Tuesday Poster Session
Category: Esophagus
P5022 - U-Turn to Obstruction: A Flipped Case of EGJ Outflow Obstruction
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- MM
Momin Masroor, MD
University of California Irvine
Orange, CA
Presenting Author(s)
Momin Masroor, MD1, Andy Lin, MD1, Shoujit Banerjee, MD1, Trevor McCracken, MD1, Yuri Kwon, MD2, Frances Dang, MD, MSc3, Jason Samarasena, MD, MBA, FACG1, Peter Nguyen, MD1, Elliot Yu, MD3
1University of California Irvine, Orange, CA; 2University of California Irvine Health, Orange, CA; 3University of California Irvine, Irvine, CA
Introduction: Esophageal motility disorders can be challenging to interpret in the setting of altered anatomy. Large hernias can complicate manometric interpretation by distorting normal pressure patterns. We present a case of esophagogastric junction outflow obstruction (EGJOO) in a patient with significantly altered anatomy, where manometry findings were influenced by these anatomic changes.
Case Description/
Methods: 73-year-old male with a history of Barrett’s Esophagus presented with morning regurgitation and chronic cough. Incidentally when evaluated for pulmonary embolism, imaging revealed a large gastric herniation with axial rotation of the stomach causing the greater curvature to compress the esophagus (Figure 1). These anatomic findings are reflected on high-resolution manometry which demonstrates EGJ outflow obstruction with an elevated median integrated relaxation pressure (Figure 1). A large signal of intrabolus pressure is seen under the peristaltic contraction. This is in line with the fluoroscopic image of the greater curvature compressing the midthoracic esophagus. Striated esophageal contractions are prominent to push past this area of obstruction with intact smooth muscle peristalsis and normal distal latency. The slope of peristalsis, contractile front velocity, is altered from extrinsic gastric compression. The manometry catheter appears to not reach the stomach body and is curled up in the cardiac hernia, resulting in pressure artifacts in a butterfly pattern below the LES which may be overlapped with vascular artifact from the descending aorta.
Discussion: This case highlights the importance of interpreting esophageal manometry in the context of the patient’s clinical presentation and anatomy. Despite manometric distortion, clinical context from identifiable altered anatomy demonstrated findings consistent with an EGJOO. Distal latency should be measured from the start of UES relaxation to the contractile deceleration point with an isobar contour of 30 mmHg to avoid premature diagnosis of a spastic swallow. Although EGJOO is often an inconclusive diagnosis, with situational awareness, causes can be identified. For our patient, the presence of intact peristalsis suggests that esophageal clearance is likely preserved. Therefore, postoperative dysphagia may be less of a concern which is a key point to communicate for surgical planning. Manometric data should be interpreted alongside clinical and anatomical context for accurate diagnosis and management.
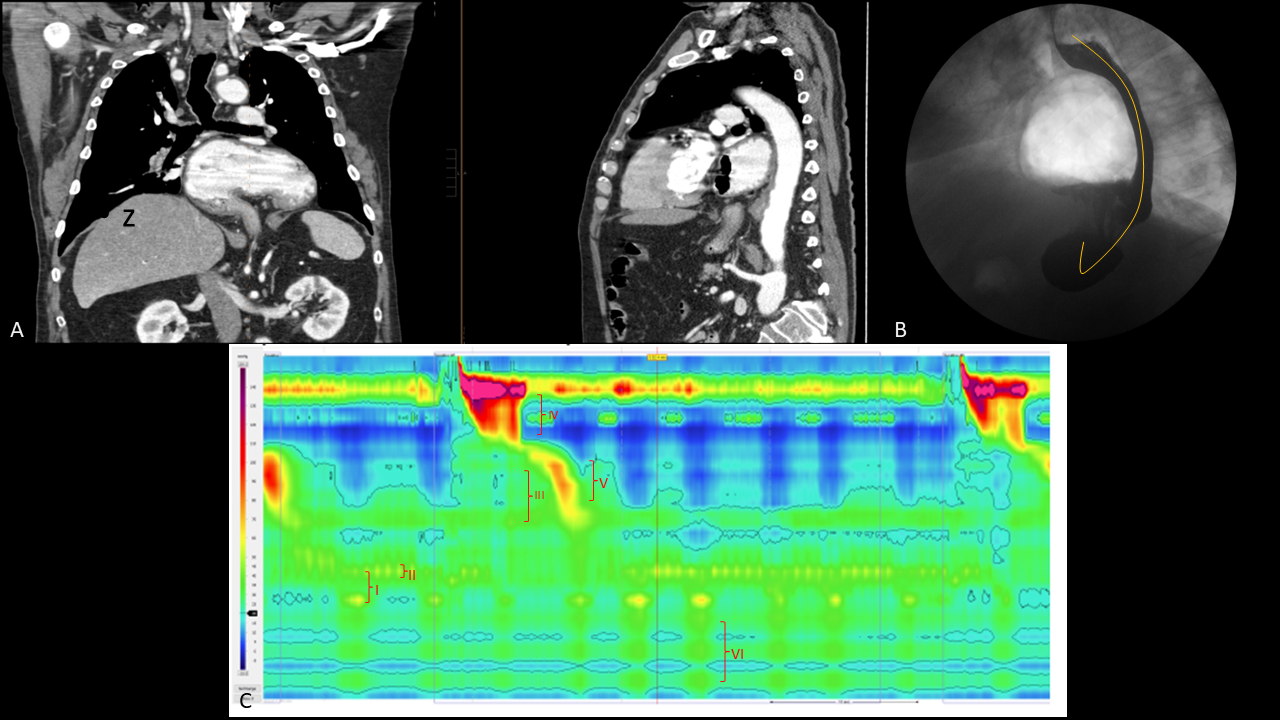
Figure: Figure 1A: CT showing prominent hiatal hernia with compression of esophagus by the great curvature of the stomach.
