Tuesday Poster Session
Category: Esophagus
P4993 - Black Esophagus: A Rare Case of Upper GI Bleeding From Acute Esophageal Necrosis in the Setting of Recent Influenza Infection
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Natalie Rosseau, MD (she/her/hers)
University of Florida Health Shands Hospital
Gainesville, FL
Presenting Author(s)
Natalie Rosseau, MD1, Hannah Zuercher, MD1, Marlee Panther, MD1, Katherine Ray, DO1, Ahmed Al Qady, MD2, Amitabh Kumar, MD1
1University of Florida Health Shands Hospital, Gainesville, FL; 2University of Florida, Gainesville, FL
Introduction: Acute esophageal necrosis (AEN) is a rare cause of upper gastrointestinal bleeding (UGIB), defined by circumferential black-appearing esophageal mucosa in the distal esophagus. We present a case of AEN in an immunocompetent patient with type 2 diabetes mellitus, atherosclerotic disease, and recent influenza A infection treated with oseltamivir.
Case Description/
Methods: A male in his seventies with a past medical history of DM, CAD, HTN, and HLD presented with a syncopal episode and a two-day history of hematemesis, melena, and weakness. Upon presentation, he was afebrile with a blood pressure of 94/74. At home, he was on naproxen for osteoarthritis and apixaban for atrial fibrillation. A week prior to this presentation, he was admitted to an outside hospital for respiratory failure secondary to an influenza A infection, which was treated with oseltamivir.
Initial laboratory analysis showed a hemoglobin of 7.8 g/dL from 15.4 g/dL a week prior (normal: 13.0-16.5 g/dL), elevated white blood cell count of 14.3 x10E3/uL (normal: 4.0-10.0 x10E3/uL), and an elevated whole blood lactic acid at 3.1 mmol/L (normal: 0.3-1.5 mmol/L). Computed tomography angiography of the abdomen and pelvis with contrast was unremarkable. He received one unit of packed red blood cells and underwent an urgent upper endoscopy (EGD), which demonstrated Los Angeles (LA) Classification Grade D necrotizing esophagitis (Figure 1, Part C), LA Classification Grade B reflux esophagitis (Figure 1, Parts A and B), and erosive gastropathy (Figure 2, Part C), all without active or recent bleeding. Pathology revealed acute inflammation and ulcer debris, with no evidence of viral or fungal infections.
The patient was treated with an eight-week course of omeprazole 40mg twice daily and a second therapeutic course of oseltamivir. The bleeding ceased, and his hemoglobin levels remained stable. Anticoagulation was resumed after risk-benefit discussion. He was discharged to an inpatient rehabilitation facility and scheduled for a one-month repeat EGD outpatient.
Discussion: In summary, this case reports a possible and novel association between influenza A infection and the development of acute esophageal necrosis (AEN). While this patient’s history included known risk factors for AEN, including atherosclerosis, DM, and NSAID use, his hospital course strongly suggests that his recent influenza A infection and treatment with oseltamivir may have played a significant role as potential contributors to the development of AEN.
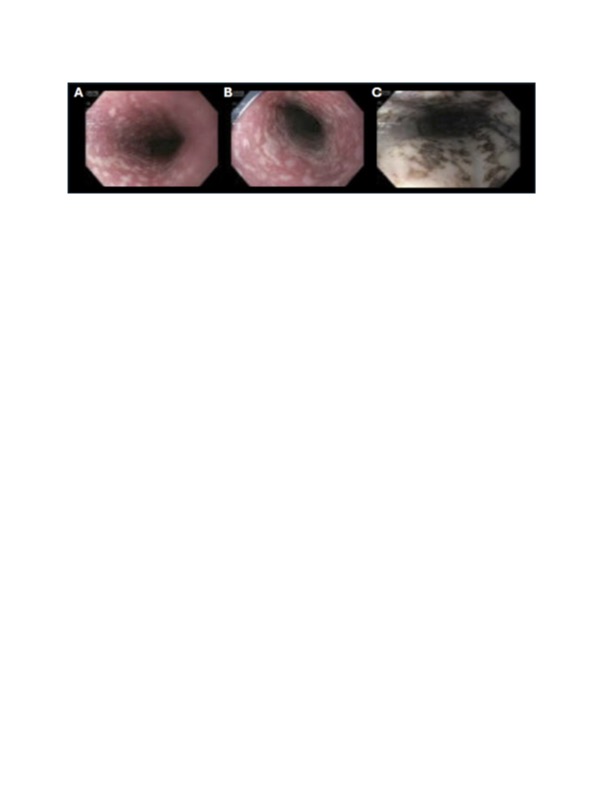
Figure: Figure 1. Upper and middle thirds of the esophagus with esophagitis suspicious for underlying Barrett’s esophagus (A, B). Lower third of the esophagus with circumferential black-appearing esophageal mucosa, characteristic of AEN (C).
