Tuesday Poster Session
Category: Esophagus
P5000 - Gurvits Syndrome Following Septic Shock: A Case Report and Review of Management
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Chris Pace, DO (he/him/his)
Valley Hospital Medical Center
Las Vegas, NV
Presenting Author(s)
Christopher Pace, DO, John Ko, DO, Melanie De Shadarevian, DO, Christina Joya, DO, Vishvinder Sharma, MD
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Acute esophageal necrosis (AEN), or Gurvits syndrome, is a rare condition marked by diffuse black discoloration of the esophageal mucosa due to necrosis. It typically affects the distal third of the esophagus and ends abruptly at the gastroesophageal (GE) junction. Its prevalence is estimated at 0.2% based on autopsy studies. The exact pathogenesis is unclear but AEN has been linked to a variety of conditions. We present a case of AEN likely secondary to critical illness.
Case Description/
Methods: 76-year-old man with advanced dementia and chronic debility presented with hemoptysis. One month earlier, he had undergone PEG tube placement for aspiration pneumonia and dysphagia.
On admission, CT abdomen/pelvis showed stable pneumoperitoneum from prior imaging. Chest CT revealed bilateral pleural effusions and lower lobe endobronchial obstruction. He was started on meropenem and vancomycin for suspected pneumonia.
He later developed melena with hemoglobin dropping to 6.2 g/dL. During transfusion, he became acutely altered, hypoxic, and hypotensive, requiring intubation and vasopressors.
EGD revealed a diffusely black necrotic esophagus ending sharply at the GE junction—findings consistent with AEN. He was started on high-dose proton pump inhibitors (PPIs), and enteral nutrition was resumed via PEG tube.
Discussion: AEN is believed to result from a "two-hit" mechanism: first, a hypo-perfusion event, followed by secondary injury, such as acid reflux. The distal esophagus is especially vulnerable due to its relatively poor blood supply. In this case, septic shock and hypoxia likely caused ischemia of the distal esophagus, followed by chemical injury from acid reflux. AEN can develop within 18 hours of the inciting event and presents with a GI bleed in 70% of cases.
Initial treatment focuses on treating the underlying cause of hypo-perfusion. The patient should be given fluid resuscitation to restore perfusion and PPI therapy to reduce further topical injury. Oral feeding should be stopped for 24 hours, if oral intake cannot resume after 24 hours, parenteral nutrition should be considered.
With conservative management and restoration of adequate perfusion to the esophagus, endoscopic findings resolve in most cases. However, complications of esophageal perforation (7% of cases), and esophageal strictures (40% of cases) may develop during recovery. Close monitoring following diagnosis and follow-up endoscopy is warranted to assess for healing and stricture formation.
*Generative AI used to edit this paper
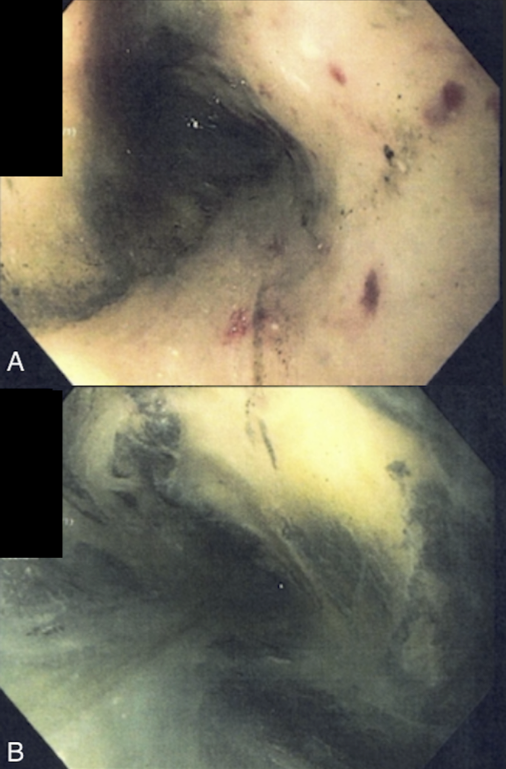
Figure: Images captured during Upper Endoscopy
A: Mid - Distal Third esophagus showing transition to necrotic esophageal mucosa
B: Distal Esophagus prior to GE junction showing diffuse black necrotic mucosa
Disclosures:
Christopher Pace indicated no relevant financial relationships.