Figure 1B: Fluoroscopic imaging of hiatal hernia with proposed path of manometry catheter.
Figure 1C: Manometry showing LES above the diaphragmatic crux consistent with a hiatal hernia (I), IRP elevation (II), intrabolus pressure with stomach compression (III), prominent striated esophageal contraction (IV), intact smooth muscle peristalsis (V), and catheter artifact due to curling of the catheter (VI).
Disclosures:
Momin Masroor indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Shoujit Banerjee indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Yuri Kwon indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Peter Nguyen indicated no relevant financial relationships.
Elliot Yu indicated no relevant financial relationships.
Momin Masroor, MD1, Andy Lin, MD1, Shoujit Banerjee, MD1, Trevor McCracken, MD1, Yuri Kwon, MD2, Frances Dang, MD, MSc3, Jason Samarasena, MD, MBA, FACG1, Peter Nguyen, MD1, Elliot Yu, MD3. P5022 - U-Turn to Obstruction: A Flipped Case of EGJ Outflow Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of California Irvine, Orange, CA; 2University of California Irvine Health, Orange, CA; 3University of California Irvine, Irvine, CA
Introduction: Esophageal motility disorders can be challenging to interpret in the setting of altered anatomy. Large hernias can complicate manometric interpretation by distorting normal pressure patterns. We present a case of esophagogastric junction outflow obstruction (EGJOO) in a patient with significantly altered anatomy, where manometry findings were influenced by these anatomic changes.
Case Description/
Methods: 73-year-old male with a history of Barrett’s Esophagus presented with morning regurgitation and chronic cough. Incidentally when evaluated for pulmonary embolism, imaging revealed a large gastric herniation with axial rotation of the stomach causing the greater curvature to compress the esophagus (Figure 1). These anatomic findings are reflected on high-resolution manometry which demonstrates EGJ outflow obstruction with an elevated median integrated relaxation pressure (Figure 1). A large signal of intrabolus pressure is seen under the peristaltic contraction. This is in line with the fluoroscopic image of the greater curvature compressing the midthoracic esophagus. Striated esophageal contractions are prominent to push past this area of obstruction with intact smooth muscle peristalsis and normal distal latency. The slope of peristalsis, contractile front velocity, is altered from extrinsic gastric compression. The manometry catheter appears to not reach the stomach body and is curled up in the cardiac hernia, resulting in pressure artifacts in a butterfly pattern below the LES which may be overlapped with vascular artifact from the descending aorta.
Discussion: This case highlights the importance of interpreting esophageal manometry in the context of the patient’s clinical presentation and anatomy. Despite manometric distortion, clinical context from identifiable altered anatomy demonstrated findings consistent with an EGJOO. Distal latency should be measured from the start of UES relaxation to the contractile deceleration point with an isobar contour of 30 mmHg to avoid premature diagnosis of a spastic swallow. Although EGJOO is often an inconclusive diagnosis, with situational awareness, causes can be identified. For our patient, the presence of intact peristalsis suggests that esophageal clearance is likely preserved. Therefore, postoperative dysphagia may be less of a concern which is a key point to communicate for surgical planning. Manometric data should be interpreted alongside clinical and anatomical context for accurate diagnosis and management.