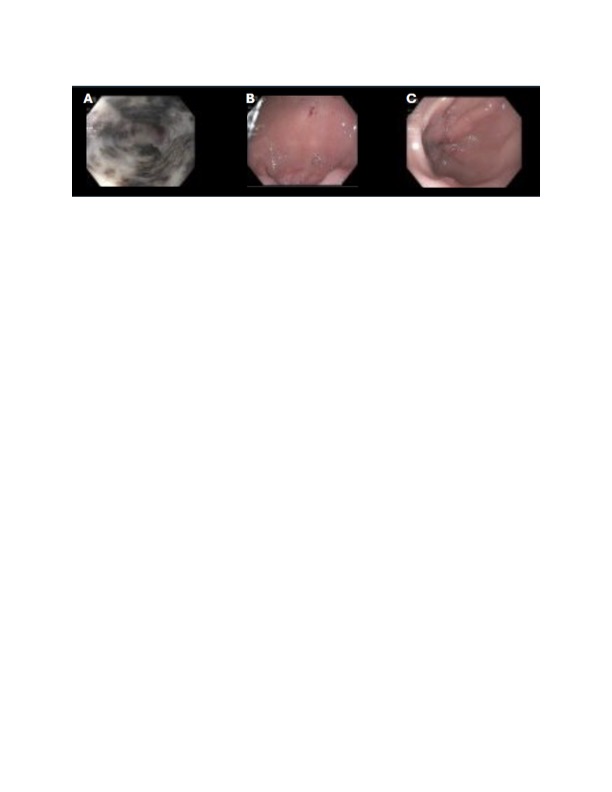
Figure: Figure 2. Gastric cardia with black-appearing mucosa (A) characteristic of AEN, with normal appearing mucosa in gastric fundus (B) and pylorus (C).
Disclosures:
Natalie Rosseau indicated no relevant financial relationships.
Hannah Zuercher indicated no relevant financial relationships.
Marlee Panther indicated no relevant financial relationships.
Katherine Ray indicated no relevant financial relationships.
Ahmed Al Qady indicated no relevant financial relationships.
Amitabh Kumar indicated no relevant financial relationships.
Natalie Rosseau, MD1, Hannah Zuercher, MD1, Marlee Panther, MD1, Katherine Ray, DO1, Ahmed Al Qady, MD2, Amitabh Kumar, MD1. P4993 - Black Esophagus: A Rare Case of Upper GI Bleeding From Acute Esophageal Necrosis in the Setting of Recent Influenza Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
1University of Florida Health Shands Hospital, Gainesville, FL; 2University of Florida, Gainesville, FL
Introduction: Acute esophageal necrosis (AEN) is a rare cause of upper gastrointestinal bleeding (UGIB), defined by circumferential black-appearing esophageal mucosa in the distal esophagus. We present a case of AEN in an immunocompetent patient with type 2 diabetes mellitus, atherosclerotic disease, and recent influenza A infection treated with oseltamivir.
Case Description/
Methods: A male in his seventies with a past medical history of DM, CAD, HTN, and HLD presented with a syncopal episode and a two-day history of hematemesis, melena, and weakness. Upon presentation, he was afebrile with a blood pressure of 94/74. At home, he was on naproxen for osteoarthritis and apixaban for atrial fibrillation. A week prior to this presentation, he was admitted to an outside hospital for respiratory failure secondary to an influenza A infection, which was treated with oseltamivir.
Initial laboratory analysis showed a hemoglobin of 7.8 g/dL from 15.4 g/dL a week prior (normal: 13.0-16.5 g/dL), elevated white blood cell count of 14.3 x10E3/uL (normal: 4.0-10.0 x10E3/uL), and an elevated whole blood lactic acid at 3.1 mmol/L (normal: 0.3-1.5 mmol/L). Computed tomography angiography of the abdomen and pelvis with contrast was unremarkable. He received one unit of packed red blood cells and underwent an urgent upper endoscopy (EGD), which demonstrated Los Angeles (LA) Classification Grade D necrotizing esophagitis (Figure 1, Part C), LA Classification Grade B reflux esophagitis (Figure 1, Parts A and B), and erosive gastropathy (Figure 2, Part C), all without active or recent bleeding. Pathology revealed acute inflammation and ulcer debris, with no evidence of viral or fungal infections.
The patient was treated with an eight-week course of omeprazole 40mg twice daily and a second therapeutic course of oseltamivir. The bleeding ceased, and his hemoglobin levels remained stable. Anticoagulation was resumed after risk-benefit discussion. He was discharged to an inpatient rehabilitation facility and scheduled for a one-month repeat EGD outpatient.
