Tuesday Poster Session
Category: Esophagus
P5003 - Endoscopic Stenting With Sutures for Palliation of Broncho-Esophageal Fistulas in Advanced Lung Cancer: A Case Series
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall
Yeshika Thapa, MD
University of Central Florida
Gainesville, FL
Presenting Author(s)
Yeshika Thapa, MD1, Carson Creamer, DO2, Bahar Rehan, MD2, Mohammed Janajrah, MD3, Yaseen Perbtani, DO2, Tony Brar, MD1
1University of Central Florida, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL; 3UCF/HCA Florida North Florida, Gainesville, FL
Introduction: Broncho-esophageal fistula (BEF) is a rare and often fatal complication of advanced lung carcinoma, often leading to recurrent aspiration, malnutrition, and infections, severely limiting quality of life and patient survival. Surgical options are often not viable due to poor functional status and extensive disease, especially in patients who have undergone prior radiation or thoracic surgery. In such cases, minimally invasive endoscopic stenting offers a promising alternative for symptom relief. This case series presents two patients with lung cancer-associated BEF, showing how endoscopic stenting especially when secured with sutures can provide meaningful palliation.
Case Description/
Methods: Case 1: A 75-year-old man with stage IV non-small cell lung cancer with previous left lower lobectomy and radiotherapy presented with worsening dysphagia and shortness of breath. Endoscopy revealed a 10 mm fistula in the mid-esophagus. Due to ineligibility for surgery, he underwent endoscopic palliation with placement of a 23×120 mm fully covered self-expanding metal stent (SEMS), secured with a single 2.0 polypropylene suture in a running fashion and cinches at both ends to prevent migration. This technique achieved effective tissue approximation and stent fixation without bleeding or leakage. The patient showed marked symptom relief and resumed oral intake, in lieu of a feeding tube.
Case 2: A 60-year-old man with newly diagnosed lung adenocarcinoma and severe COPD reported significant weight loss, shortness of breath and worsening dysphagia. Imaging and endoscopy confirmed a large fistula, which was successfully closed with a fully covered SEMS. The patient was able to resume oral intake and avoid a feeding tube, significantly improving his comfort and function.
Discussion: These cases illustrate the challenges of managing BEF in advanced lung cancer patients who are poor surgical candidates. Esophageal stenting offers quick and effective palliation, allowing symptom relief and improved oral intake. Importantly, adding a running suture to anchor the stent as seen in Case 1 helped prevent migration and ensured a better seal. This simple technique was safe and improved stent stability without complications. While outcomes are still limited by disease progression, this approach can restore quality of life and function, even if only temporarily. These cases support the role of endoscopic stenting with suturing as a valuable tool for palliation of malignant BEFs.
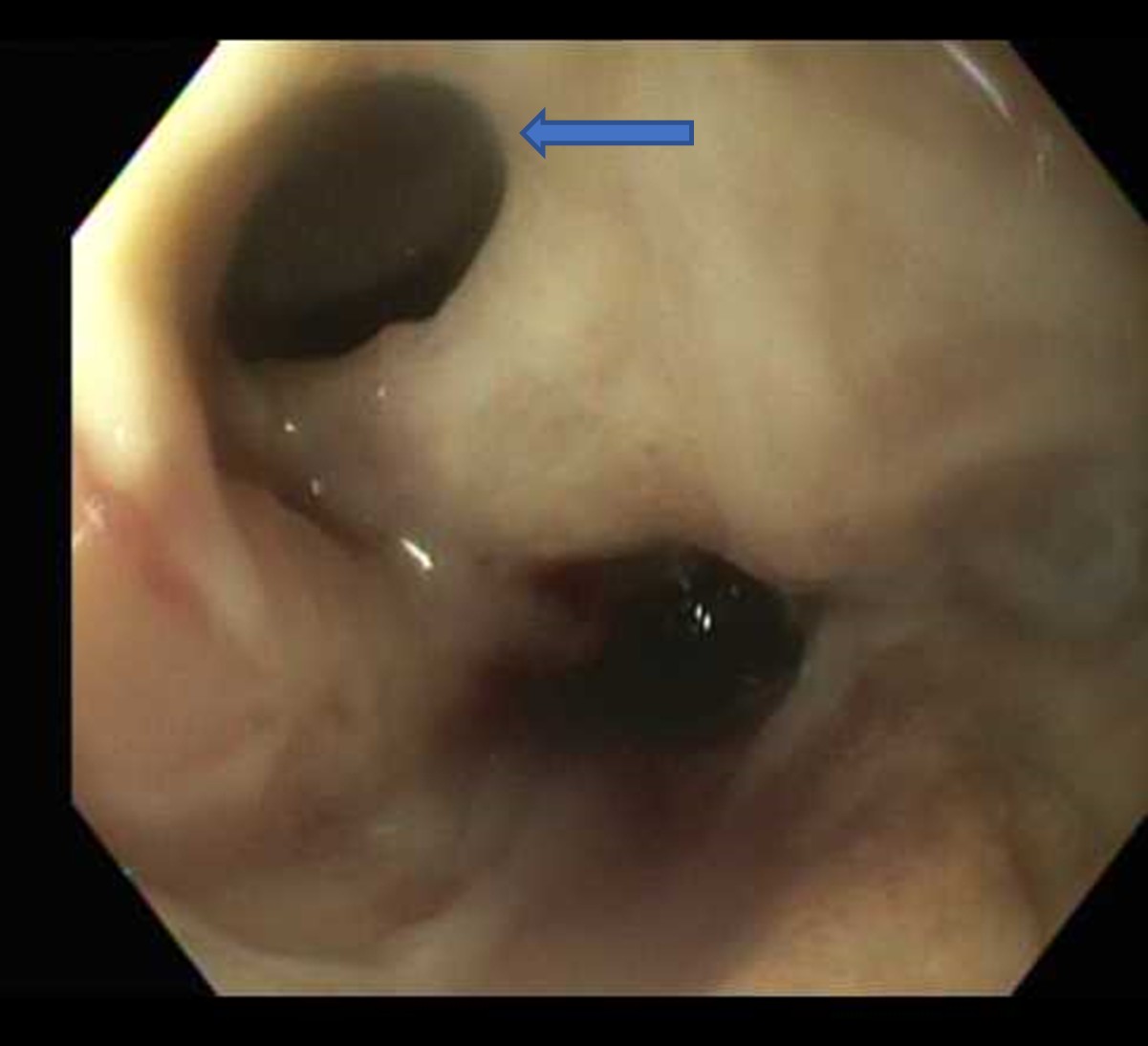
Figure: A 10 mm fistula in the middle third of the esophagus on EGD.
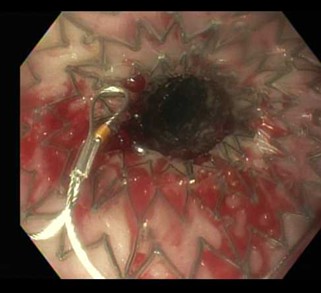
