Tuesday Poster Session
Category: Esophagus
P4992 - When Pancreatitis Turns Black: A Case Report of Acute Esophageal Necrosis
Tuesday, October 28, 2025
10:30 AM - 4:00 PM PDT
Location: Exhibit Hall

Nicole Villa, MD (she/her/hers)
NYC Health + Hospitals/Metropolitan
New York, NY
Presenting Author(s)
Nicole Villa, MD, Julio C. Valencia-Manrique, MD, Gajendra Bham, MD, Carlos Munoz, MD, Jennifer Harley, MD
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Acute Esophageal Necrosis (AEN), also known as “black esophagus,” is a rare but serious condition characterized by circumferential black discoloration of the esophageal mucosa, typically associated with critical illness, hemodynamic instability, and hypoperfusion. We present a case of AEN in the setting of acute gallstone pancreatitis, emphasizing diagnostic challenges and clinical management.
Case Description/
Methods: A 71-year-old woman with a history of hypertension, dyslipidemia, and prior cholecystectomy presented with four days of severe epigastric pain radiating to the back, along with nausea and vomiting. On admission, she was hemodynamically stable, though physical exam revealed marked epigastric tenderness. Laboratory evaluation showed leukocytosis (24,990 cells/mm³), elevated lipase (361 U/L), and a mixed hepatocellular-cholestatic liver enzyme pattern (total bilirubin 2.5 mg/dL, ALT 222 U/L, AST 111 U/L, ALP 170 U/L). Abdominal CT showed peripancreatic fat stranding and a 2.1 cm area of suspected necrosis; chest CT revealed bilateral basal pleural effusions. Magnetic resonance cholangiopancreatography (MRCP) confirmed acute pancreatitis and revealed retained gallstones in the residual gallbladder, along with a dilated proximal common bile duct (8.4 mm) and a filling defect suggestive of choledocholithiasis. During ERCP, the procedure was aborted upon visualization of extensive black, ulcerated esophageal mucosa consistent with AEN. CT angiography ruled out vascular occlusion, and follow-up contrasted CT excluded esophageal perforation. The patient was managed conservatively with intravenous fluids, high-dose proton pump inhibitors, and oral sucralfate. Her condition steadily improved, and she tolerated diet advancement without recurrence of symptoms. Liver enzyme abnormalities resolved, likely due to spontaneous stone passage. A follow-up esophagogastroduodenoscopy (EGD) at three months showed complete healing of the esophageal mucosa.
Discussion: AEN has a multifactorial pathogenesis involving ischemia, acid injury, and systemic insults. While rare, acute pancreatitis may act as a trigger via systemic inflammatory response and compromised esophageal perfusion, particularly in patients with underlying vasculopathy. Prompt recognition, exclusion of complications such as perforation, and early supportive care are essential for favorable outcomes, as demonstrated in this case.