Discussion: In summary, this case reports a possible and novel association between influenza A infection and the development of acute esophageal necrosis (AEN). While this patient’s history included known risk factors for AEN, including atherosclerosis, DM, and NSAID use, his hospital course strongly suggests that his recent influenza A infection and treatment with oseltamivir may have played a significant role as potential contributors to the development of AEN.
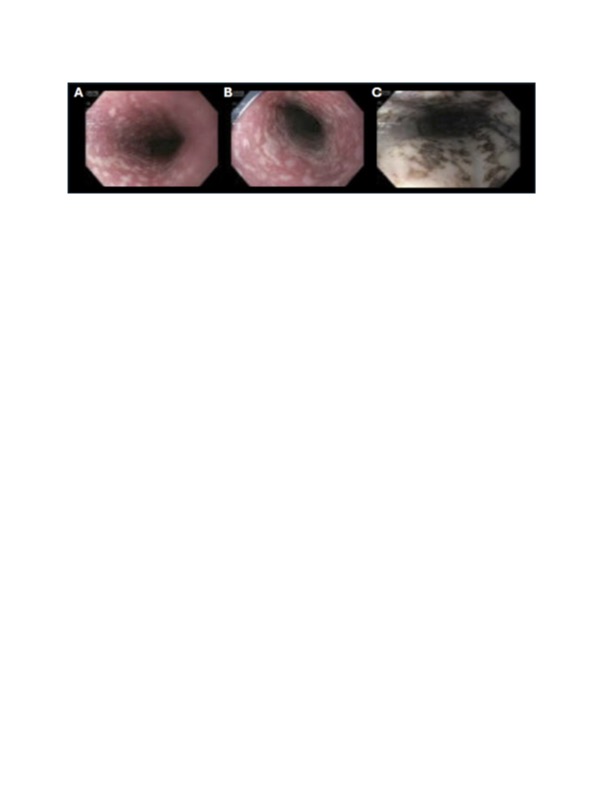
Figure: Figure 1. Upper and middle thirds of the esophagus with esophagitis suspicious for underlying Barrett’s esophagus (A, B). Lower third of the esophagus with circumferential black-appearing esophageal mucosa, characteristic of AEN (C).
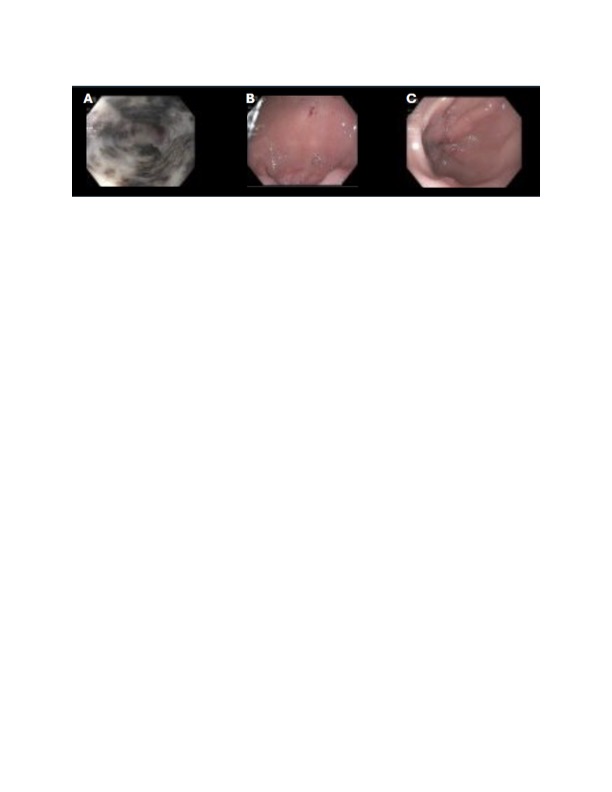
Figure: Figure 2. Gastric cardia with black-appearing mucosa (A) characteristic of AEN, with normal appearing mucosa in gastric fundus (B) and pylorus (C).
Disclosures:
Natalie Rosseau indicated no relevant financial relationships.
Hannah Zuercher indicated no relevant financial relationships.
Marlee Panther indicated no relevant financial relationships.
Katherine Ray indicated no relevant financial relationships.
Ahmed Al Qady indicated no relevant financial relationships.
Amitabh Kumar indicated no relevant financial relationships.
Natalie Rosseau, MD1, Hannah Zuercher, MD1, Marlee Panther, MD1, Katherine Ray, DO1, Ahmed Al Qady, MD2, Amitabh Kumar, MD1. P4993 - Black Esophagus: A Rare Case of Upper GI Bleeding From Acute Esophageal Necrosis in the Setting of Recent Influenza Infection, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
