Tuesday Poster Session
Category: Esophagus
P4998 - Primary Esophageal Mucosa-Associated Lymphoid Tissue Lymphoma Masquerading as a Benign Tumor
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Agustin Gavidia Rosario, MD
Henry Ford Health
Detroit, MI
Presenting Author(s)
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Jonathan A. Montrose, DO2, Hollis Johanson, MD2, Omar Abbas, MD2, Sumit Singla, MD2, Keith E. Mullins, MD2, Tobias Zuchelli, 1, Andrew M. Popoff, MD2, Mazen Elatrache, MD2
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Primary gastrointestinal (GI) lymphomas represent only 10–15% of all non-Hodgkin lymphomas (NHLs), with esophageal involvement being extremely rare—accounting for less than 1% of GI lymphomas and only 0.2% of extra-nodal NHLs. Most esophageal cases arise from direct extension of adjacent disease, while primary esophageal lymphomas (PEL) are exceptionally rare. Mucosa-associated lymphoid tissue (MALT) lymphoma is a rare but recognized variant. Its pathogenesis in the esophagus remains poorly understood, and clinical presentations are often nonspecific, hindering timely diagnosis. We present a rare case of primary esophageal malt lymphoma.
Case Description/
Methods: A 53-year-old man underwent a screening cardiac computed tomography (CT) due to a strong family history of coronary artery disease. A filling defect in the distal esophagus was incidentally identified. Retrospective review of imaging from three years prior showed a similar but smaller lesion. The patient was asymptomatic. Esophagogastroduodenoscopy (EGD) revealed a 3×1 cm submucosal lesion in the distal esophagus (Figure 1). Endoscopic ultrasound (EUS) identified a subepithelial nodule, 32–38 cm from the incisors causing luminal narrowing (Figure 2). The lesion appeared predominantly anechoic to slightly hypoechoic, originating from the submucosa. Esophagogram showed a polypoid mass without high-grade obstruction. Fine-needle biopsy was deferred due to concern for possible duplication cyst. Magnetic resonance imaging (MRI) suggested a solid lesion, possibly leiomyoma, and chest CT confirmed interval growth of a distal esophageal soft tissue mass. The patient underwent a robotic-assisted resection of the periesophageal nodule and mass. Histopathology confirmed extra-nodal marginal zone lymphoma (MALT lymphoma) of the esophagus. PET scan revealed moderate metabolic activity in the esophageal mass and widespread nodal involvement in the neck, thorax, abdomen, and inguinal regions consistent with stage IV disease. The patient was subsequently referred to hematology and initiated on a six-week course of Rituximab therapy, with plans for ongoing response assessment.
Discussion: This case illustrates a rare presentation of primary esophageal MALT lymphoma discovered incidentally in an asymptomatic patient. It underscores the diagnostic complexity of submucosal esophageal lesions and the importance of considering lymphoma in the differential. Early identification and appropriate staging are critical to guide timely therapy and improve outcomes.
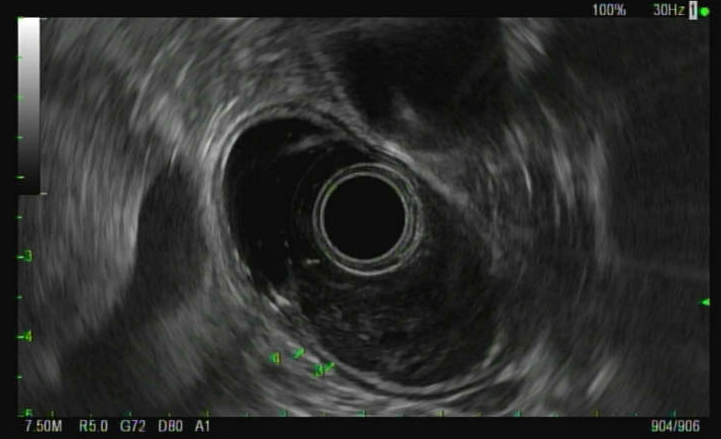
Figure: Figure 1: Subepithelial esophageal nodule resulting in partial obstruction of the esophagus
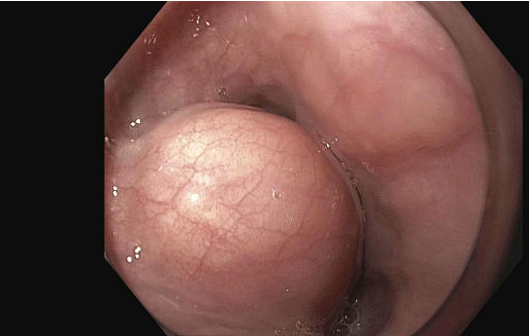
Figure: Figure 2: EUS showing hypoechoic esophageal subepithelial nodule arising from the submucosa (Layer 3).
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Hollis Johanson indicated no relevant financial relationships.
Omar Abbas indicated no relevant financial relationships.
Sumit Singla: Boston Scientific. – Consultant.
Keith E. Mullins indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Andrew Popoff: Intuitive Surgical – Consultant. Oxford Performance Materials – Consultant. Premier – Consultant.
Mazen Elatrache indicated no relevant financial relationships.
