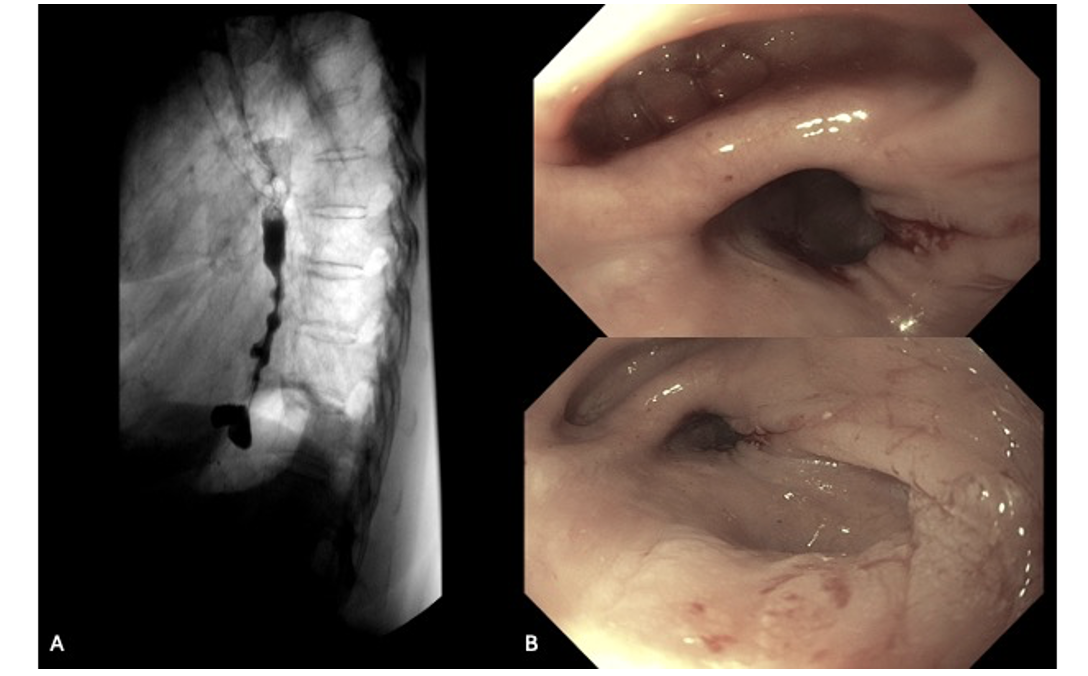
Figure: Figure 2A. Barium swallow confirming achalasia type 1. Figure 2B. EGD findings showing two diverticula in the distal esophagus for case 2.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Richard McCallum indicated no relevant financial relationships.
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD3, Richard McCallum, MD, FACG3. P5057 - Unveiling a Rare Coexistence: Achalasia Associated with Distal Esophageal and Gastric Diverticula – A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Department of Internal Medicine at Paul L. Foster School of Medicine, Texas Tech University Health Sciences Center, El Paso TX, USA, El Paso, TX; 2Texas A&M, El Paso, TX; 3Texas Tech University Health Sciences Center, El Paso, TX
Introduction: Achalasia is an esophageal motor disorder marked by incomplete lower esophageal sphincter relaxation and impaired peristalsis, leading to esophageal dilation. Gastroesophageal conditions coexist in 3%–7% of cases and may mimic achalasia (pseudoachalasia), be unrelated (e.g., hiatal hernia, gastric volvulus), or related (e.g., esophageal diverticulum). Distal esophageal diverticulum (ED) is often linked to motility disorders, with achalasia present in over 60% of cases. In contrast, gastric diverticula (GD) are rare, with an incidence of 0.03%–0.3%, and their coexistence with achalasia is undocumented. We present two rare cases of achalasia with concurrent ED and GD.
Case Description/
Methods: Case 1: A 49-year-old male with a history of GERD presented with one year of progressive dysphagia to solids and liquids. High-resolution esophageal manometry and barium swallow confirmed type I achalasia with complete aperistalsis. Esophagogastroduodenoscopy (EGD) with functional lumen imaging probe (FLIP) demonstrated a markedly dilated esophagus and a medium-sized GD located in the gastric fundus. The patient underwent successful 30 mm balloon dilation of the gastroesophageal junction (GEJ) under fluoroscopic guidance. Post-dilation FLIP showed improved GEJ distensibility with a maximum diameter of 16 mm. The patient was discharged with scheduled outpatient follow-up.
Case 2: A 90-year-old female with Sjögren’s syndrome and hypertension presented with a 10-week history of dysphagia to solids and liquids. Manometry and barium swallow confirmed type I achalasia with aperistalsis. EGD with FLIP evaluation identified a mid-esophageal diverticulum along with two distal esophageal diverticula. The patient underwent 30 mm balloon dilation of the GEJ under fluoroscopic guidance. Post-procedure FLIP revealed enhanced distensibility with a maximal diameter of 30 mm. She was discharged with outpatient gastroenterology follow-up.
Discussion: This case series reports two rare cases of achalasia coexisting with esophageal and gastric diverticula, a previously undocumented association. Advanced diagnostics, including FLIP, and targeted interventions like balloon dilation, proved effective in managing these complex presentations. These findings highlight the importance of recognizing atypical anatomical anomalies in achalasia for optimal patient care.