John Ko indicated no relevant financial relationships.
Melanie De Shadarevian indicated no relevant financial relationships.
Christina Joya indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christopher Pace, DO, John Ko, DO, Melanie De Shadarevian, DO, Christina Joya, DO, Vishvinder Sharma, MD. P5000 - Gurvits Syndrome Following Septic Shock: A Case Report and Review of Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
Valley Hospital Medical Center, Las Vegas, NV
Introduction: Acute esophageal necrosis (AEN), or Gurvits syndrome, is a rare condition marked by diffuse black discoloration of the esophageal mucosa due to necrosis. It typically affects the distal third of the esophagus and ends abruptly at the gastroesophageal (GE) junction. Its prevalence is estimated at 0.2% based on autopsy studies. The exact pathogenesis is unclear but AEN has been linked to a variety of conditions. We present a case of AEN likely secondary to critical illness.
Case Description/
Methods: 76-year-old man with advanced dementia and chronic debility presented with hemoptysis. One month earlier, he had undergone PEG tube placement for aspiration pneumonia and dysphagia.
On admission, CT abdomen/pelvis showed stable pneumoperitoneum from prior imaging. Chest CT revealed bilateral pleural effusions and lower lobe endobronchial obstruction. He was started on meropenem and vancomycin for suspected pneumonia.
He later developed melena with hemoglobin dropping to 6.2 g/dL. During transfusion, he became acutely altered, hypoxic, and hypotensive, requiring intubation and vasopressors.
EGD revealed a diffusely black necrotic esophagus ending sharply at the GE junction—findings consistent with AEN. He was started on high-dose proton pump inhibitors (PPIs), and enteral nutrition was resumed via PEG tube.
Discussion: AEN is believed to result from a "two-hit" mechanism: first, a hypo-perfusion event, followed by secondary injury, such as acid reflux. The distal esophagus is especially vulnerable due to its relatively poor blood supply. In this case, septic shock and hypoxia likely caused ischemia of the distal esophagus, followed by chemical injury from acid reflux. AEN can develop within 18 hours of the inciting event and presents with a GI bleed in 70% of cases.
Initial treatment focuses on treating the underlying cause of hypo-perfusion. The patient should be given fluid resuscitation to restore perfusion and PPI therapy to reduce further topical injury. Oral feeding should be stopped for 24 hours, if oral intake cannot resume after 24 hours, parenteral nutrition should be considered.
With conservative management and restoration of adequate perfusion to the esophagus, endoscopic findings resolve in most cases. However, complications of esophageal perforation (7% of cases), and esophageal strictures (40% of cases) may develop during recovery. Close monitoring following diagnosis and follow-up endoscopy is warranted to assess for healing and stricture formation.
*Generative AI used to edit this paper
Figure: Images captured during Upper Endoscopy
A: Mid - Distal Third esophagus showing transition to necrotic esophageal mucosa
B: Distal Esophagus prior to GE junction showing diffuse black necrotic mucosa
Disclosures:
Christopher Pace indicated no relevant financial relationships.
John Ko indicated no relevant financial relationships.
Melanie De Shadarevian indicated no relevant financial relationships.
Christina Joya indicated no relevant financial relationships.
Vishvinder Sharma indicated no relevant financial relationships.
Christopher Pace, DO, John Ko, DO, Melanie De Shadarevian, DO, Christina Joya, DO, Vishvinder Sharma, MD. P5000 - Gurvits Syndrome Following Septic Shock: A Case Report and Review of Management, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