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Jonathan A. Montrose, DO2, Hollis Johanson, MD2, Omar Abbas, MD2, Sumit Singla, MD2, Keith E. Mullins, MD2, Tobias Zuchelli, 1, Andrew M. Popoff, MD2, Mazen Elatrache, MD2. P4998 - Primary Esophageal Mucosa-Associated Lymphoid Tissue Lymphoma Masquerading as a Benign Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1Henry Ford Hospital, Detroit, MI; 2Henry Ford Health, Detroit, MI
Introduction: Primary gastrointestinal (GI) lymphomas represent only 10–15% of all non-Hodgkin lymphomas (NHLs), with esophageal involvement being extremely rare—accounting for less than 1% of GI lymphomas and only 0.2% of extra-nodal NHLs. Most esophageal cases arise from direct extension of adjacent disease, while primary esophageal lymphomas (PEL) are exceptionally rare. Mucosa-associated lymphoid tissue (MALT) lymphoma is a rare but recognized variant. Its pathogenesis in the esophagus remains poorly understood, and clinical presentations are often nonspecific, hindering timely diagnosis. We present a rare case of primary esophageal malt lymphoma.
Case Description/
Methods: A 53-year-old man underwent a screening cardiac computed tomography (CT) due to a strong family history of coronary artery disease. A filling defect in the distal esophagus was incidentally identified. Retrospective review of imaging from three years prior showed a similar but smaller lesion. The patient was asymptomatic. Esophagogastroduodenoscopy (EGD) revealed a 3×1 cm submucosal lesion in the distal esophagus (Figure 1). Endoscopic ultrasound (EUS) identified a subepithelial nodule, 32–38 cm from the incisors causing luminal narrowing (Figure 2). The lesion appeared predominantly anechoic to slightly hypoechoic, originating from the submucosa. Esophagogram showed a polypoid mass without high-grade obstruction. Fine-needle biopsy was deferred due to concern for possible duplication cyst. Magnetic resonance imaging (MRI) suggested a solid lesion, possibly leiomyoma, and chest CT confirmed interval growth of a distal esophageal soft tissue mass. The patient underwent a robotic-assisted resection of the periesophageal nodule and mass. Histopathology confirmed extra-nodal marginal zone lymphoma (MALT lymphoma) of the esophagus. PET scan revealed moderate metabolic activity in the esophageal mass and widespread nodal involvement in the neck, thorax, abdomen, and inguinal regions consistent with stage IV disease. The patient was subsequently referred to hematology and initiated on a six-week course of Rituximab therapy, with plans for ongoing response assessment.
Discussion: This case illustrates a rare presentation of primary esophageal MALT lymphoma discovered incidentally in an asymptomatic patient. It underscores the diagnostic complexity of submucosal esophageal lesions and the importance of considering lymphoma in the differential. Early identification and appropriate staging are critical to guide timely therapy and improve outcomes.
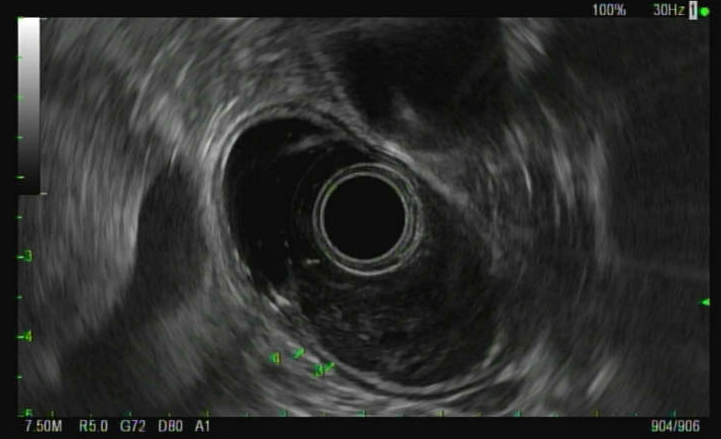
Figure: Figure 1: Subepithelial esophageal nodule resulting in partial obstruction of the esophagus
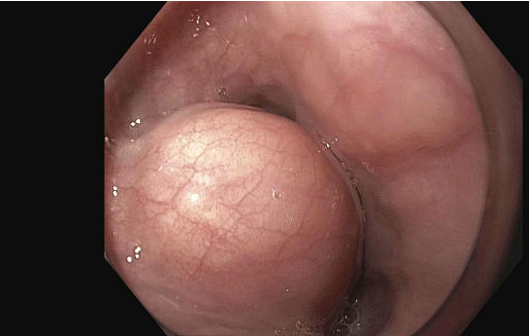
Figure: Figure 2: EUS showing hypoechoic esophageal subepithelial nodule arising from the submucosa (Layer 3).
Disclosures:
Mohammed Abusuliman indicated no relevant financial relationships.
Agustin Gavidia Rosario indicated no relevant financial relationships.
Jonathan Montrose indicated no relevant financial relationships.
Hollis Johanson indicated no relevant financial relationships.
Omar Abbas indicated no relevant financial relationships.
Sumit Singla: Boston Scientific. – Consultant.
Keith E. Mullins indicated no relevant financial relationships.
Tobias Zuchelli: Boston Scientific – Consultant.
Andrew Popoff: Intuitive Surgical – Consultant. Oxford Performance Materials – Consultant. Premier – Consultant.
Mazen Elatrache indicated no relevant financial relationships.
Mohammed Abusuliman, MD1, Agustin Gavidia Rosario, MD2, Jonathan A. Montrose, DO2, Hollis Johanson, MD2, Omar Abbas, MD2, Sumit Singla, MD2, Keith E. Mullins, MD2, Tobias Zuchelli, 1, Andrew M. Popoff, MD2, Mazen Elatrache, MD2. P4998 - Primary Esophageal Mucosa-Associated Lymphoid Tissue Lymphoma Masquerading as a Benign Tumor, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