Figure: A fully covered stent was placed over the defect in the middle third of the esophagus.
Disclosures:
Yeshika Thapa indicated no relevant financial relationships.
Carson Creamer indicated no relevant financial relationships.
Bahar Rehan indicated no relevant financial relationships.
Mohammed Janajrah indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yeshika Thapa, MD1, Carson Creamer, DO2, Bahar Rehan, MD2, Mohammed Janajrah, MD3, Yaseen Perbtani, DO2, Tony Brar, MD1. P5003 - Endoscopic Stenting With Sutures for Palliation of Broncho-Esophageal Fistulas in Advanced Lung Cancer: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Central Florida, Gainesville, FL; 2University of Central Florida, HCA Healthcare GME, Gainesville, FL; 3UCF/HCA Florida North Florida, Gainesville, FL
Introduction: Broncho-esophageal fistula (BEF) is a rare and often fatal complication of advanced lung carcinoma, often leading to recurrent aspiration, malnutrition, and infections, severely limiting quality of life and patient survival. Surgical options are often not viable due to poor functional status and extensive disease, especially in patients who have undergone prior radiation or thoracic surgery. In such cases, minimally invasive endoscopic stenting offers a promising alternative for symptom relief. This case series presents two patients with lung cancer-associated BEF, showing how endoscopic stenting especially when secured with sutures can provide meaningful palliation.
Case Description/
Methods: Case 1: A 75-year-old man with stage IV non-small cell lung cancer with previous left lower lobectomy and radiotherapy presented with worsening dysphagia and shortness of breath. Endoscopy revealed a 10 mm fistula in the mid-esophagus. Due to ineligibility for surgery, he underwent endoscopic palliation with placement of a 23×120 mm fully covered self-expanding metal stent (SEMS), secured with a single 2.0 polypropylene suture in a running fashion and cinches at both ends to prevent migration. This technique achieved effective tissue approximation and stent fixation without bleeding or leakage. The patient showed marked symptom relief and resumed oral intake, in lieu of a feeding tube.
Case 2: A 60-year-old man with newly diagnosed lung adenocarcinoma and severe COPD reported significant weight loss, shortness of breath and worsening dysphagia. Imaging and endoscopy confirmed a large fistula, which was successfully closed with a fully covered SEMS. The patient was able to resume oral intake and avoid a feeding tube, significantly improving his comfort and function.
Discussion: These cases illustrate the challenges of managing BEF in advanced lung cancer patients who are poor surgical candidates. Esophageal stenting offers quick and effective palliation, allowing symptom relief and improved oral intake. Importantly, adding a running suture to anchor the stent as seen in Case 1 helped prevent migration and ensured a better seal. This simple technique was safe and improved stent stability without complications. While outcomes are still limited by disease progression, this approach can restore quality of life and function, even if only temporarily. These cases support the role of endoscopic stenting with suturing as a valuable tool for palliation of malignant BEFs.