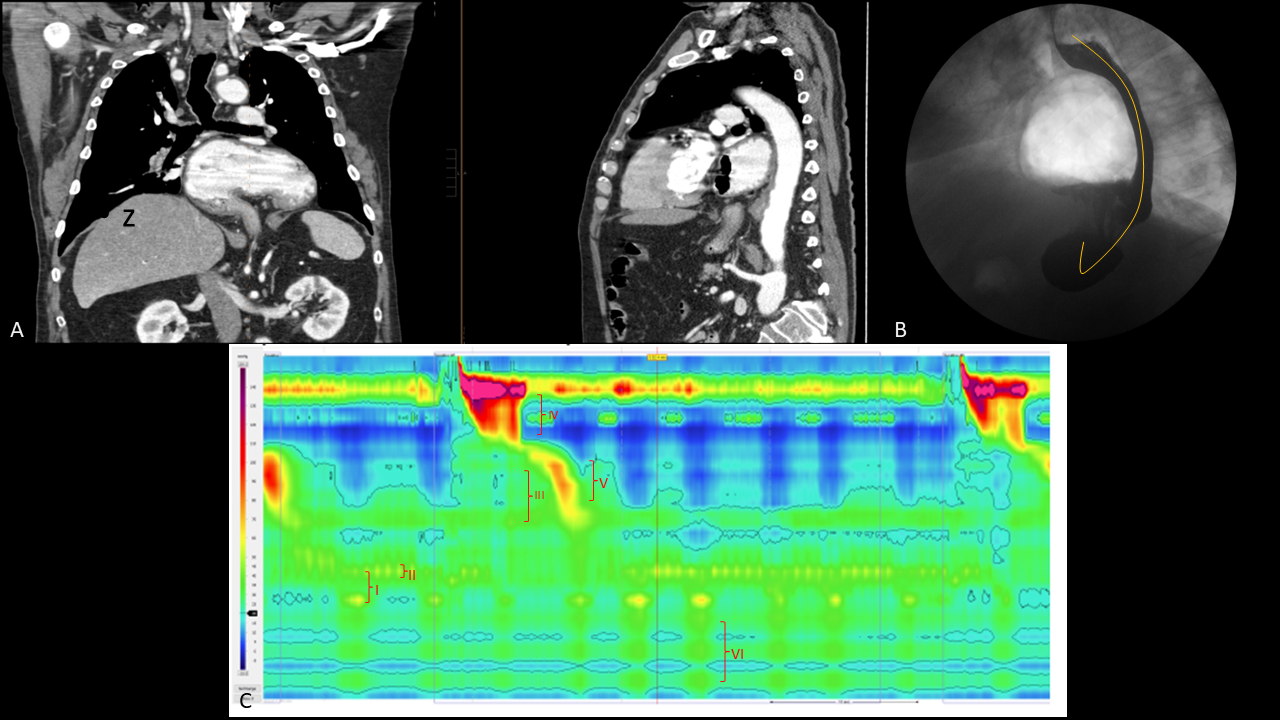
Figure: Figure 1A: CT showing prominent hiatal hernia with compression of esophagus by the great curvature of the stomach.
Figure 1B: Fluoroscopic imaging of hiatal hernia with proposed path of manometry catheter.
Figure 1C: Manometry showing LES above the diaphragmatic crux consistent with a hiatal hernia (I), IRP elevation (II), intrabolus pressure with stomach compression (III), prominent striated esophageal contraction (IV), intact smooth muscle peristalsis (V), and catheter artifact due to curling of the catheter (VI).
Disclosures:
Momin Masroor indicated no relevant financial relationships.
Andy Lin indicated no relevant financial relationships.
Shoujit Banerjee indicated no relevant financial relationships.
Trevor McCracken indicated no relevant financial relationships.
Yuri Kwon indicated no relevant financial relationships.
Frances Dang: Cook Medical – Speaker.
Jason Samarasena: Applied Medical – Consultant. Boston Scientific – Consultant. Cook Medical – Consultant. Neptune Medical – Consultant. Olympus – Consultant.
Peter Nguyen indicated no relevant financial relationships.
Elliot Yu indicated no relevant financial relationships.
Momin Masroor, MD1, Andy Lin, MD1, Shoujit Banerjee, MD1, Trevor McCracken, MD1, Yuri Kwon, MD2, Frances Dang, MD, MSc3, Jason Samarasena, MD, MBA, FACG1, Peter Nguyen, MD1, Elliot Yu, MD3. P5022 - U-Turn to Obstruction: A Flipped Case of EGJ Outflow Obstruction, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