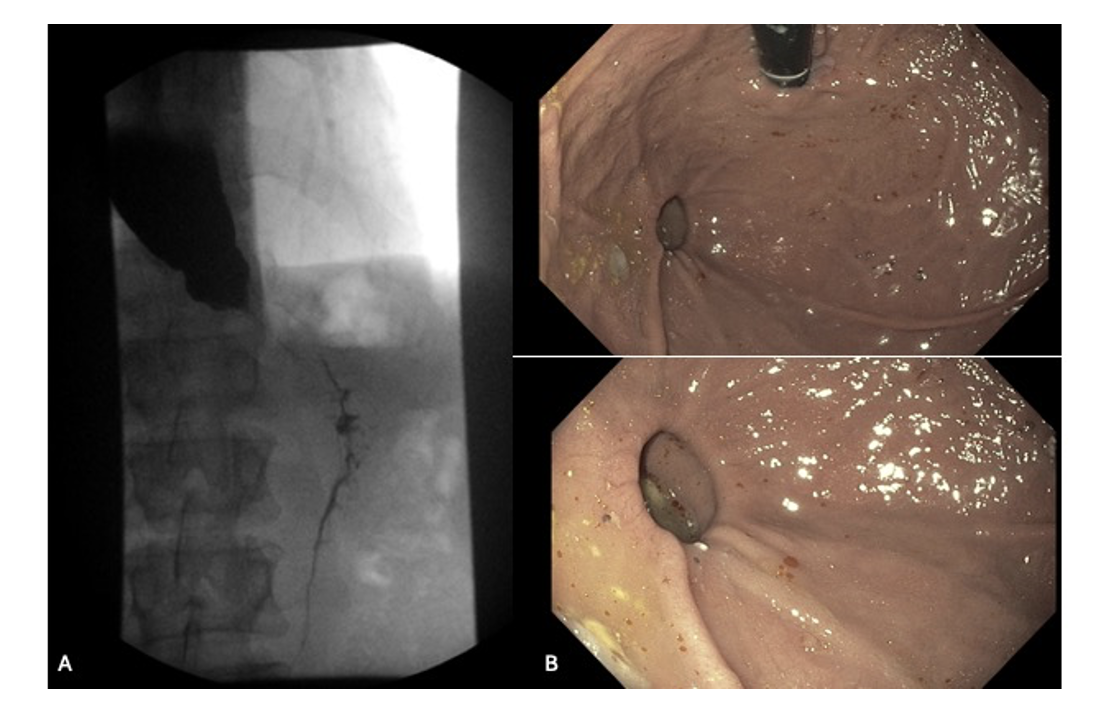
Figure: Figure 1A. Barium swallow showing mildly dilated esophagus with decreased esophageal motility, confirming achalasia type 1. Figure 1B. EGD findings showing medium-sized gastric diverticulum in the gastric fundus for case 1.
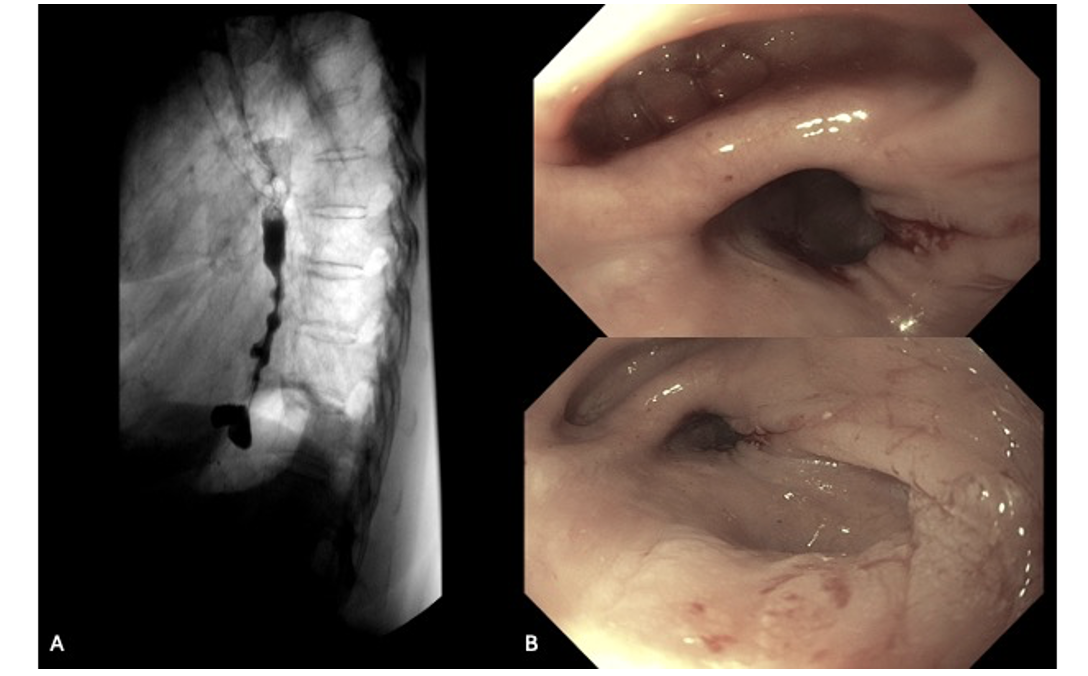
Figure: Figure 2A. Barium swallow confirming achalasia type 1. Figure 2B. EGD findings showing two diverticula in the distal esophagus for case 2.
Disclosures:
Shivangini Duggal indicated no relevant financial relationships.
Swati Mahapatra indicated no relevant financial relationships.
Keith Garrison indicated no relevant financial relationships.
Richard McCallum indicated no relevant financial relationships.
Shivangini Duggal, MD1, Swati Mahapatra, DO2, Keith Garrison, MD3, Richard McCallum, MD, FACG3. P5057 - Unveiling a Rare Coexistence: Achalasia Associated with Distal Esophageal and Gastric Diverticula – A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