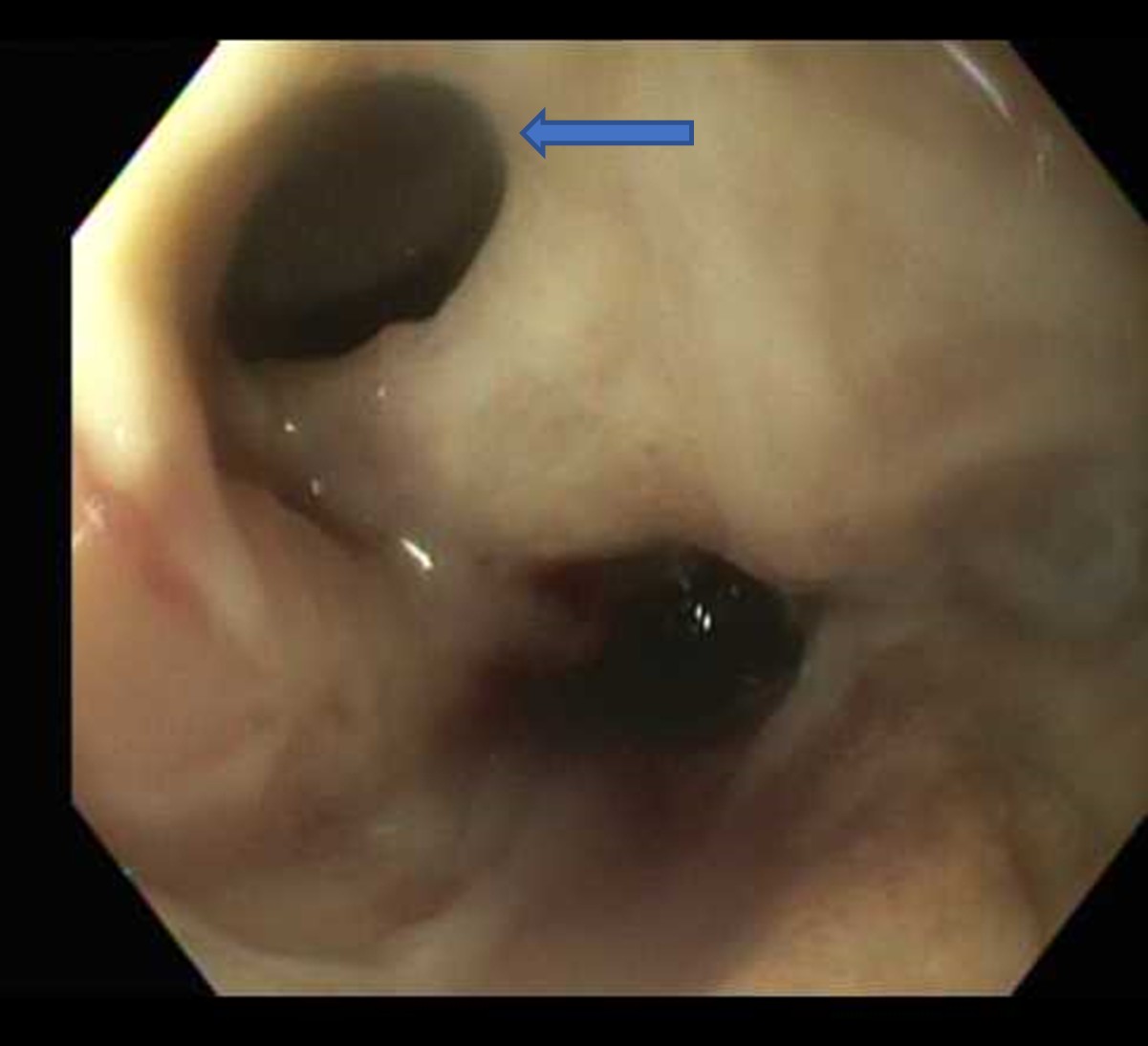
Figure: A 10 mm fistula in the middle third of the esophagus on EGD.
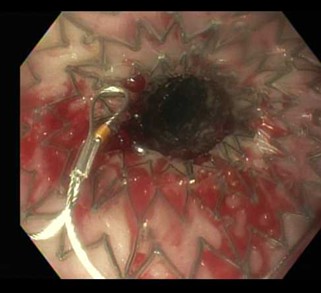
Figure: A fully covered stent was placed over the defect in the middle third of the esophagus.
Disclosures:
Yeshika Thapa indicated no relevant financial relationships.
Carson Creamer indicated no relevant financial relationships.
Bahar Rehan indicated no relevant financial relationships.
Mohammed Janajrah indicated no relevant financial relationships.
Yaseen Perbtani indicated no relevant financial relationships.
Tony Brar indicated no relevant financial relationships.
Yeshika Thapa, MD1, Carson Creamer, DO2, Bahar Rehan, MD2, Mohammed Janajrah, MD3, Yaseen Perbtani, DO2, Tony Brar, MD1. P5003 - Endoscopic Stenting With Sutures for Palliation of Broncho-Esophageal Fistulas in Advanced Lung Cancer: A Case Series, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
