Tuesday Poster Session
Category: Esophagus
P5011 - A Rare Case of Diffuse Esophageal Intramural Pseudodiverticulosis!
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
- AD
Amir Darr, MD (he/him/his)
University Hospitals
Holland, OH
Presenting Author(s)
Amir Darr, MD1, Brendan Andres, MD2, Fady Haddad, MD2
1University Hospitals, Holland, OH; 2University Hospitals, Cleveland, OH
Introduction: Esophageal Intramural Pseudo-diverticulosis (EIPD) is a rare clinical entity of unclear etiology. It describes the presence of flask- shaped extraluminal outpouchings in the esophageal wall that result from cystic dilation of the excretory ducts of the esophageal submucosal glands. Despite that EIPD was previously described, it is a very rare and ambiguous entity with < 200 cases reported worldwide. We report the case of an elderly immunosuppressed man diagnosed with EIPD after presenting with worsening dysphagia.
Case Description/
Methods: A 65 year-old man with history of HIV-1 infection, gout, and hyperlipidemia presented with few months history of postprandial heartburn and solid food dysphagia. Medications included a combination of elvitegravir, cobicistat, emtracitibine, and tenofovir alafenamide in addition to colchicine and atorvastatin. Vital signs and physical exam were unremarkable. Labs showed an HIV1 viral load of 57 copies/mL and an absolute CD4 count of 678/mm3. Upper endoscopy showed diffuse moderate esophagitis with exudates and traversable diverticula-like structures throughout the esophagus (Fig 1). A traversable intrinsic stricture was also noted in the mid and distal esophagus. GMS and PAS fungal stains were positive for yeast and pseudohyphae consistent with candidiasis (Fig 2). CMV and HSV viral immnostains were negative. The patient received a 2 week course of flucanazole with complete resolution of his symptoms.