Figure: CT Abdomen revealing significant peripancreatic fat stranding compatible with acute pancreatitis. There is an area of decreased density at the body of the pancreas measuring 3.1 cm, suggestive of necrosis.
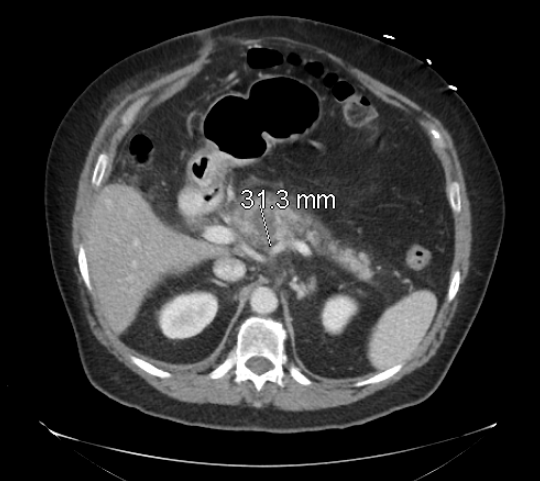
Figure: Upper endoscopy before ERCP showing black necrotic mucosa with confluent and cratered ulcerations scattered in the entire esophagus
Disclosures:
Nicole Villa indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Gajendra Bham indicated no relevant financial relationships.
Carlos Munoz indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Nicole Villa, MD, Julio C. Valencia-Manrique, MD, Gajendra Bham, MD, Carlos Munoz, MD, Jennifer Harley, MD. P4992 - When Pancreatitis Turns Black: A Case Report of Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
NYC Health + Hospitals/Metropolitan, New York, NY
Introduction: Acute Esophageal Necrosis (AEN), also known as “black esophagus,” is a rare but serious condition characterized by circumferential black discoloration of the esophageal mucosa, typically associated with critical illness, hemodynamic instability, and hypoperfusion. We present a case of AEN in the setting of acute gallstone pancreatitis, emphasizing diagnostic challenges and clinical management.
Case Description/
Methods: A 71-year-old woman with a history of hypertension, dyslipidemia, and prior cholecystectomy presented with four days of severe epigastric pain radiating to the back, along with nausea and vomiting. On admission, she was hemodynamically stable, though physical exam revealed marked epigastric tenderness. Laboratory evaluation showed leukocytosis (24,990 cells/mm³), elevated lipase (361 U/L), and a mixed hepatocellular-cholestatic liver enzyme pattern (total bilirubin 2.5 mg/dL, ALT 222 U/L, AST 111 U/L, ALP 170 U/L). Abdominal CT showed peripancreatic fat stranding and a 2.1 cm area of suspected necrosis; chest CT revealed bilateral basal pleural effusions. Magnetic resonance cholangiopancreatography (MRCP) confirmed acute pancreatitis and revealed retained gallstones in the residual gallbladder, along with a dilated proximal common bile duct (8.4 mm) and a filling defect suggestive of choledocholithiasis. During ERCP, the procedure was aborted upon visualization of extensive black, ulcerated esophageal mucosa consistent with AEN. CT angiography ruled out vascular occlusion, and follow-up contrasted CT excluded esophageal perforation. The patient was managed conservatively with intravenous fluids, high-dose proton pump inhibitors, and oral sucralfate. Her condition steadily improved, and she tolerated diet advancement without recurrence of symptoms. Liver enzyme abnormalities resolved, likely due to spontaneous stone passage. A follow-up esophagogastroduodenoscopy (EGD) at three months showed complete healing of the esophageal mucosa.
Discussion: AEN has a multifactorial pathogenesis involving ischemia, acid injury, and systemic insults. While rare, acute pancreatitis may act as a trigger via systemic inflammatory response and compromised esophageal perfusion, particularly in patients with underlying vasculopathy. Prompt recognition, exclusion of complications such as perforation, and early supportive care are essential for favorable outcomes, as demonstrated in this case.

Figure: CT Abdomen revealing significant peripancreatic fat stranding compatible with acute pancreatitis. There is an area of decreased density at the body of the pancreas measuring 3.1 cm, suggestive of necrosis.
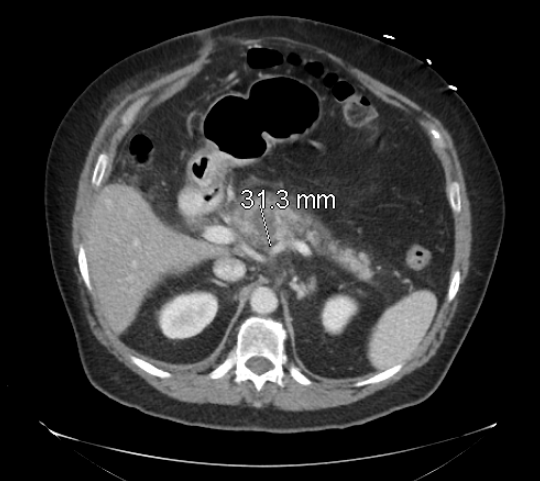
Figure: Upper endoscopy before ERCP showing black necrotic mucosa with confluent and cratered ulcerations scattered in the entire esophagus
Disclosures:
Nicole Villa indicated no relevant financial relationships.
Julio Valencia-Manrique indicated no relevant financial relationships.
Gajendra Bham indicated no relevant financial relationships.
Carlos Munoz indicated no relevant financial relationships.
Jennifer Harley indicated no relevant financial relationships.
Nicole Villa, MD, Julio C. Valencia-Manrique, MD, Gajendra Bham, MD, Carlos Munoz, MD, Jennifer Harley, MD. P4992 - When Pancreatitis Turns Black: A Case Report of Acute Esophageal Necrosis, ACG 2025 Annual Scientific Meeting Abstracts. Phoenix, AZ: American College of Gastroenterology.