Discussion: First described in 1960, EIPD affects < 1% of the population. Etiology remains unclear with the most favored theory suggesting autonomic abnormality of the vagal nerve innervating the esophageal glands. Most patients have a history of heavy tobacco or alcohol use. EIPD can be asymptomatic. When present, symptoms include dysphagia, odynophagia, upper gastrointestinal bleeding and chest tightness. Diagnosis is suggested by endoscopy and barium esophagogram. Endoscopy shows multiple localized small mucosal depressions of yellowish or whitish coloration that look like diverticula. Up to 10% of patients with EIPD do not require interventions and are monitored conservatively. Management aims at controlling the underlying inflammation, relieving the patients' symptoms and treating the coexisting esophageal conditions. Despite that EIPD is considered a benign clinical entity, serious complications can occur including esophageal stricture, esophageal dysmotility, esophageal perforation, intra-mediastinal fistula, mediastinitis, and lung abscess.
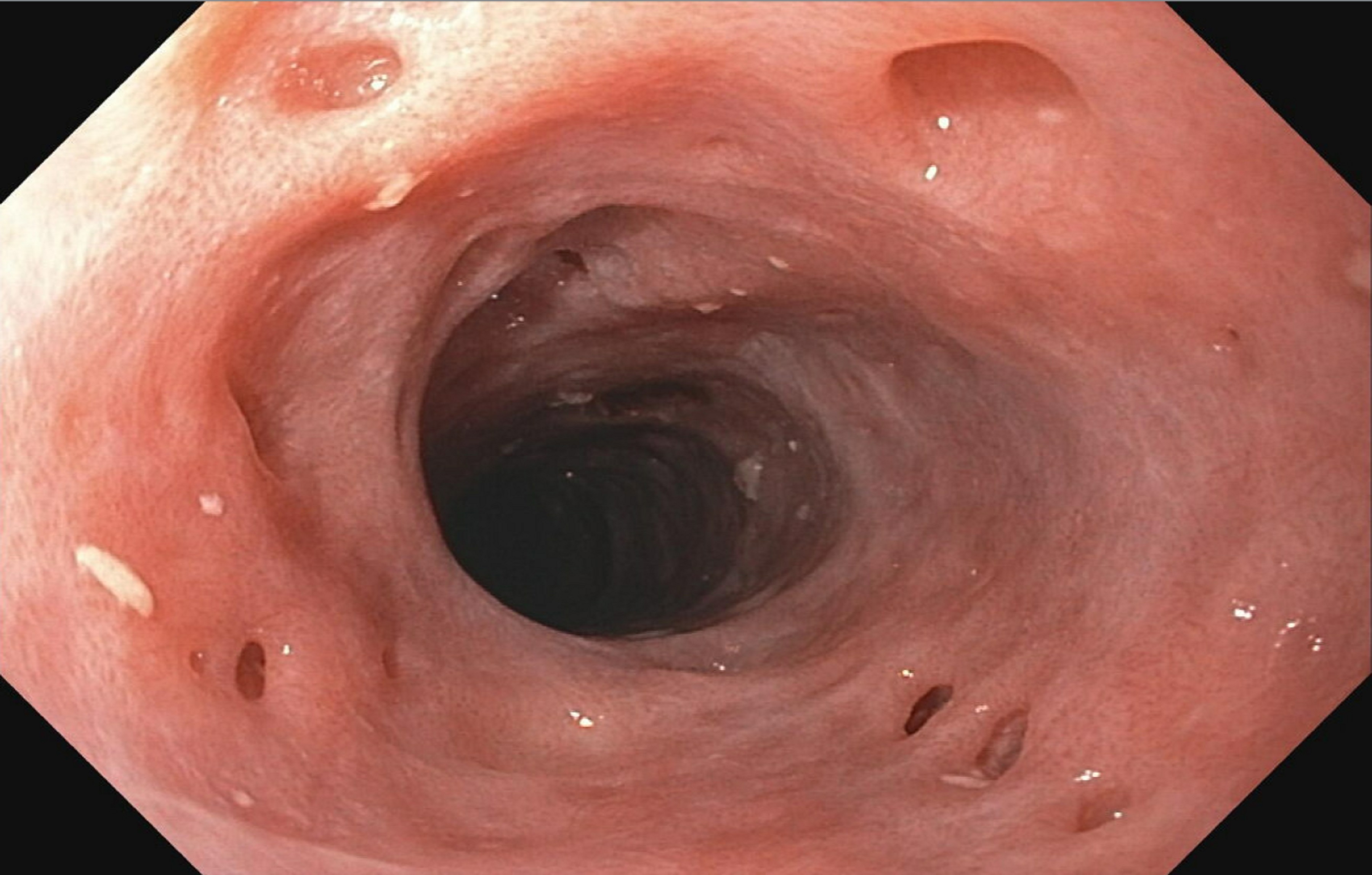
Figure: Esophageal Intramural Pseudo-Diverticulosis
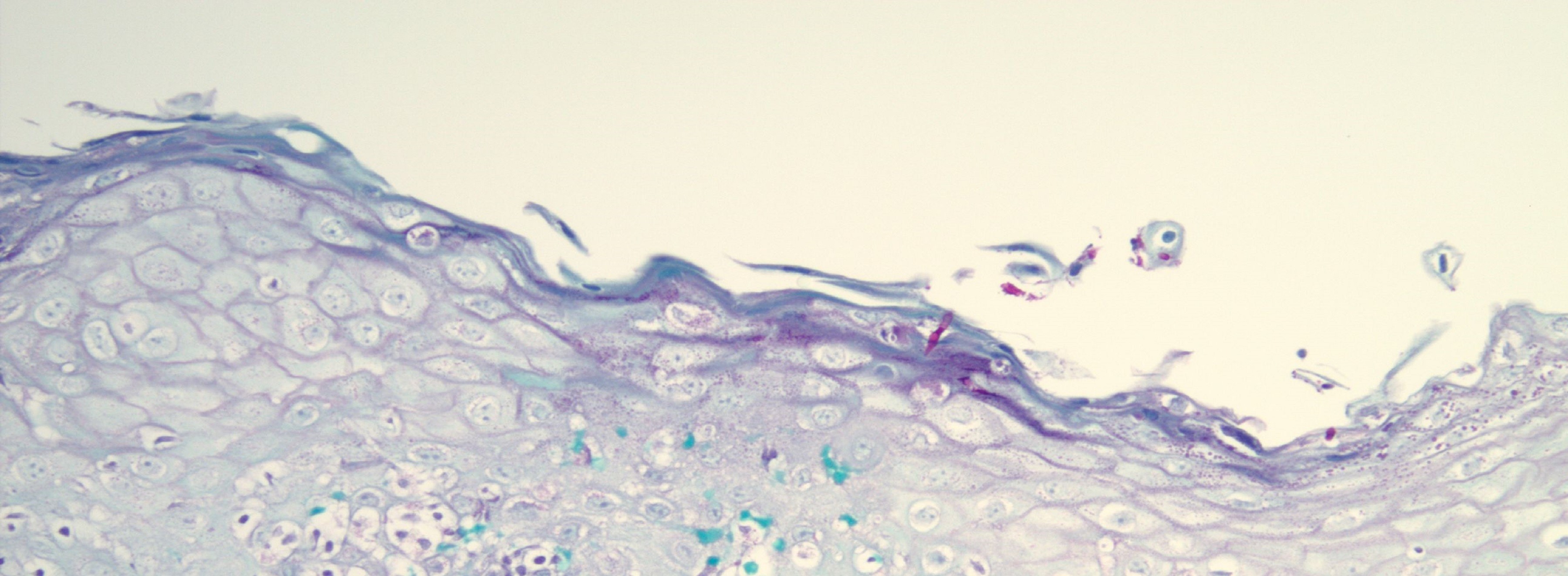
Figure: Pathology
Disclosures:
Amir Darr indicated no relevant financial relationships.
Brendan Andres indicated no relevant financial relationships.
Fady Haddad indicated no relevant financial relationships.
Amir Darr, MD1, Brendan Andres, MD2, Fady Haddad, MD2. P5011 - A Rare Case of Diffuse Esophageal Intramural Pseudodiverticulosis!, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University Hospitals, Holland, OH; 2University Hospitals, Cleveland, OH
Introduction: Esophageal Intramural Pseudo-diverticulosis (EIPD) is a rare clinical entity of unclear etiology. It describes the presence of flask- shaped extraluminal outpouchings in the esophageal wall that result from cystic dilation of the excretory ducts of the esophageal submucosal glands. Despite that EIPD was previously described, it is a very rare and ambiguous entity with < 200 cases reported worldwide. We report the case of an elderly immunosuppressed man diagnosed with EIPD after presenting with worsening dysphagia.
Case Description/
Methods: A 65 year-old man with history of HIV-1 infection, gout, and hyperlipidemia presented with few months history of postprandial heartburn and solid food dysphagia. Medications included a combination of elvitegravir, cobicistat, emtracitibine, and tenofovir alafenamide in addition to colchicine and atorvastatin. Vital signs and physical exam were unremarkable. Labs showed an HIV1 viral load of 57 copies/mL and an absolute CD4 count of 678/mm3. Upper endoscopy showed diffuse moderate esophagitis with exudates and traversable diverticula-like structures throughout the esophagus (Fig 1). A traversable intrinsic stricture was also noted in the mid and distal esophagus. GMS and PAS fungal stains were positive for yeast and pseudohyphae consistent with candidiasis (Fig 2). CMV and HSV viral immnostains were negative. The patient received a 2 week course of flucanazole with complete resolution of his symptoms.
Discussion: First described in 1960, EIPD affects < 1% of the population. Etiology remains unclear with the most favored theory suggesting autonomic abnormality of the vagal nerve innervating the esophageal glands. Most patients have a history of heavy tobacco or alcohol use. EIPD can be asymptomatic. When present, symptoms include dysphagia, odynophagia, upper gastrointestinal bleeding and chest tightness. Diagnosis is suggested by endoscopy and barium esophagogram. Endoscopy shows multiple localized small mucosal depressions of yellowish or whitish coloration that look like diverticula. Up to 10% of patients with EIPD do not require interventions and are monitored conservatively. Management aims at controlling the underlying inflammation, relieving the patients' symptoms and treating the coexisting esophageal conditions. Despite that EIPD is considered a benign clinical entity, serious complications can occur including esophageal stricture, esophageal dysmotility, esophageal perforation, intra-mediastinal fistula, mediastinitis, and lung abscess.
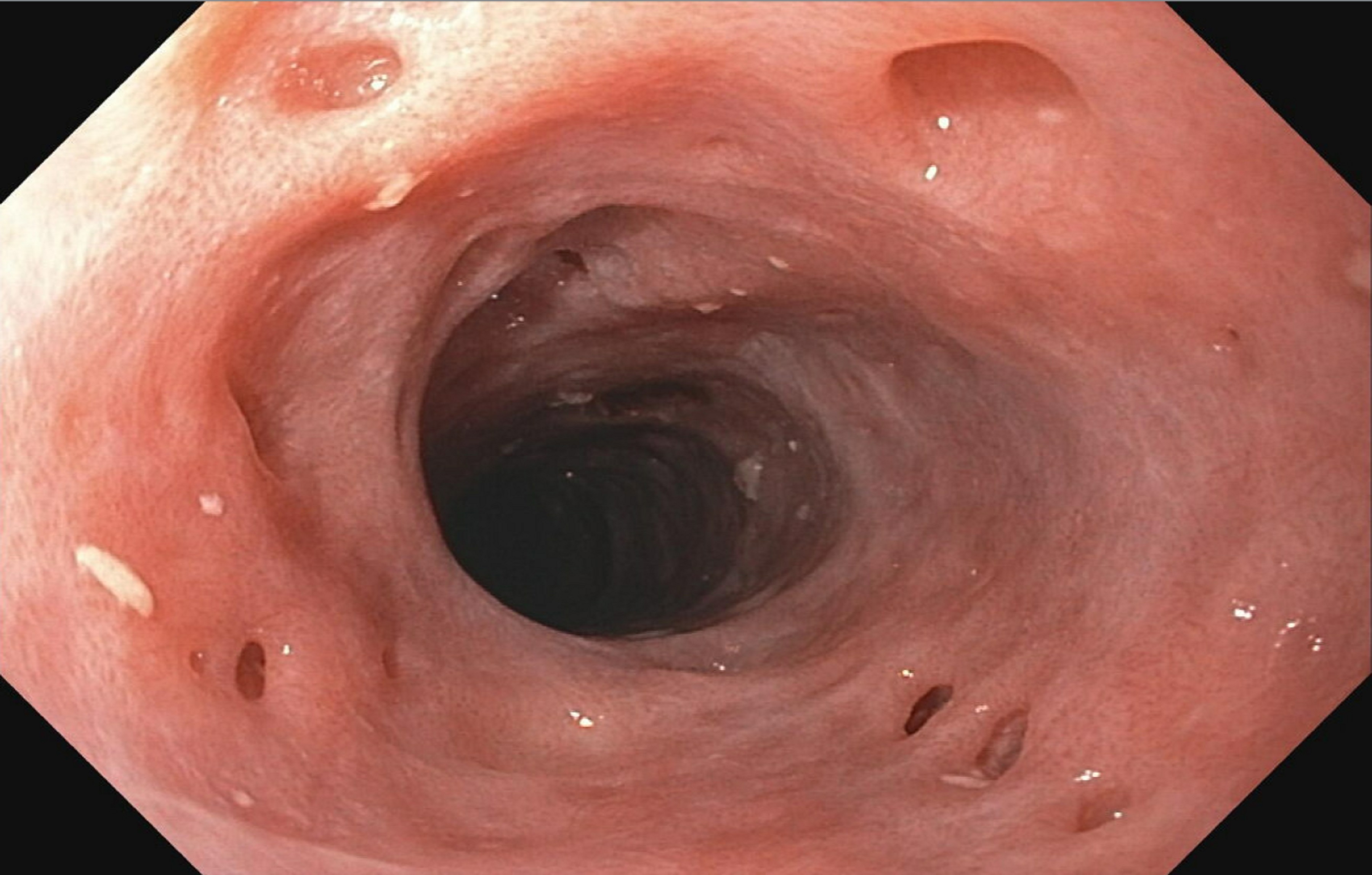
Figure: Esophageal Intramural Pseudo-Diverticulosis
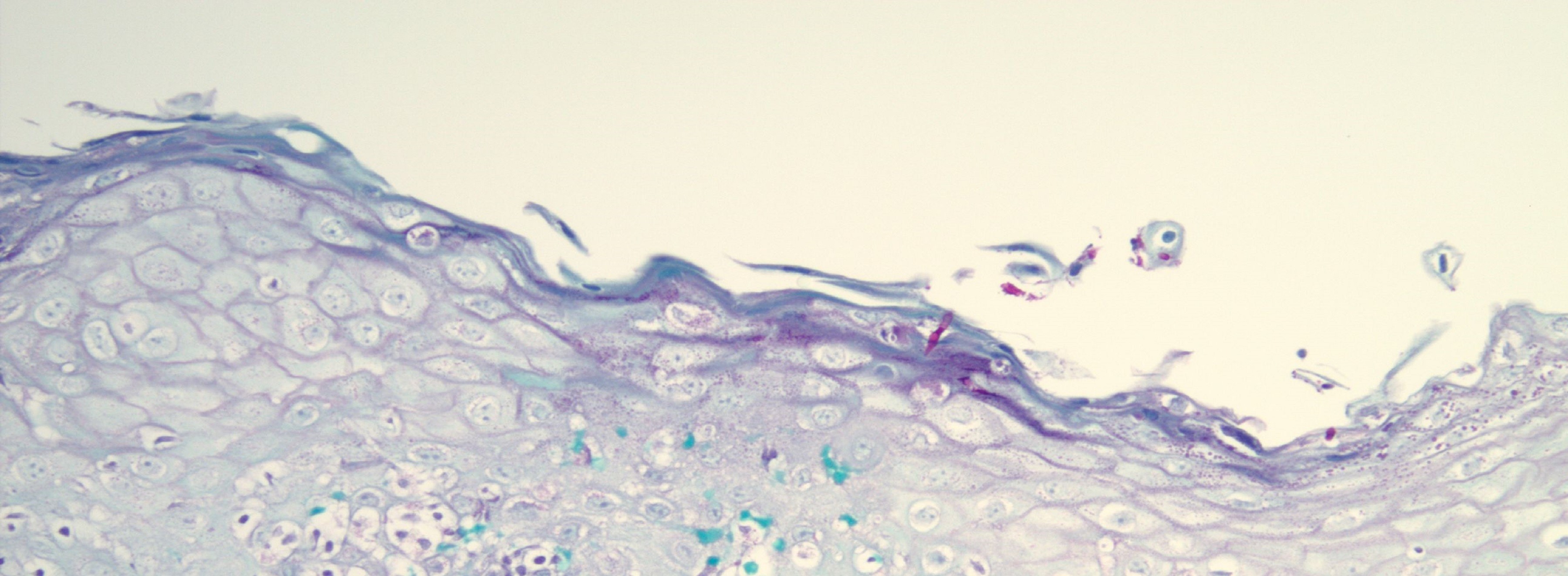
Figure: Pathology
Disclosures:
Amir Darr indicated no relevant financial relationships.
Brendan Andres indicated no relevant financial relationships.
Fady Haddad indicated no relevant financial relationships.
Amir Darr, MD1, Brendan Andres, MD2, Fady Haddad, MD2. P5011 - A Rare Case of Diffuse Esophageal Intramural Pseudodiverticulosis!, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
